![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
7 Cards in this Set
- Front
- Back
|
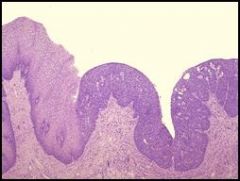
• This is the next step toward neoplasia. The cells toward the bottom are nucleated and proliferating. The cells lose their nuclei and flatten as they move up to the surface where they will slough off.
• There is normal cervical squamous epithelium at the left, but dysplastic squamous epithelium at the right. The displastic tissue has dark nuclei seen in all layers, and moving toward the surface they do not lose their nuclei or assume the flattened morphology. (@ a higher magnification you would see larger nuclei & less cytoplasm comparative to normal cells. You might also see increased mitotic figures indicating actively proliferating tissue.) • Dysplasia is a disorderly growth of the epithelium, but it is still confined to the epithelium. • Dysplasia is reversible. • This figure is full-thickness dysplasia that extends through the entire epithelia layer. • Dysplasia can be classified as mild, moderate, or severe depending on the extent of tissue involvement. • This type of cervical dysplasia is also called carcinoma in situ. |
Describe
|
|
|
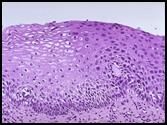
• High magnification cervical dysplasia.
• Note nuclear changes (black dots). In normal epithelium, the cells lose their nuclei or assume a flattening morphology as they move to the top of the epithelial surface). • These dysplastic cells maintain their nuclei as they move to the top. The nucleus: cytoplasm ratio has increased, and there are morphological irregularities in the nuclear membrane. |
Describe
|
|
|
• Gross specimen of Cervical Carcinoma.
• Squamous cell neoplasms are often bulky & irregular, like this gross specimen. • This is a neoplasm. Neoplasia is uncontrolled new growth. Note the mass of abnormal tissue on the surface of the cervix. The term “tumor” is often used synonymously with neoplasm, but a “tumor” can mean any mass effect, whether it is inflammatory, hemodynamic, or neoplastic in origin. • Neoplasms are NOT reversible. • A large tumor can start outpacing its blood supply, leading to necrosis & hemorrhage that would (in this case) present as vaginal bleeding or discharge. A patient might also experience pain on intercourse. This can occur in anyone, but is most common in middle age to older women. |

Describe
|
|
|
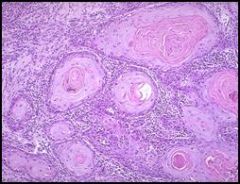
• Squamous Cell Carcinoma of the Cervix.
• If dysplasias are left to their own devices, the neoplastic cells will break through the basement membrane and invade the connective tissue, forming nests of keratin. • The cells are still epithelial in nature, with well-defined cell borders and producing keratin. Because this is morphologically still an epithelial cell, this is a well-differentiated squamous cell carcinoma. • The nucleated cells (dark) in between the keratin nests are largely lymphocytes that mediated the inflammatory response in response to the carcinoma. • Treatment: surgical followed by chemo or radiation. |
Describe
|
|
|
• Multiple Adenomatous polyps of the cecum are seen here in a case of familial polyposis.
• These are benign. • Polyp = any growth into the lumen of the GI tract. • “stalk & poof” morphology results from the mechanical strain put on the growth by the motion of fluid traveling through the lumen. • These are examples of adenomas, which are benign neoplasms in glandular tissue. In the colon these adenomas are also dysplastic. Colon adenomas are most common in older individuals >50y.o, but can be seen in genetically susceptible younger individuals (as in familial adenomatous polyposis). These will proress to malignant neoplasms if not treated. • Presentation: generally present with occult bleeding (blood not visible in the stool, but can be identified by testing stool directly). • Treatment: surgical. |

Describe
|
|
|
• Fibroadema of the Breast (this specimen includes the tumor & surrounding parenchyma).
• Benign neoplasm more commonly found in younger women of reproductive ages. • Called an adenoma because the tissue of origin is glandular, even though the cell of origin is itself not glandular. • Blue dye was injected during a radiographic procedure to mark the location of the neoplasm so that the surgeon could find it. |

Describe
|
|
|
• Microscopic view of Fibroadenoma of the Breast
• Compressed ducts surrounded by a fibrous stoma. • These lesions are most likely to be found as a “breast lump” on examination of young women. They are discreet, firm, rubbery masses that are freely movable. |

Describe
|

