![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
157 Cards in this Set
- Front
- Back
|
How long is the cardiac action potential? |
0.2 seconds |
|
|
How much longer than skeletal muscle is the cardiac action potential? |
15 times longer |
|
|
What is the resting cardiac membrane potential? |
-90mV |
|
|
What causes the plateau during the cardiac action potential? |
Slow Ca++ channels allowing influx/depolarization |
|
|
What does the plateau in the cardiac action potential allow for, physiologically? |
Full contraction |
|
|
How does the cardiac membrane's permeability to K+ change during the action potential plateau? |
It decreases |
|
|
What two factors delay the heart's repolarization with each action potential? |
Slow Ca++ channels open Decreased permeability to K+ during the plateau (while Ca++ channels open) |
|
|
What is the velocity of the excitatory fibers in the atria and ventricles? |
0.3 - 0.5 m/sec |
|
|
How do fast sodium channels in the heart compare to those in skeletal muscle? |
They are slower |
|
|
Differentiate between absolute and relative refractory periods: |
Absolute - zero potential for another AP to cause a beat
Refractory - an AP can cause a beat, it just has to be a big one |
|
|
What causes PACs and PVCs? |
Action potential during the relative refractory period |
|
|
Potential for full strength contraction is _______ in beats triggered during refractory period (PAC/PVC) |
Lower |
|
|
What is happening, electrically, during V tach? Why is there no BP during V tach? |
Each AP is coming at the beginning of the relative refractory period. This means the heart is beating so fast, it has no time to fill. |
|
|
How are T tubules in the heart different than those in the skeletal muscle? |
Heart T tubules are 5x the size!
They have much more Ca++ |
|
|
What structure is the pacemaker of the heart? |
SA node |
|
|
What structure delays conduction between the atria and the ventricles? |
AV node |
|
|
What structure becomes the pacemaker if the SA node is destroyed? |
AV node |
|
|
What part of the heart beat corresponds to the P wave? |
Atrial systole |
|
|
What % of stroke volume comes from atrial systole? |
20% |
|
|
What system is most sensitive to decreased blood flow? |
Renal |
|
|
What will be one of the first signs of losing atrial systole volume? |
Decreased UOP |
|
|
What time point on the EKG reading represents systole? |
The electrically neutral time after depolarization |
|
|
What causes the delay between depolarization and systole? |
The slow Ca++ channels and AP plateau |
|
|
What part of the EKG tracing correlates to repolarization? |
T wave |
|
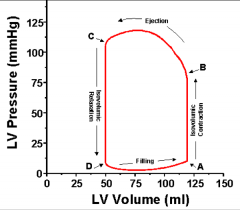
Point A is: |
End diastolic volume & start of contraction |
|
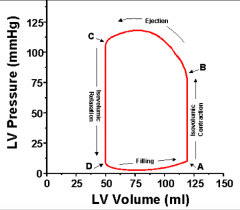
Point B is: |
Start of ejection |
|
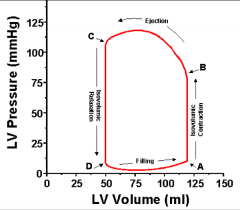
Point C is: |
End-systolic volume & end of ejection |
|
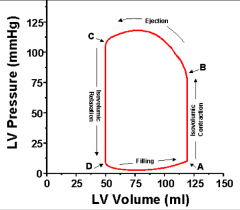
Point D is: |
Start of diastole |
|
|
What is the end systolic volume? (Both the number and a definition) |
Usually 50ml; the amount that still remains the heart when it is fully contracted at the end of systole |
|
|
Where is blood flow occurring during the post-ejection, pre-diastole isovolumic relaxation? |
From the venous system into the atria |
|
|
What happens to the pressure-volume loop if the patient has noncompliant, stiff heart tissue? |
The loop becomes narrower |
|
|
How much ejection occurs during the initial ventricular contraction? |
None; isovolumic contraction occurs until a threshold pressure is met |
|
|
What changes will occur in the pressure-volume loop in someone who is acutely intoxicated with cocaine? |
Much narrower (filling volume decreased with tachycardia) and taller (higher pressure for ejection since heart is beating against potent vasoconstriction) |
|
|
What changes will occur in the pressure-volume loop in someone who is on levophed? |
Much narrower (filling volume decreased with tachycardia) and taller (higher pressure for ejection since heart is beating against potent vasoconstriction) |
|
|
How do we calculate ejection fraction? |
SV / EDV * 100 |
|
|
What is a typical ejection fraction? |
60% |
|
|
How is CO calculated? |
HR * SV |
|
|
What is typical CO at rest? |
4-6L/min |
|
|
What can CO rise to during hard exercise? |
4-7x higher than normal |
|
|
What are the three ways we regulate the cardiac pump? |
1. Intrinsic changes (i.e. Frank-Starling) 2. Controlling rate/strength via ANS 3. Effects of electrolytes (Ca, K) |
|
|
What is the Frank-Starling law? |
The heart will increase its force in response to increased stretch; in plain English, it will pump out what comes in |
|
|
According to the Frank-Starling law, what relationship should preload and stroke volume have? |
They should be equal |
|
|
What will R atrium stretch do to HR? |
Increase it by 10-20% (SA node effect) |
|
|
What components of the ANS innervate the atria? |
Vagus nerve (PSNS); specifically SA, AV nodes Sympathetic chains (SNS) |
|
|
What components of the ANS innervate the ventricles? |
Sympathetic chains (SNS) |
|
|
What are the SNS effects on the heart? |
Increased HR Increased contractility (activation of β receptors) |
|
|
What are the PSNS effects on the heart? |
Mostly just decrease of HR No real effect on ventricular function |
|
|
What would happen to the heart if sympathetic stimulation were cut off? |
CO would decrease, but heart would still function |
|
|
What is more stimulating to the CV system: intubation or surgical manipulation? |
Intubation |
|
|
How does increased K+ in the ECF affect the functioning of the heart? |
Membrane potential is less negative... This means intensity of AP is lower... This means contraction strength decreases.
Also, HR decreases. |
|
|
How can excess K+ affect the physical structure of the heart? |
Can dilate the myocardium |
|
|
How does excess Ca2+ in the ECF affect the functioning of the heart? |
Causes spastic contractions |
|
|
How does low Ca2+ affect the heart? |
Causes flaccidity |
|
|
What is the physical structure of arteries? How does blood flow through arteries? |
Strong, muscular walls
Blood flow - fast, high pressure |
|
|
How does blood flow through arterioles? |
This is the point at which flow is downregulated dramatically |
|
|
What is the physical structure of veins? |
Thin walls, but muscular enough to expand and contract |
|
|
What is another name for the venous system? |
Capacitance system |
|
|
What % of the body's blood is found in the lungs at any given point? |
9% |
|
|
What % of the body's blood is found in the heart at any given point? |
7% |
|
|
What % of the body's blood is found in the venous system at any given point? |
60% |
|
|
What % of the body's blood is found in the arterial system at any given point? |
24% |
|
|
Pressure, resistance, and velocity of the systemic circulation are: |
High pressure High resistance High velocity |
|
|
Pressure, resistance, and velocity of the pulmonary circulation are: |
Low pressure Low resistance Low velocity |
|
|
What organs get the greatest % of blood flow, and how much do they get? |
Kidneys - 22% GI system and spleen - 21% Skeletal muscle - 15% Brain - 14% |
|
|
What % of the body's blood does the heart itself require? |
3% |
|
|
Why do arterioles have to decrease the pressure going to the organs? |
If the organs are hit with the high pressures at the capillary level, there will be no chance for exchange |
|
|
What part of the circulatory system has the highest pulse pressure? |
Left ventricle |
|
|
What part of the circulatory system has the lowest pulse pressure? |
Capillaries and veins |
|
|
How will stiffening of the aorta affect blood pressure? |
High pressures needed to get the same flow out of the heart |
|
|
What causes intrinsic hypertrophy of the septum? |
Increased Ca2+ channels (genetic) |
|
|
Why is hypertrophy of the septum problematic? |
Heart is very muscular and strong, so ejection velocity is very fast
Heart is unable to relax and let volume in, so during exercise it becomes depleted and dies |
|
|
What is the equation for Ohm's law? |

|
|
|
What measurement of pressure determines blood flow through a tube/vessel? |
Pressure difference between the two ends
NOT pressure inside the vessel/tube |
|
|
Increased resistance leads to _______ flow: |
Increased resistance leads to decreased flow. |
|
|
Flow is __________ proportional to pressure gradient and ___________ proportional to resistance. |
Flow is directly proportional to pressure gradient and inversely proportional to resistance. |
|
|
How do medications that strictly increase vascular resistance affect blood flow? |
Decrease blood flow |
|
|
What does flow refer to? |
Amount of blood that passes a point over a given amount of time |
|
|
Describe laminar flow: |
Straight paths for fluid; fluid in middle travels faster than fluid on edges |
|
|
Describe turbulent flow: |
Fluid takes spiraling, curved paths that cut back and forward |
|
|
What is the equation for Reynold's number? |

|
|
|
What does a Reynold's number greater than 2000 indicate? Less than 2000? |
> 2000 = turbulent flow < 2000 = laminar flow |
|
|
What sort of conditions cause turbulent flow? |
Rapid rate Obstructions Sharp turns Rough surfaces |
|
|
According to the Reynold's number equation, what factors will increase the chance of turbulent flow? |
Higher density Large diameter of vessel High velocity Low viscocity |
|
|
What does critical velocity refer to when discussing flow? |
The velocity at which flow transitions from laminar to turbulent, all other factors consistent |
|
|
Why is turbulent flow bad for patients with atherosclerotic disease? |
Turbulent flow can dislodge plaques and cause embolic stroke/MI |
|
|
What is the equation for Poiseuille's Law? |

|
|
|
According to Poiseuille's Law, if the length of a tube is doubled, what happens to the flow? |
The flow is halved |
|
|
According to Poiseuille's Law, if the width of a tube is doubled, what happens to the flow? |
The flow is 16-fold |
|
|
What happens to blood flow with polycythemia? |
Flow decreases because viscosity increases |
|
|
The total resistance in a series is _______ than resistance in any single vessel.
__________ blood will flow through parallel vessels than through one single vessel. |
The total resistance in a series is far less than resistance in any single vessel.
Far more blood will flow through parallel vessels than through one single vessel. |
|
|
What does less resistance at the organ level mean for regulation? |
Organs are able to accommodate increased/decreased flow more easily |
|
|
What advantages does the parallel circuit circulation afford the end organs? |
Lower resistance and lower pressure |
|
|
What is the equation for LaPlace's law, applied to capillaries? |
T = P * r |
|
|
What causes altitude sickness? |
Lung vessels will constrict in response to low O2; this causes such increased pressure in the lungs that capillaries become permeable (high tension) and pulmonary edema occurs |
|
|
How do organs regulate blood flow? |
Via changes to resistance |
|
|
How quickly do organs achieve acute control of blood flow? |
Within minutes |
|
|
What is the #1 reason why local blood flow changes? |
Change in O2 pressure |
|
|
What is the metabolic theory of blood flow regulation? |
Changes in O2 pressure cause the release of mediators that activate pathways which cause vasodilation or vasoconstriction |
|
|
What are the mediators released according to the metabolic theory of blood flow regulation? |
Adenosine Histamine CO2 H+ K+ |
|
|
What is the myogenic theory of blood flow regulation? |
Sudden stretch of vascular smooth muscle (from increased BP) causes a reflex contraction in order to keep radius consistent |
|
|
How does nitric oxide affect the vessels? |
Causes vasodilation |
|
|
What kind of stimuli lead to nitric oxide release? |
Chemical or physical |
|
|
What substance is released when vessels are injured and how does it affect their size? |
Endothelin; is a vasoconstrictor |
|
|
Is the myogenic reflex endothelium-dependent? |
No; depends only on presence of vascular smooth muscle |
|
|
In what organ is CO2 an especially potent vasodilator? |
The brain |
|
|
Why do we see a BP drop from morphine? |
Morphine is a histamine releasing drug; histamine has a vasodilatory effect |
|
|
How does O2 regulation of vascular resistance differ in the lungs? |
Decreased O2 in the lungs causes vasoconstriction rather than dilation, to shunt blood away from poorly-ventilated areas of the lungs
Called Hypoxic Pulmonary Vasoconstriction |
|
|
What are some endogenous vasoconstrictors? |
Norepinephrine Angiotensin II Vasopressin |
|
|
What are some endogenous vasodilators? |
Bradykinin Histamine |
|
|
Do the brain, heart, and skeletal muscle have more metabolic or neurogenic control of blood flow? |
Metabolic; blood flow based upon activity level |
|
|
Do the skin, kidney, and splanchnic organs have more metabolic or neurogenic control of blood flow? |
Neurogenic; based mostly on sympathetic activity levels (so blood can go to the important stuff when the body is very sympathetically stimulated) |
|
|
How is resistance/blood flow to tissues regulated long-term? |
Angiogenesis |
|
|
What are three angiogenesis-causing factors? |
VEGF - vascular endothelin growth factor Fibroblast growth factor Angiogenin |
|
|
What type of conditions cause angiogenesis? |
Metabolic increases in an area (i.e. a tumor) Blockages to blood flow (i.e. a plaque) |
|
|
Describe the autoregulation curve: |
Below lower limit and above upper limit (of pressure), blood flow and perfusion pressure are linearly related.
Between the limits, blood flow remains nearly constant despite change in perfusion pressure. |
|
|
What is the lower limit of the autoregulation curve in a healthy young adult? |
~50mmHg |
|
|
What is the upper limit of the autoregulation range in a healthy young adult? |
~180mmHg |
|
|
How does a hx of HTN affect the autoregulation curve? |
Shifts it to the right |
|
|
Where are the vasoconstrictor areas located in the brainstem? |
Bilaterally, in the anterolateral portions of the upper medulla
(Preganglionic vasoconstrictor neurons of the SNS) |
|
|
Where are the vasodilator areas located in the brainstem? |
Bilaterally, in the anterolateral portions of the lower medulla
Their fibers project upward into the upper medulla and the vasoconstrictor areas, which they inhibit |
|
|
Where is the sensory area located that helps regulate the vasoconstrictor/vasodilator areas of the medulla? |
Bilaterally, in the tractus solitarius in the posterolateralo portions of the medulla and lower pons |
|
|
What nerves does the tractus solitarius recieve input from? |
Vagus and glossopharyngeal |
|
|
What effect does stimulation of the muscarinic receptors of the heart have? |
Decreased heart rate Slightly decreased contractility |
|
|
What effect does stimulation of the β1 receptors of the heart have? |
Increased HR & contractility |
|
|
From what system does the baroreceptor reflex arise? |
Nervous |
|
|
Where are baroreceptors found? |
Aorta Carotid bodies Glossopharyngeal nerve |
|
|
How does the baroreceptor reflex work? |
When baroreceptors detect increased volume, they send a signal to the brain to slow the HR and stabilize CO |
|
|
How does the Bainbridge reflex work? |
Stretch receptors in the atria send signals to the medulla via the vagus nerve
Return efferent signals are sent via both the vagus and the SNS; the SNS signal is stronger and overrides, leading to increased HR/contractility |
|
|
What is the physiological advantage of the Bainbridge reflex? |
Prevents blood from pooling in the veins and pulmonary circulation when volumes increase |
|
|
What are two reasons that increased pressure can lead to increased heart rate? |
1. Direct stretch of the RA and SA node 2. Bainbridge reflex |
|
|
What is the relationship between venous return and cardiac output? |
They are equal, or should be |
|
|
What's the average male CO? |
5.6 L/min |
|
|
What's the average female CO? |
4.9 L/min |
|
|
What factors influence CO? |
Metabolic rate Exercise Individual size Age |
|
|
What's the average 80 year old's CI? |
2.4 L/min |
|
|
Under resting conditions, CO is controlled almost entirely by _______________. |
Under resting conditions, CO is controlled almost entirely by peripheral mechanisms. |
|
|
What are two ways to calculate CO? |
CO = HR * SV
CO = Arterial pressure / SVR |
|
|
What factors control cardiac rate? |
PSNS and SNS innervation |
|
|
What factors control stroke volume? |
MAP Frank-Starling factors (contraction strength, stretch, EDV) |
|
|
What conditions make the heart hypereffective? |
Hypertrophy (to a point) Exercise |
|
|
What conditions make the heart hypoeffective? |
Disease states (advanced hypertrophy) Valve disease Anything causing akinesic or dyskenesic ventricles |
|
|
How does changing ventilation to positive-pressure affect cardiac output? |
PPV will decrease CO unless blood pressure increases to compensate |
|
|
What conditions shift the RA pressure-CO curve to the right? |
PPV Opening the thoracic cage Cardiac tamponade |
|
|
How does regional anesthesia benefit people with cardiac disease? |
Does not increase the pressure required to maintain CO like intubation and PPV does |
|
|
At what point does atrial filling stop with each heart beat cycle? |
When the RA pressure equals the mean systemic filling pressure |
|
|
How do pressors lead to decreased cardiac output? |
Mean systemic filling pressure increases, which means less volume is able to fill the heart before RA pressure equals filling pressure |
|
|
Define mean systemic filling pressure: |
Pressure that pushes venous blood from system into heart |
|
|
What is the average filling pressure? |
7mmHg |
|
|
What happens if RA pressure rises dramatically? |
Blood backs up and pools in venous system Causes edema due to high hydrostatic pressure (LaPlace's law!) |
|
|
What happens when the atrial pressure is higher than the mean filling pressure? |
The atria will not fill |
|
|
How much of the CO does the heart take for itself? |
5% |
|
|
What parts of the heart does the LCA supply? |
The anterior and lateral left ventricle |
|
|
What parts of the heart does the RCA supply? |
The right ventricle Posterior part of left ventricle |
|
|
How does most blood return to systemic circulation from the coronary circulation? What % is accounted for this way? |
75%, via the coronary sinus, from the left ventricle back into the right atrium |
|
|
What veins return blood from the right ventricle's circulation? |
Small anterior veins |
|
|
What vessels supply the myocardium during systole? |
Subendocardial vessels |
|
|
During what phase of the cardiac cycle do the coronary arteries fill? |
Diastole |

