![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
195 Cards in this Set
- Front
- Back
|
Pain-define
|
subjective experience of tissue damage
|
|
|
nociception
|
objective activation of nociceptors by a noxious stimulus
does nto always cause pain |
|
|
3 types of pain
|
nociceptive pain-tissue injury
inflammatory pain- inflammatory mediators activate nociceptors neuropathic pain- damge/misfiring of nervous system |
|
|
What channels mediate mechanical injury?
|
DEG/ENaC
|
|
|
what nociceptors mediate extreme heat pain?
|
TRPV1 (capsaicin of peppers)
cation channels that open in respnse to heat |
|
|
Extreme cold channels?
|
TRPM8
|
|
|
Chelical injury channels?
|
Acid Sensing Ion Channels
|
|
|
Examples of neuropathic pain
|
carpal tunnel
stroke spinal injury |
|
|
Fast pain
-fibers - which nocireceptors -used for? |
-Alphaomega fibers (fast)
-themal and mechanical nocireceptors -what the brain uses to localize pain |
|
|
Slow pain
-fibers -which nocireceptors -used for |
-C fibers (slow)
-polymodal ( many stimuli) -affective, subjective component of pain |
|
|
What is unique about the CNS and nociceptors?
|
it has none
|
|
|
What is hyperalgesia
|
increased sensation of pain to a noxious (harmful) stimulus
|
|
|
What is allodynia
|
increased sensation of pain to an innocuous (harmless) stimulous
|
|
|
Primary hyperalesia allodynia?
Secondary? |
Primary- damage tissue
Secondary- surrounding undamaged tissue |
|
|
When does hyperalgesia/allodynia occur?
|
-Injury= inflammatory mediators= neuropeptides released= mast cell degranulation
|
|
|
Describe pain circuitry
|
1. soma is in DRG
2. pain from skin to lisauer's tract into spinal cord 3. synapse w/ in substantia gelantiosa and nucleus proprius on dorsal horn 4. cross spinal cord 5. proceed up via spinothalamic, spinoreticular, or spinomesencephalic pathway |
|
|
spinothalamic pathway?
|
main pain-sensing pathwya
synapses in VPL of thalamus to S1 |
|
|
spinoreticular pathway
|
minor-pain sensing pathway
from spinal cord to reticular formation of pons Then to thalamus then to S1 |
|
|
spinosemsenphalic pathway
|
pain-modulating pathway, reduces sensitivity to pain
from spinal cord to periaqueductal gray in midbrain tegmentum Then to raphe nucleus of brain stem Raphe nucleus projects down spinal cord to release serotonin on opioid reducing cells in dorsal horn |
|
|
What is used to mock the final step of the spinomesencephalic pathway?
|
morphine
|
|
|
What are the high pain centers?
|
s1 and s2= activate by pain
insula and cingulate cortex= mediate the affective component of pain |
|
|
Where are cholinergic neurons located in the PNS?
|
motor neurons of ventral horm release ACh @ neuromuscular jxn
|
|
|
Where are cholinergic neuros located in the CNS?
|
some brainstem motor nuclei:
-hypoglossal nucleus -dorsal nucleus of vagus- gives rise to preganglionic parasympathetic fibers nucelus basalis of myenert- innervation to cortex (alzheimers) perpendicular tegmental nucleus- innervation to thalamus, involved in sleep Interneurons of basal ganglia |
|
|
What is an interneuron
|
a neuron that provides local signaling w/ in a given brain structure
|
|
|
Features of excitatory synapses
|
1. round vessicles
2. post synaptic density- asymmetric |
|
|
GABAnergic neurons tend to synapse where?
|
on cell bodies, not dendrittes, of their targets
|
|
|
features of inhibitory synapses
|
1. flattened vessicles
2. thin pre and post synaptic densities- symmetric |
|
|
Which GABAnergic neurons are interneurons?
|
GABAergic cells in the cortex
|
|
|
Which GABAergic neurons are projection neurons
|
reticular nucleus of the thalamus- involved in sleep
neurons in the basal ganglia- motor control |
|
|
What are projection neurons
|
nueron that travels outside of structure of origin (opposite of interneuron)
|
|
|
2 areas that release dopamine
|
1. substantia nigra (pars compacta)
2. ventral tegmental area- reward circuitry, schizophrenia associated |
|
|
What is retinal detachment
|
when the neural retina and the pigment epithelium separate
|
|
|
Fxn of cornea
|
main focuser - b/c air and aqueous humor have different refractory indexes
|
|
|
fxn of lens
|
minor focuser- shape changes via ciliary muscles
|
|
|
fxn of iris
|
adjustable for light passage- via iris sphincter muscles
|
|
|
pupil
|
openin of iris, allows light into the eye
|
|
|
anterior posterior champer
|
spaces in fromt of the eye filled w/ aqueous humor
|
|
|
ciliary body , epithelium and muscle fxns
|
epithelium- secretes aqueous humor
muscle- connects to lense via suspensory ligaments |
|
|
What happens when siliary muscle contracts
|
ligaments slacken, lens relaxes and becomes more round, focus on near objects
|
|
|
fxn of canal of schlemm
|
absorb aqueous humor
|
|
|
vitreous humor?
|
fills back of eye
|
|
|
fxn of retina
|
transform light into electrical signals
|
|
|
pigment epithelium
|
support cells of the retina
|
|
|
choroid
|
blood vesels in the back of the eye
|
|
|
fovea
|
area of central vision, high cone density,
pit in the middle fo the macula |
|
|
sclera
|
whites of eyes , continous w/ dura= protection
|
|
|
optic disk
|
exit site for retinal ganglion cells- no photoreceptors
|
|
|
lamina cribosa
|
opening in sclera that allows retinal ganglion cells to exit
|
|
|
optic nerve
|
retinal ganglion cells exiting the eye
|
|
|
subarachnoid space of the eye?
|
surrounds optic nerve and filled w/ CSF
|
|
|
What is paliedema
|
high intracranial pressure puts pressure on CSF,, and there fore the optic nerve, causing nerve to bulge into the eye
|
|
|
Fxn of pigment epithelium
|
support photreceptors:
- absorb photoreceptor outersegments (continously growing) -recycle inactive all-trans retinal to active 11-cis retinal -absorb stray photons- reduce light scattering -secrete fluid into potential ventricular space |
|
|
Inner vs. oouter segment of photoreceptors
|
inner- mitochondria/organelles
outer- modified cilium that contains membranous disks packed w/ photopigment to do phototransduction cascade |
|
|
Which have a higher sensitivity to light, rods or cones?
|
rods
|
|
|
Cones mediate light in low or high light conditions
|
high-light
|
|
|
Photoreceptors: fovea
|
fovea= many cones, few rods
|
|
|
photoreceptors: peripheral retina
|
few cones, many rods
dimness best viewed via peripheral vision |
|
|
on/off channels of retinal carry info about?
|
increments of light/decrements of light
|
|
|
How is the off channel formed
|
ocurs at photo-receptor to bipolar synapse
formed from bipolar cells expresion ionotropic glutamate receptors |
|
|
How is the on channel formed?
|
at photoreceptor-to-bipolar synapse
formed from bipolar cells expressing metabotropic glutamate receptors |
|
|
Off channel preserves/reverse light induced hyper polarization?
|
preserves
|
|
|
on channel preserves/reverse light induced hyperpolarization?
|
reverse
|
|
|
Which cells are the only retinal cells that fire action potentials?
|
Retinal ganglion cells (others use passive)
|
|
|
Define receptive field
|
area of visual space that can affect the firing system
|
|
|
Retinal ganglion cells have what type of receptive fiends?
|
center- surround
|
|
|
With an on- center receptive field: vertical signal
|
from photoreceptor
to ON bipolar cells to ON ganglion cells to generate excitatory center of ON- center receptive fields |
|
|
With an on-center receptive field: lateral signal transmission?
|
from inhibitory horizontal amacrine cells
to vertical circuitry dampens signal |
|
|
With an off- center receptive field: vertical signal
|
from photoreceptors
to OFF bipolar cells to OFF ganglion cells to generate excitatory center of OFF- center receptive fields |
|
|
With an on-center receptive field: lateral signal transmission?
|
from inhibitory horizontal amacrine cells
to vertical circuitry dampens signal |
|
|
P vs. M cell: size
|
P= small
M= big |
|
|
P vs. M cell: amount
|
P= numerous
M= less numerous |
|
|
P vs. M cell: resolution
|
P= high spatial resolution
M= high temporal resoultion |
|
|
P vs. M cells: color?
|
P= color
M= achromatic |
|
|
Are P/M cells bigger in the fovea or the peripheral retina
|
peripheral retina
|
|
|
P and M cells are types of
|
retial ganglion cells
|
|
|
Which layers are displaced in the fovea, why?
|
retinal ganglion cells, inner plexiformlayer, inner nuclear layer
allows light a clearer path to photreceptors |
|
|
fovea mediates ____ vision
|
central
|
|
|
Are there more or less retinal ganglion cells in the fovea or the periphery?
consequence |
more in periphery
in fovea, each retinal ganglion cell receives input from more photoreceptors, allowing better sensitivity to light= better sensitivity, poorer resolution |
|
|
Places where retinal ganglion cells send out put and what do they do
|
superior colliculus- eye movement
suprachiasmatic nucleus of hypothalamus- circadian ruthms lateral geniculate nucleus of thalamus- everyday vision pretectum- pupillary light reflex |
|
|
how does the pretectum work?
|
pupillaru light reflex:
1. input from optic nerve 2. bilateral projection to edinger-westphal nucleus of occulomotor nucleus 3. Edinger westphal nucleus sends projects via the parasympahtetic ciliary ganglion 4. project to iris sphincter muscles 5. close iris sphincter muscle upon light stimulation |
|
|
absent or unilateral light reflex =?
|
damage to mid brain, home of pretectum/endinger-westphal nucleus
|
|
|
Describe the LGN and what happens when light is presented on the left half of visual space.
|
1. light strikes right sides of both retina- 1 nasal, 1 temporal
2. nasal side crosses optic chiasm 3. nasal and temporal join to make optic tract 4. optic tract travel to LGN 5. Info from each eye goes into 1 magnocellular layer (m retinal ganglion cells) and 2 parvocellular years (p retinal ganglion cells) 6. LGN sends out optic radiation that reach primary visual cortex, which lines the calcarine sulcus |
|
|
Fibers of LGN terminate where? what do they do here?
|
in layer 4C of the primary visual cortex
segregate by eye into ocular dominance columns |
|
|
Are cells in V1 monocular or binocular
|
both
|
|
|
what type of cells mediate steropsis?
|
steropsis= depth perception
binocular cells |
|
|
binocular cells are in which layers of V1?
|
higher : 1-4b
|
|
|
orientation cells are in which layers of V1?
|
higher: 1-4b
|
|
|
What are simple cells?
|
orientation selective
must be in proper receptive field |
|
|
what are complex cells?
|
orientation selective: orientation is all that matters
|
|
|
This in upper left visual space are represented where?
|
bottom right part of calcarine sulcus
|
|
|
which part of the brain represents central vision?
|
occipital pole- very tip of occipital lobe
|
|
|
When are lesions often macular sparing? why?
|
when they are in or near V1
central vision is everywhere in V1- 1 lesion rarely knocks it all out 2. occipital pole gets 2 blood supplies- compensation |
|
|
Structures optic tract is next to, moving posteriro
|
hypothalamus
3rd ventricle/basal ganglia internal capsule terminate in LGN |
|
|
The LGN contains ___ parvocellular layers, populated by ___ cells
|
4
sma;; p cells |
|
|
The LGN contains ___ magnocellular layers, populated by ___ cells
|
2
large M cells |
|
|
The LGN separates magnocellular and parvocellular layers w/ ____ layers which contain ___ and ___ cells
|
interlaminal layers
white matter (in and out going) K cells- receive input from K retinal ganglion cells |
|
|
V1 has more or less layers than the standard 6 cortical layers? why?
|
more
layer 4 expand s into sublyaers |
|
|
what is the stria of Gennari?
|
layer 4b of V1, light in color
|
|
|
Define hierachcial organization
|
early stages= simple feature cells
later stages= complex features |
|
|
topographic mapping
|
maintained at high levels such that each section has a map of visual space
|
|
|
Propertiesof higher layers of V1/V2?
|
1. first to show binocular response (combined inputs from left/right ocular dominance columns)
2. orientation selectivity 3. form blob-interblob columns |
|
|
what stains for blob- interblob columns?
|
cytochrome oxidase
|
|
|
blobs?
|
high color sensitivity, low orientation selectivity
|
|
|
interblobs
|
low color sensitivity
high orientation selectivity |
|
|
modules of V1 have
|
1. 100k neurons
2. 1 full set of orientation columns 3. 1 pair of ocular dominance columns, and one pair of blob/interblobs |
|
|
V2 recieves input from?
|
V1
|
|
|
cytochrome oxidase staining pattern of V2?
|
thick stripes
interstripes thin stripes |
|
|
2 visual processing streams?
|
ventral-what (respond to complex objects such as faces)
dorsal stream-where (respond to motion in a preferred direction) |
|
|
Ventral stream
-info comes from -travels to - type of info |
- P-type retinal cells (high spatial resolution and color sensitivyt)
- goes to V4 and then inferotemporal cortex -what (i.e. complex objects) |
|
|
dorsal stream
-info comes from -travels to -type of info |
-M-type retinal ganglion cells
--area MT and the posterior parietal cortex -where (respond to motion in a preffered direction) |
|
|
CNS development involves an ___ of neurons, many of which are fated to___
|
excess
die by apoptosis |
|
|
How are excessive synapses tuned down to give the right final pattern of connections?
|
endogenous/exogenous activity of the circuit
only connections to receptive neurons will survive |
|
|
in general activity-___ development helps forms the basic architecture of the nervous system
|
independent
|
|
|
formation of fovea: activity-dependent or independent
|
independent
|
|
|
migration of neurons to their correct location: activity-dependent or independent
|
independent
|
|
|
What is the reeler mutant?
|
mutation of reelin, which is used in radial migration, that causes an inversion of the cortical layers
|
|
|
mutations in doublecortin cause?
|
doublecortin lissencephaly= thick cortex, packed w/ too many cells
|
|
|
abnormal basal lamina causes?
|
cobblestone lissencephay= brain spills out of a patch basal lamina
|
|
|
What is an example of endogenous activity? describe
|
retinal waves- spontaneous firing of retinal ganglion cells to carry them to the LGN (layers)
also carry from LGN into V1 (formation of occular dominace columns |
|
|
formation vs. maintenace of occular dominance columns
|
formation- endogenous activity (retinal waves
maintenance- exogenous activity (visual experience) |
|
|
What happens if only one eye gets input?
|
deprived eye's occular dominance column will be taken over by the non-deprived eye
loss of stereopsis (depth perception) |
|
|
Is occular dominance column wiring permanent?
|
no- if the column is taken over, visual system is plastic allowing it to go back to normal if eye deprivation is fixed
must occur during the critical period (2 years) |
|
|
being cross-eyed can lead to?
|
loss of depth perception (steropsis) due to the uncorrelated info from both eyes
|
|
|
__% of synapses in visual cortex turn over each week?
|
10
|
|
|
CSF flow depends on
|
1. rate of CSF production
2. Rate of CSF absoprtion 3. Ciliary action of ependymal cells (epithelial cells lining ventricles) |
|
|
rate of CSF absorption is determined by?
|
pressure difference between CSF and venous system
|
|
|
volume, turnover, color of CSF
|
150-250 mL
4 x per day clear- no cells |
|
|
Structure of chorid plexus
|
vascular core surrounded by epithelial cells w/ tight jxns forming blood-CSFbarrier
|
|
|
Steps of CSF production
|
1. vascular core of chorid plexus
2. recieve filtrate from capillaries to epithelial cells 3. epithelial cells absorb filtrate 4. epithelial cells secrete Na, Cl, HCO3 into ventricular space, water follow 5. CSF is produced/secreted |
|
|
what makes HCO3 for CSF production?
|
carbonic anhydrase
|
|
|
What effect does intracranial pressure have on CSF production?
|
none
|
|
|
What effect does intracranial pressure have on CSF resportion?
|
increass it by forcing more CSF into venous drainage
|
|
|
Causes of hydrocephalus?
|
1.non-communicating- blocking ventricular system by tumors
2. communicating- reduced absorption due to infection/problem w/ arachnoid granulation 3. tumors of choroid plexus causing excess CSF prodution |
|
|
Treatment for hydropephalus
|
1. carbonic anhydrase inhibitor (dec. CSF production)
2. ventriculostom (drain ventricle out of skull) 3. ventriculoperitoneal shunt (drain ventricle to gut) |
|
|
3 things that form blood brain barrier
|
1. tight jxns btwn endothelial cells
2. pericytes 3. astrocyte endfeet |
|
|
How do molecules cross the BBB?
|
1. transport proteins from endothelial cells
2. transocytosis- endothelial cells take in large molecules by endocytosis 3. being liphophilic |
|
|
BBB may be distrupted during
|
pathological states: infection, hypoxia
|
|
|
normal value for CBF?
|
50ml/100g/min or high
|
|
|
CBF=
|
CBF=CPP/CVR (perfusion pressure over resistance)
CPP= (MAP-ICP) (arterial pressure- intracranial pressure) |
|
|
What increases CBF?
|
paCO2
serum H dilates vesselsof the brain- so during anerobic conditions brain can get more oxygen |
|
|
What decreases CBF?
|
paO2- constricts vessels of the vein, alleviating some of the ressure
|
|
|
Hyperventilation and CBF?
|
hyperventilation= increased paO2= vessels constrict= lower BF=lower intracranial pressure
|
|
|
diminshed vision in part of visual field?
|
central cotoma
|
|
|
loss of half of visual field
|
hemianposia (can be bitemporal- both eyes, can be homonymous- same in both eyes)
|
|
|
Which arteries supply the occipital lobe?
|
posterior cerebral artiers, from basilar artery
|
|
|
what could cause hypoxic damage to right v1? what would this cause
|
blocking right posterior cerebral artery
left homonymous heimanopsia |
|
|
|
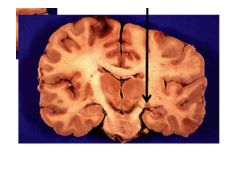
Globus pallidus
|
|
|
diminshed vision in part of visual field?
|
central cotoma
|
|
|
loss of half of visual field
|
hemianposia (can be bitemporal- both eyes, can be homonymous- same in both eyes)
|
|
|
Which arteries supply the occipital lobe?
|
posterior cerebral artiers, from basilar artery
|
|
|
what could cause hypoxic damage to right v1? what would this cause
|
blocking right posterior cerebral artery
left homonymous heimanopsia |
|

|
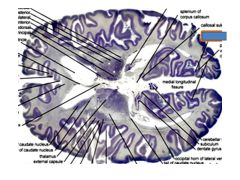
globus pallidus
|
|

|
Anterior commisure
|
|

|
putamen
|
|

|
caudate
|
|
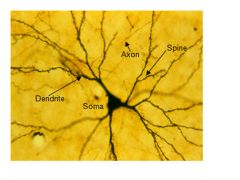
What type of neuron is this?
|
Glutamatergic (pyramidal neuron)
Make glutamine |
|
What type of nt does this make?
|
Substantia nigra- dopamine
|
|

Name, fxn, level, projection
|
Locus ceruleus, makes noradrenaline, located at the level of pons
Project to the cortex |
|
Name, fxn, projection
|
Ralphe nucleus, makes serotonin, project to cortex and spinal cord (decreased sensitivity to pain)
|
|

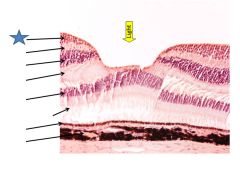
Fxn
|
Photoreceptor outer segments
Contain photopigment, convert light into electrical signals |
|

Fxn
|
Outer plexiform layer
Connection btwn photoreceptors and bipolar/horizontal cells |
|

Fxn
|
Inner plexiform layer
Connections between bipolar/amacrine cells and retinal gangglion cells |
|

Fxn
|
Retinal ganglion cells
Output cells of the retina, axons make up optic nerve CII |
|

Fxn
|
Pigment epithelium
Supports photoreceptors |
|

Fxn
|
(potential) ventricular space)
Where retinal distachment occurs |
|
|
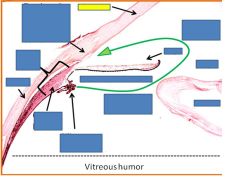
cornea
|
|
|
Ciliary body
|
|
|
sclera
|
|
|
Ciliary muscle
|
|
|
Ciliary epithelium
|
|
|
Posterior chamber
|
|
|
iris
|
|
|
pupil
|
|
|
lens
|
|

|
lens
|
|
|
Retinal ganglion cells
|
|
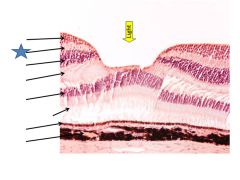
|
Inner plexiform layer
|
|
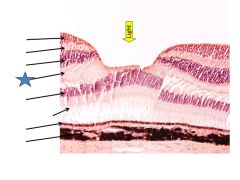
|
Outer plexiform layer
|
|
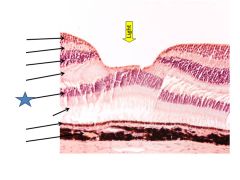
|
Outer nuclear layer
|
|
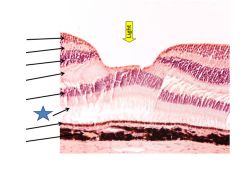
|
Photoreceptor outer segments
|
|
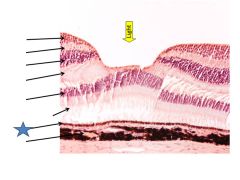
|
Pigment epithelium
|
|
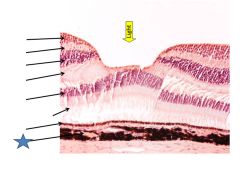
|
choroid
|
|
|
Defect in one eye= of the optic nerve- not crossed yet
|
|
|
Tunnel vision= lesion of optic chiasm
Nasal retinas are damaged= can’t capture light from periphery |
|
|
Symmetric deficit= lesion in optic tract on opposite side of where you can’t see and beyond
Nasal retina fibers have crossed over |
|

|
Upper left visual field of both eyes= lesion of lower right optic radiation
|
|

|
Defect of both upper left visual fields, macular sparing= lesion to lower right calcarine sulcus
|
|
|
LGN
|
|
|
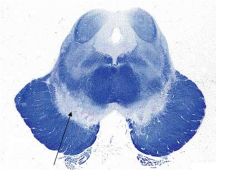
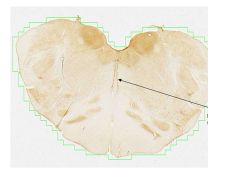
1= parvo layer of LGN
2= magno layer of LGN |
|
|
1= parvo layer of LGN
2=interlaminar layer of LGN 3= magno layer of LGN |
|

Fxn
|
Superior colliculus- eye movements
|
|

fxn
|
Pretectum= pupillary light reflex
|
|

fxn
|
LGN-sends visual info to primary visual cortex (V1)
|
|
|
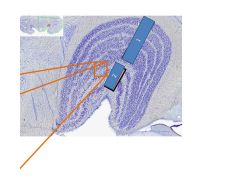
Calcarine sulcus
|
|
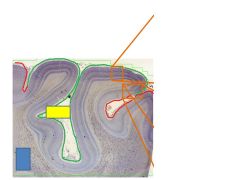
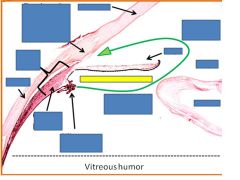
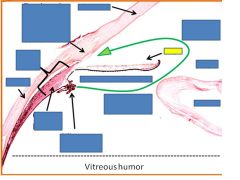
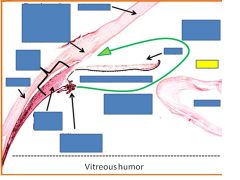
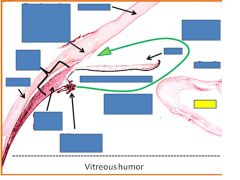
Red?
Green? Yellow box? |
V2
V1 Calcarine sulcus |

