![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
4 divisions of the diencephalon
|
- Hypothalamus
- Subthalamus - Epithalamus - Dorsal Thalamus THALAMUS |
|
|
|
Anterior Nucleus
|
PAPEZ CIRCUIT:
Mammillary bodies to Anterior Nucleus to Cingulate Gyrus to Hypocampus to Fornix to Mammillary Bodies {Learning/Memory: Anterior cingulated gyrus} |
|
|
|
Dorsomedial nucleii
|
Connected to Frontal Lobe
{Connects Limbic areas: Prefrontal cortex} |
|
|
|
Ventral Anterior nucleii
|
{Premotor}
|
|
|
|
Ventral Lateral
|
{M1. Primary motor cortex}
|
|
|
|
Ventral Posterior Nucleii
|
1) VPL: from trunk/limbs via Spinothalmic and Medial Lemniscus
2)VPM: from Trigeminal {Somatosensory input} |
|
|
|
Medial Geniculate
|
{Auditory input: A1}
|
|
|
|
Lateral Geniculate
|
{Vision: V1}
|
|
|
|
Motor Nucleii
Somatosensory PTO Cortex |
Motor Nucleii : VA, VL
Somatosensory: VPL, VPM PTO Cortex: Pulvinar |
|
|
|
Subcortical nucleii
|
Have NO CORTICAL PROJECTIONS (project back to other thalmic nucleii)
|
|
|
|
Thalamus irrigated by
|
1) Thalamoperforating a.
2) Thalamogeniculate a. 3) Posterior choroidal aa. {HTN>Contralateral hemiplegia} |
|
|
|
Internal capsule irrigated by
|
1) Lenticulostriate a. {HTN>Contralateral hemiplegia}
2) Medial striate a. (from ACA) 3) Anterior choroidal (from MCA) |
|
|
|
VPL/VPM Lesion
|
Contralateral Somatosensory disturbance
|
|
|
|
LGN lesion
|
Contralateral Visual field defects
|
|
|
|
VA/VL lesion
|
Disturbances in motor control
|
|
|
|
Pulvinar lesion
|
Visual-spatial, perceptual, language disturbances
|
|
|
|
Anterior nuc. lesion
|
Memory loss
|
|
|
|
DM nuc. lesion
|
Executive or frontal lobe deficits
|
|
|
|
Intralaminar nuc. lesion
|
Attention/arousal deficits
|
|
|
|
Multiple nucleii lesion
|
Neglect
|
|
|
|
Ventral posterior nuc. lesion
|
Dejerine-Roussy Syndrome
Sx: Feeling lingering pain after $ removed. Minor $ can cause stron and persistent pain |
|
|
|
Function of THALAMUS
|
Funnels through all sensory input (except olfactory sense)
SELECTIVE ATTENTION, thalamus prioritizes what is important |
|
|
|
Four subtypes of cortical architecture
|
"CAMI"
1) Corticoid 2) Allocortex 3) Mesocortex 4) ISOCORTEX |
|
|
|
Isocortex
|
- 6-layered neocortex
- 2 subtypes + Idiotypic/Heterotypic: Layers diff to differentiate > Granular (sensory cortex) > Agranular (Motor cortex-pyramids) + Homotypic: Easier to differentiate > Posterior * Unimodal 2* * Heteromodal 3* > Frontal |
|
|
|
6 Layers of Isocortex
|
1) Molecular: acellular
2) External granular: 3) External pyramidal 4) Internal granular: TERMINATION OF PRIMARY THALAMIC INPUTS 5) Internal pyramidal 6) Multiform (polymorphic) |
|
|
|
Brodmann's Areas
|
S1 - 3, 1, 2
S2 - 5, 7 M1 - 4 M2 - 6 A1 - 41, 42 A2 - 22 V1 - 17 V2 - 18, 19 |
|
|
|
3 types of cortical pathways
|
"ACP"
1) Association 2) Commissural 3) Projection |
|
|
|
Association pathways
|
>Within same hemisphere
>(1) Arcuate fasciculus: frontal cortex to superior temporal cortex {ant & post speech} >(2) Cingulum: septal frontal lobe to cingulated/parahippocampal gyrus {limbic} |
|
|
|
Commissural pathway
|
>Left hemisphere to right
> {Spatial info} > Ex: Corpus collosum |
|
|
|
Projection pathways
|
>Up and down cortex to non-cortex
>(1) Internal capsule: Corticobulbar/spinal/pontine >(2) Optic radiations: Geniculocortical fibers |
|
|
|
Watershed/Border zone
|
Anastomosis between ACA and MCA in medial frontal and parietal lobes
LESION: Nebulous cortical probs like diff calculating and reading (no motor deficits) |
|
|
|
ACA irrigates
|
Medial frontal and parietal lobes
|
|
|
|
MCA irrigates
|
Runs in lateral sulcus; supplies lateral frontal, parietal, and temporal lobes
|
|
|
|
PCA irrigates
|
Occipital lobe, part of inferior temporal lobe
|
|
|
|
Triune Brain
|
1) Posterior cortex: Info gathering, processing, integration
2) Frontal lobe: Executive, decision making 3) Hypothalamus/limbic: Emotion/motivation |
|
|
|
Lesion to primary posterior cortex
|
No sensory deficits
|
|
|
|
Cannot recognize objects.
Can open door when given key but doesn't know what it is |
Lesion to secondary posterior cortex
|
Apperceptive agnosia
|
|
|
Lost ability to associate things with multiple concepts.
Knowing what a hat looks AND feels like. |
Lesion to tertiary posterior cortex
|
Associate agnosia
|
|
|
Left frontal cortex
|
Speech, motor skills
|
|
|
|
Right frontal cortex
|
Emotion, expression, perception, social skills
|
|
|
|
Inability to recognize own fingers
|
Lesion of left angular gyrus
|
Gerstmann's Syndrome
|
|
|
Pt. unaware of own disease/deficit
|
Ansognosia
|
|
|
|
Pt. cannot name colors, cannot read, can see in ipsilateral visual field and can write
|
Lesion to left or right PCA>damaging ipsilateral occipital lobe and ipsilateral corpus callosum
|
Alexia (without agraphia)
|
|
|
Inability to carry our a discrete previously learned movement
"How do you use a hammer?" |
Lesion to supramarginal gyrus, arcuate fasciculus, left premotor area > bilateral deficit
Also from injury to corpus collosum or right premotor area > left side deficit only |
Ideomotor apraxia
|
|
|
Pt can speak but cannot repeat things. Difficulty naming objects, reading aloud, writing, and occasionally will substitute sounds for words
|
Disconnection between Broca's (speaking) & Wernicke's areas (comprehension)
|
Conduction aphasia
|
|
|
MRI of swiss cheese brain
|
Arteriovenous malformation, no Sx. other than headaches and seizures
|
|
|
|
MRI with giant fucking cyst
|
Subarachnoid cyst
|
|
|
|
Three types of headaches
|
1) Tension
2) Cluster 3) Migraine >With/Without Aura |
|
|
|
Tension Headaches
|
> Most common
> Head in vise > 30 min to 7 days > Chronic if >15days over one month |
Tx: Stress relief
Chronic >NSAIDS, >ASA-Caffeine-Bulbital (barbituate!) >Phenacetin also >Anti-depressants >Muscle relaxant |
|
|
Cluster Headaches
|
>Severe unilateral pain in and around orbit
>Icepick into face >15 min to 2 hours |
Tx:
>Pure oxygen >5-HT agonists (serotonin agonists) >Intranasal lidocaine also >Ca++ channel blockers >Bellergal >Lithium >Steroids >Antihistamines |
|
|
Migraine Headaches
|
>Unilateral
>Pulsation rather than icepick stab >Females experience more >Peak between 30s and 50s >Can present with anorezia, nausea, vomiting (and photo- and phono-phobia) |
Tx
ACUTE >Analgesic, triptans (serotonin agonists) PROPHYLACTIC >Antiepileptics >Beta-blocker >Antidepressant BEHAVIORAL >Limiting caffeine/stress >Inc exercise >Sleep |
|
|
Migraine stages
|
Prodrome
Aura Headache Postdrome |
|
|
|
Three theories of migraine causes
|
1) Spreading wave: Brainstem to cortex like epileptic seizure
2) Trigeminal: Efferent vasospasms (why serotonin agonists work) 3) Allodynia theory: Hypersensitivity |
|
|
|
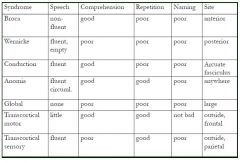
Memorize syndrome chart:
BROCA WERNICKE CONDUCTION ANOMIA GLOBAL TRANSCORTICAL (Motor&Sensory) |
|
|
|
|
Irrigation to language part of brain
|
MCA
|
|
|
|
Left M1 loss yields...
|
Loss of entire left side of brain
>Contralateral hemiplegia and sensory loss > Homonymous hemianopia >Eye deviation toward affected side >Global aphasia (if left) > >Neglect and Anosognosia (if right) |
|
|
|
M2 loss yields...
|
>Eye deviation
>Contalateral motor loss >Broca's aphasia |
|
|
|
ACA problems
|
Echolalia: Pt repeats back what you said to them
|
|
|
|
Parts of Frontal lobe
|
1) Superolateral cortex
2) Orbitofrontal area |
|
|
|
Superolateral cortex
|
>Executive center
>Working memory/Scratchpad >Processes things >Only area to produce actions without external $ -X- Pathological inertia >Can't move from one task to another without a $ >Easily distracted |
|
|
|
Orbitofrontal cortex
|
>Prone to injury from falls
>Center of social self >Inhibits impulses that are socially unacceptable "Oh Fuck" - OF |
|
|
|
Types of Memory
|
1) Immediate
2) Short term 3) Recent 4) Remote |
|
|
|
Memory pathway
|
>Sensory memory
+Attn or +Forget >Working memory +Encode or +Forget >Longterm memory +Declarative (facts_ *Semantic (knowledge,meaning) *Episodic (events,times,places) +Procedural (skills) |
|
|
|
Constructional ability
|
Ability to reproduce drawings (right brain)
|
|
|
|
Abstract reasoning
|
Math, proverbs, similarities/differences
|
|
|
|
Apraxia
|
Manifestation of dysfxn in multiple areas. Inability to do somethin on command
|
|
|
|
Neglect
|
Usually right brain problem (and neglect left side)
|
|
|
|
Types of neglect
|
>Hemibody
>Motor >Sensory >Visual >Auditory |
|
|
|
Lesion to dominant angular gyrus
|
>Gerstmann's Syndrome
>MCA dz. |
|
|
|
Acalculia
|
Can't calculate
|
|
|
|
Agraphia
|
Can't write sentence
|
|
|
|
Finger agnosia
|
Don't know which finger is ring finger
|
|
|
|
R/L Confusion
|
Can't determine which is R or L
|
|
|
|
R frontal eye field drives eye to _____
|
Left
Eye looks to side of destruction |
|
|
|
PCA dz.
|
Can write but not read
|
|
|
|
Three things to look for in a neurological exam
|
1) Localize the lesion
2) Determine the tempo (onset/duration) 3) Get demographics (exposure, hazards to help Dx) |
|
|
|
Two pathological processes that can impair consciousness
|
1) Bilateral cerebral hemisphere dysfxn
2) Rostral brainstem-thalmic dysfxn in >Diencephalon >Midbrain >Rostral pons >Disruption os ARAS (ascending reticular activating system) {Consciousness, sleep/wake cycles} |
|
|
|
Delirium
|
>Acute onset, fluctuating course
>Impaired attn and arousal >Agitated/altered sleep cycle Dementia is more global |
|
|
|
Delirium risk factors
|
SHE DIES
I WATCH DEATH [Seizure, hemodynamic, endocrine, drugs, infection, electrolytes, stroke] [Infections, Withdrawal, acid/base disturbance, trauma, CNS pathology, hypoxia, deficiency in vitamins, endocrinopathies, acute vascular, toxins/drug, heavy metals] |
|
|
|
Pupillary response in CN exam (Symp vs Parasymp)
|
Pupillodilator - Symp damage causes constricted pupil and ptosis (like horner)
Pupilloconstrictor PS damage causes unreactive dilated pupil >Uncal herniation |
|
|
|
Sluggish light reactivity retained until all other brain stem reflexes lost
|
Diffuse cellular cerebral dysfxn (toxic-metabolic encephalopathy)
|
|
|
|
Unilateral papillary dilation, pupil unreactive to light
|
3rd CN compression (like transtentorial herniation) usually due to ipsilateral lesion
|
|
|
|
Pupils fixed in midposition
|
Midbrain dysfxn due to structural damage (infarction, hemorrhage)
Central herniation Prolonged metabolic depression by drugs or toxins |
|
|
|
Pupils tiny (1mm wide)
|
Massive pontine hemorrhage
Toxicity due to opoids or certain insecticides (organophosphates, carbamates) |
|
|
|
General CN by test
Ocular mvmt Facial grimacing Corneal reflex Gag reflex |
General CN by test
Ocular mvmt [3, 4, 6] LR6SO4R3 Facial grimacing [5, 7] Corneal reflex [5, 7] Gag reflex [9, 10] |
|
|
|
Doll's eyes
|
Oculocephalic reflex
If absent eyes stay static |
|
|
|
Calorics
|
Oculovestibular reflex
Cold water turns eyes away Warm water attracts |
|
|
|
Arms flexed and legs extended
|
Decorticate rigidity, problem above midbrain
|
|
|
|
Arms and legs extended
|
DEcErEbratE rigidity, prob at or below midbrain
E - all limbs ExtEntEd |
|
|
|
Compartments of cranial vault, must be balanced to maintain intercranial pressure
|
Monroe-Kellie Doctrine
1) Parenchyma (80%) 2) CSF (10%) 3) Blood (10%) |
|
|
|
**Cerebral perfusion pressure eqn (CPP)
|
CPP = Mean art press - Intercranial press
CPP = MAP - ICP |
|
|
|
**Uncal herniation
|
From high to low pressure
Uncus and/or hippocampus shifts from Middle cranial fossa to posterior fossa. Compression of ipsilateral CN3, contra CN2, and mesencephalon |
|
|
|
Uncal herniation stages
|
1)Early: drowsy/sluggish
2)Herniation of midbrain/poins: coma, babinski 3)Later herniation of medulla (IRREVERSIBLE) |
|
|
|
Persistent vegetative state
|
No awareness, communication, response to $, voluntary mvmt, control
|
|
|
|
Locked in syndrome
|
Due to basilar artery thrombosis
Awake and alert but tetraplegic, can only blink RAS and oculomotor nerve fine but other motor (cortico____ not) |
|
|
|
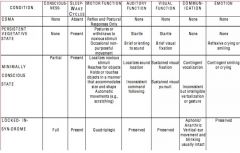
Mental status chart:
COMA PVS MinCS LIS |
|
|
|
|
Brain death
|
Loss of fxn of entire cerebrum and brain stem, resulting in coma, no spontaneous respiration, loss of ALL BRAINSTEM REFLEXES (some spinal reflexes such as deep tendon, plantar flexion, and withdrawal remain)
No recovery. Core temp will be more than 32C |
|
|
|
How to confirm brain death
|
Must confirm absence of brain stem reflexes
>Pupils don't respond to brigh light >No oculocephalic reflex >No oculovestibular reflex >No corneal reflex >No grimacing due to pain > No jaw jerk >No cough response to bronchial suctioning |
|
|
|
Only fibers from the _____ project directly into the thalamus
|
Spinothalmic (duh, look at the name)
|
|
|
|
What are the three somatosensory systems
|
1) DCMLS (M>L as ^) foot is medial {VPL}
2) Trigeminal 3) ALS (L>M as ^) foot is lateral {VPL} |
|
|
|
Loss of discrimination in
>3B >1 >2 |
>3B: severe deficit in texture and shape discrimination
>1: Deficit in texture disc >2: Deficit in Finger coordination, shape, and size discrimination |
|
|
|
Receptive field and what determines amount of discrimination
|
A single neuron area
Size and density as well as contrast (affected by lateral inhibition) |
|
|
|
The fastest most dense sensory pathway to the cortex is _______
|
ML
|
|
|
|
The four fundamental properties for a $
|
"MIDL"
1)Modality: Class of $ (Touch,temp,pain) 2)Intensity 3)Duration 4)Location All affect RECRUITMENT |
|
|
|
Modalities and type of receptor
MR. PM |
|
|
|
|
Modalities and Receptor types
|
MR.PM
|
|
|
|
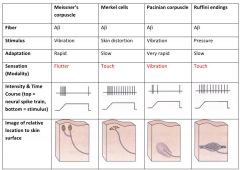
Dynamic/fast adapting receptors
|
Pacinian corpuscles and Meissner
LOW freq, discontinuous APs |
|
|
|
Slowly adapting receptors
|
Merkel cells and Ruffini ends
HIGH freq, continuous APs |
|
|
|
Thermoreceptors
|
"Combo"
Adapt quickly then fire steady state APs for entire duration of temperature stimulus |
|
|
|
Nociceptors
>Types of fibers |
A-delta: myelinated, fast pain, localized, sharp {mechanosensitive, mechanothermal}
C fibers: nonmyelin, slowpain, diffusem aggravating |
|
|
|
Encapuslation effects
|
WITH: receptor potention only when skin undergoes change (rapidly adapting)
WITHOUT: slowly adapting receptor |
|
|
|
Basal Ganglia functions
|
1) Preparation
2) Smooth transitioning 3) Inhibiting 4) Monitoring 5) Initial learning 6) Adapting |
|
|
|
Basal ganglia derived from ______
|
Telencephalon
|
|
|
|
Basal ganglia comprised of
|
Caudate
Globus pallidus Putamen (all together considered Corpus striatum) Last two are lentiform/lenticular nucleus |
|
|
|
Excitatory NT
Inhibitatory NT |
+Glutamate
-GABA |
|
|
|
Receiving Nucleii
|
Caudate and putamen
|
|
|
|
Processing nucleii
|
GPe and subthalmic nucleus
|
|
|
|
Output nucleii
|
GPi and SNr
(SNc - mixed fxn nucleus) |
|
|
|
MOTOR LOOP
|
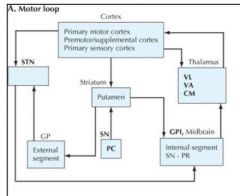
|
|
|
|
LIMBIC LOOP
|
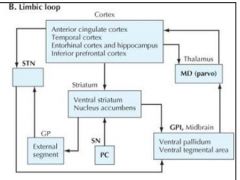
|
|
|
|
COGNITIVE LOOP
|
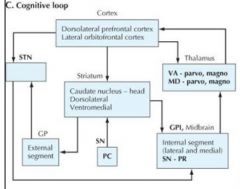
|
|
|
|
OCULOMOTOR LOOP
|
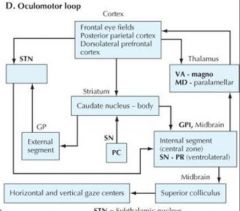
|
|
|
|
Blood supply to basal ganglia
|
>Lenticulostriate (from M2 of MCA)
>Medial striate aa. >Ant. choroidal aa. |
|
|
|
Motor basal ganglia disorders
|
Hypokinetic: Parkinsons, prob direct system
Hyperkinetic: Huntington's prob of indirect inhib system |
|
|
|
Parkinson's disease
|
> degen of SNc
> less dopamine (which inhib inhib paths, if less would inhib) |
|
|
|
Huntington's disease
|
>Striatum diminished cap to inhib GPe, less inhibition of thalamus, increasing unwated cortical activatio
|
|
|
|
Hemiballism
|
Lesion of subthalamus (stim inhib GPi in thalamus)
Yields excessive cortical activation |
|

