![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
Hypothalamic Agents
What is Somatotropin? |
a growth hormone; stimulates the growth & metabolism of almost all cells in the body
recombinant form of human GH, restores normal growth & metabolic GH effects in GH-deficient individuals |
|
|
Hypothalamic Agents
What happens with a deficiency of somatotropin? With an excess? |
Deficiency = Dwarfism
Excess = Acromegaly (usually caused by a pituitary tumor) |
|
|
Hypothalamic Agents
What is Octreotide? |
a synthetic growth hormone (GH) antagonist structurally related to somatostatin, inhibits acromegaly
Inhibits production of GH & to a lesser extent , of TSH, glucagon, insulin, & gastrin |
|
|
Hypothalamic Agents
What is Pegvisomant? |
newest agent that is GH antagonist, blocks GH receptors
Ameliorates effects of excess GH production, acromegaly |
|
|
Anterior Pituitary Agents
Agents (5)? |
Corticotropin (ACTH, Acthar)
Cosyntropin (Cortosyn) Somatrem (Protropin) Somatropin (Genotropin, Humatrope, others) Thyrotropin [Thyrogen, Thyroid-stimulating hormone (TSH)] |
|
|
Posterior Pituitary Agents
What is Anti-Diuretic Hormone (ADH)? |
conserves H2O in the body
Secreted by the posterior pituitary when the hypothalamus senses low plasma volume or if osmolality is too high |
|
|
Posterior Pituitary Agents
Agents (2)? |
Used for SIADH
Desmopressin Acetate (DDAVP, Stimate) - most common form of ADH in use - intranasal form most common Vasopressin (Pitressin) - drug for Diabetes Insipidus, potent vasoconstrictor |
|
|
Thyroid Drugs
What are the two types of cells in the thyroid gland & what do they secrete? |
Thyroid gland: consists of two types of cells which secrete different hormones.
Parafollicular cells: secrete calcitonin Follicular cells: secrete thyroid hormones (T4 & T3) |
|
|
Thyroid Drugs
What role does iodine play w/Thyroid function? |
Iodine is essential for the synthesis of T4 and T3 (provided via intake)
|
|
|
Thyroid Drugs
What is Hashimoto's thyroiditis? |
autoimmune thyroiditis - most common presentation of hypothyroidism
|
|
|
Thyroid Drugs (Hypothyroidism)
Agents (3)? |
Levothyroxine (Levothroid, Synthroid, others)
Liothyronine (Cytomel, Triostat) - specific for T3 Thyroid (Armour Thyroid, Westhroid) |
|
|
Antithyroid Drugs
What is the most common presentation of hyperthyroidism? How much more common in women? In which age group is it most common? |
Grave's disease is the most common presentation
4-8xs more common in women 30-40 year olds most common |
|
|
Antithyroid Drugs (Hyperthyroidism)
Agents (4)? |
Thioamides:
Methimazole (Tapazole) Potassium Iodide (ThyroShield, SSKI) Propylthiouracil (PTU) Radioactive Iodine (I131, RAI) |
|
|
Antithyroid Drugs
What are concerns about methimazole? |
Methimazole (Tapazole) is a thioamide and is pregnancy category D - crosses the placenta more readily.
|
|
|
Antithyroid Drugs
What are concerns about Sodium iodine-131? |
Radioactive Iodine (I-131, RAI) destroys follicular cells with radiation (contraindicated in pregnancy)
Used to shrink thyroid prior to surgery |
|
|
Antithyroid Drugs
What is Lugol's solution? |
nonreactive iodine, inhibits organificaiont & hormone release, reduce the size & vascularity of gland
|
|
|
What are the three essential classes of steroids secreted by the adrenal glands?
|
Glucocorticoids
Mineralcorticoids Gonadocorticoids |
|
|
Which two steroids are known as corticosteroids or adrenocortical hormones"?"
|
Glucocorticoids & mineralocorticoids
|
|
|
95% of the mineralocorticoids secreted by the adrenals are what?
|
Aldosterone
|
|
|
What is the primary function of Aldosterone?
Aldosterone + Androgen = ?? |
The primary function of aldosterone is to promote Na reabsorption & K+ excretion by the renal tubules, thus regulating plasma volume.
Aldosterone + Androgen = Mineralocorticoid |
|
|
What does the kidney due when plasma volume is low?
|
The kidneys secrete renin --> production of Angiotensin II
Angiotensin II --> aldosterone secretion --> promonts Na & water retention |
|
|
What is hyperaldosteronism?
|
condition from excessive aldosterone secretion usually as a result of adrenal tumors, characterized by hypertension and hypokalemia.
|
|
|
How many glucocorticoids are secreted by the adrenal cortex?
|
More than 30 glucocorticoids are secreted.
|
|
|
What is hydrocortisone?
|
The most important pharmacologically glucocorticoid. Affects the metabolism of nearly every cell & prepares the body for long term stress.
|
|
|
What are five effects of glucocorticoids?
|
Increases blood glucose
Increases the breakdown of proteins & lipids & their utilization as energy sources. Suppresses the inflammatory response Increases the sensitivity of vascular smooth muscle to norepinephrine & angiotensin II. Influences the CNS by affecting mood & maintaing normal brain excitability. |
|
|
What is the first (of four) steps of glucocorticoid secretion?
|
Secretion begins with corticotropin-releasing hormone (CRF) secreted by the hypothalamus.
|
|
|
What is the second (of four) steps of glucocorticoid secretion?
|
CRF travels to the pituitary, where it causes the release of ACTH.
|
|
|
What is the third (of four) steps of glucocorticoid secretion?
|
ACTH then travels through the blood & reaches the adrenal cortex, causing it to release glucocorticoids.
|
|
|
What is the fourth (of four) steps of glucocorticoid secretion?
|
When the level of cortisol in the blood increases, it provides negative feedback to the hypothalamus and the pituitary to shut off further release of glucocorticoids.
|
|
|
What is adrenal insufficiency?
What is the role of glucocorticoids in relationship to adrenal insufficiency? |
Lack of corticosteroid.
Glucocorticoids are used as replacement therapy for adrenal insufficiency and to decrease inflammation and immune responses. Need to taper when d/c to prevent adrenal suppression. |
|
|
Name the main twelve uses of glucocorticoid?
|
Adrenal insufficiency
Allergies (seasonal rhinitis) Chronic inflammatory bowel disease Asthma & COPD Edematous states caused by hepatic, neurological & renal disorders Neoplastic disease Post-transplant surgery Rheumatic diseases Shock Skin disorders (rash, contact dermatitis, etc.) Others |
|
|
How might glucocorticoids interact with
anti-diabetic agents? |
Hyperglycemic effects may decrease the effectiveness of the anti-diabetic agents.
|
|
|
How might glucocorticoids interact with
NSAIDs? |
Combining with NSAIDs increases the risk for PUD
|
|
|
How might glucocorticoids interact with
non-potassium sparing diuretics? |
Administering with non-potassium-sparing diuretics --> hypokalemia & hypocalcemia.
|
|
|
Glucocorticoid prescribing strategies:
dosing? |
Keep doses to the lowest possible amount to achieve a therapeutic effect.
|
|
|
Glucocorticoid prescribing strategies:
administration? |
Administer every other day to limit adrenal atrophy.
|
|
|
Glucocorticoid prescribing strategies:
for acute conditions? |
For acute conditions, prescribe large amounts for a few days, and then gradually decrease the does until discontinued.
|
|
|
Glucocorticoid prescribing strategies:
to decrease systemic effects? |
To decrease the possibility of systemic effects, use inhalation, topical or intra-arterial routes.
|
|
|
What does long-term administration of glucocorticoids put a person at risk for?
|
Cushing's syndrome
|
|
|
Name two short-acting glucocorticoids
What patient would be using this? |
Cortisone (Cortistan, Cortone)
Hydrocortisone (Cortef, Hydrocortone, others) Usually given as a topical for skin irritation. |
|
|
Name four intermediate acting glucocorticoids
What patient would be using this? |
Methylprednisolone (Medrol, others)
Prednisolone (Delta-Cortef, others) Prednisone (Deltasone, Meticorten, others) Pt with hives in an urgent care receiving via IV Prednisone is for COPD or chemo patient. |
|
|
Name two long-acting glucocorticoids
What pt would be using this? |
Betamethasone (Celestone)
Dexamethasone (Decadron, Dexasone, others) Dexamethasone suppression test - r/o Cushing's |
|
|
What is the Somogyi Effect & what is the treatment?
|
Nocturnal hypoglycemia develops stimulating a surge of counter regulatory hormones which raises blood sugar.
Tx: Reduce or omit h.s. dose of insulin |
|
|
What is the Dawn Phenomenon & what is the treatment?
|
Results when tissue becomes desensitized to insulin nocturnally - blood glucose becomes progressively elevated throughout the night.
Tx: Add or increase the h.s. dose of insulin |
|
|
Diabetes Drugs: Biguanides
Agent (1)? |
Metformin (Glucophage)
|
|
|
Diabetes Drugs: Biguanides
Indications? |
Drug of choice; first line therapy for Type 2 DM, promotes weight loss
Contraindicated in liver disease & renal dysfunction (serum creatinine ≥ 1.5 males & 1.4 females) need to monitor creatinine. |
|
|
Diabetes Drugs: Biguanides
MOA? |
Decreases hepatic gluconeogenesis, improves insulin sensitivity, increases glucose utilization by muscle.
Does not cause insulin secretion, therefore no concern for hypoglycemia. |
|
|
Diabetes Drugs: Biguanides
Adverse Effects? |
Nausea, vomiting, diarrhea, decreased appetite
Rare (but fatal): lactic acidosis (s/s muscle pain). Stop use for 48 hrs after procedures w/contrast. Need to check creatinine before restarting metformin. |
|
|
Diabetes Drugs: Insulin Secretagogues, Nonsulfonylureas (Glinides)
Agents (2)? |
Nateglinide (Starlix)
repaglinide (Prandin) - affected by renal impairment |
|
|
Diabetes Drugs: Insulin Secretagogues, Nonsulfonylureas (Glinides)
Indications? |
Monotherapy or combination therapy for Type 2 DM
Use with caution in liver dysfunction. Dose adjustment required for renal dysfunction |
|
|
Diabetes Drugs: Insulin Secretagogues, Nonsulfonylureas (Glinides)
MOA? |
Stimulates insulin release from pancreas
Rapid onset (give w/ meals) & short duration of action (requires TID dosing) |
|
|
Diabetes Drugs: Insulin Secretagogues, Nonsulfonylureas (Glinides)
Adverse Effects? |
Hypoglycemia, diarrhea, arthralgia, headache, sinusitis, upper respiratory infection
Several drug-drug interactions |
|
|
Diabetes Drugs: Insulin Secretagogues, Sulfonylureas
Agents (6)? |
Chlorpropamide (Diabinese) - older agents, disulfiram rxn
Tolazamide (Tolinase) - older agents Tolbutamide (Tol-Tab) - older agents Glyburide (Diabeta, Micronase) Glipizide (Glucotrol) Glimepiride (Amaryl) |
|
|
Diabetes Drugs: Insulin Secretagogues, Sulfonylureas
Indications? |
Monotherapy or combination therapy for Type 2 DM
Use with caution in liver dysfunction. Dose adjustment required for renal dysfunction |
|
|
Diabetes Drugs: Insulin Secretagogues, Sulfonylureas
MOA? |
Stimulates insulin release from pancreas, enhances beta cell sensitivity to glucose
Over time, response to therapy may diminish. Possibly desensitizes receptors |
|
|
Diabetes Drugs: Insulin Secretagogues, Sulfonylureas
Adverse Effects? |
Hypoglycemia, nausea, bloating, weight gain, photosensitivity, disulfiram reaction (chlorpropamide)
Several drug-drug interactions Use caution w/sulfa allergy |
|
|
Diabetes Drugs: Thiazolidinediones
Indications? |
Monotherapy or combination therapy for Type 2 DM - 3rd line agent Reserved when other agents not working
Use with caution (if at all) in liver dysfunction – baseline LFTs & periodically afterwards Contraindicated in NYHA class III or IV |
|
|
Diabetes Drugs: Thiazolidinediones
Agents (2)? |
Pioglitazone (Actos)
Rosiglitazone (Avandia) – REMS program, no new pts |
|
|
Diabetes Drugs: Thiazolidinediones
MOA? |
Increases receptor sensitivity to insulin, decreases both insulin resistance & hepatic gluconeogenesis. No increase of insulin secretion
|
|
|
Diabetes Drugs: Thiazolidinediones
Adverse Effects? |
Hepatotoxicity, weight gain, peripheral edema, rash, macular edema, heart failure exacerbation, increase risk of MI (rosiglitazone)
Several drug-drug interactions, metabolized by liver May increase risk of osteoporosis May increase risk of bladder cancer (pioglitazone) |
|
|
Diabetes Drugs: Alpha-glucosidase Inhibitors
Indications? |
Adjunct therapy only for Type 2 DM, esp if post-prandial BS elevated.
Do not use in renal dysfunction (creatinine > 2.0) Contraindicated in malabsorption, IBD, or intestinal obstruction. |
|
|
Diabetes Drugs: Alpha-glucosidase Inhibitors
Agents (2)? |
Acarbose (Precose) – baseline LFTs then periodically afterwards
Miglitol (Glyset) |
|
|
Diabetes Drugs: Alpha-glucosidase Inhibitors
MOA? |
Reduces rate & extent of CHO digestion & absorption
|
|
|
Diabetes Drugs: Alpha-glucosidase Inhibitors
Adverse Effects? |
Flatulence, diarrhea, abdominal pain, decreased absorption of iron (anemia)
May influence absorption of other drugs. Glucose (dextrose) is recommended for treating hypoglycemia as sucrose metabolism is inhibited. |
|
|
Diabetes Drugs: Glucagon-like Peptide-1 Agonists
Indications? |
Monotherapy (exenatide) or combination therapy for Type 2 DM; generally considered as adjunct – does not replace insulin. For pts who fail metformin alone, or with glinides or sulfonylureas
Contraindicated in severe renal dysfunction (both), h/o pancreatitis (both), & h/o thyroid CA (liraglutide) |
|
|
Diabetes Drugs: Glucagon-like Peptide-1 Agonists
Agents (2)? |
Exenatide (Byetta)
Liraglutide (Victoza) REMS program - d/t risk for pancreatitis & thyroid tumors |
|
|
Diabetes Drugs: Glucagon-like Peptide-1 Agonists
MOA? |
Increase insulin release in the presence of elevated glucose concentrations, decrease glucagon secretion in a glucose-dependent manner & delay gastric emptying.
|
|
|
Diabetes Drugs: Glucagon-like Peptide-1 Agonists
Adverse Effects |
Nausea, vomiting, diarrhea, headache hypoglycemia, pancreatitis, teratogenic, injection site reactions, renal failure, thyroid tumors
Several drug-drug interactions |
|
|
Diabetes Drugs: Dipeptidyl Peptidase-4 Inhibitors
Indications? |
Monotherapy or combination therapy for Type 2 DM; generally considered as adjunct therapy
Contraindicated in ESRD & dose adjustment in renal impairment (sitagliptin, saxagliptin) |
|
|
Diabetes Drugs: Dipeptidyl Peptidase-4 Inhibitors
Agents (3)? |
Sitagliptin (Januvia)
Saxagliptin (Onglyza) Linagliptin (Tradjenta) |
|
|
Diabetes Drugs: Dipeptidyl Peptidase-4 Inhibitors
MOA? |
Inhibit the degradation of GiP and GLP-1
|
|
|
Diabetes Drugs: Dipeptidyl Peptidase-4 Inhibitors
Adverse Effects? |
Increased risk of infection (URI --> sepsis), headache, hypoglycemia, pancreatitis, hypersensitivity reactions, peripheral edema (saxagliptin)
Several drug-drug interactions (saxagliptin) |
|
|
Diabetes Drugs: Amylin Receptor Agonists
Indications? |
Adjunct therapy for Type 1 & Type 2 DM
Contraindicated in pts with hypoglycemic unawareness or gastroparesis Black Box warning for individuals while driving |
|
|
Diabetes Drugs: Amylin Receptor Agonists
Agents? |
Pramlintide (Symlin)
When initiating, reduce dose of any secretagogues, reduce insulin dose by at least 50% |
|
|
Diabetes Drugs: Amylin Receptor Agonists
MOA? |
Inhibit the degradation of GiP & GLP-1
|
|
|
Diabetes Drugs: Amylin Receptor Agonists
Adverse Effects? |
Abdominal pain, loss of appetite, nausea, vomiting, hypoglycemia, dizziness, headache, cough, fatigue
Severe hypoglycemia with concurrent insulin or oral hypoglycemic agent |
|
|
Diabetes Drugs: Combination Drugs & Others
Agents |
Glipizide/Metformin (Metaglip)
Glyburide/Metformin (Glucovance) Rosiglitazone/Glimepride (Avandaryl) Pioglitazone/Metformin (ACTOplusmet) Rosiglitazone/Metformin (Avandamet) |
|
|
Insulin Preparations: Rapid Acting
Agents (3)? |
Insulin Lispro (Humalog)
Insulin Aspart (NovoLog) Insulin Glulisine (Apidra) SQ only |
|
|
Insulin Preparations: Rapid Acting
Onset of Action? |
5-15 minutes
mimics body kinetics the best |
|
|
Insulin Preparations: Rapid Acting
Peak Action? |
30-90 minutes
|
|
|
Insulin Preparations: Rapid Acting
Duration of Action? |
< 5 hours
|
|
|
Insulin Preparations: Short Acting
Agents (1)? |
Regular insulin (Humulin R)
Can be given SQ or IV |
|
|
Insulin Preparations: Short Acting
Onset of Action? |
0.5-1 hour
|
|
|
Insulin Preparations: Short Acting
Peak Action? |
2-4 hours
|
|
|
Insulin Preparations: Short Acting
Duration of Action? |
5-7 hours
|
|
|
Insulin Preparations: Intermediate Acting
Agent (1)? |
NPH
|
|
|
Insulin Preparations: Intermediate Acting
Onset of Action? |
2-4 hours
|
|
|
Insulin Preparations: Intermediate Acting
Peak Action? |
4-12 hours
|
|
|
Insulin Preparations: Intermediate Acting
Duration of Action? |
12-18 hours
|
|
|
Insulin Preparations: Long Acting
Agents (2)? |
Insulin glargine (Lantus)
Insulin detemir (Levemir) Less peaks & valleys |
|
|
Insulin Preparations: Long Acting (glargine)
Onset of Action? |
1.5 hours
|
|
|
Insulin Preparations: Long Acting (glargine)
Peak Action? |
No pronounced peak
|
|
|
Insulin Preparations: Long Acting (glargine)
Duration of Action? |
20-24 hours
|
|
|
Insulin Preparations: Long Acting (detemir)
Onset of Action? |
0.8-2 hours
|
|
|
Insulin Preparations: Long Acting (detemir)
Peak Action? |
Relatively flat
|
|
|
Insulin Preparations: Long Acting (detemir)
Duration of Action? |
5.7-23.2 hours
|
|
|
Insulin Preparations
NPH/regular (70/30) |
Humulin 70/30
Novolin 70/30 |
|
|
Insulin Preparations
Insulin aspart protamine suspension / insulin aspart (70/30) |
NovoLog Mix 70/30
|
|
|
Insulin Preparations
Insulin lispro protamine suspension / insulin lispro (70/25) |
Humalog Mix 75/25
|
|
|
Insulin Preparations
Insulin lispro protamine suspension / insulin lispro (50/50) |
Humalog Mix 50/50
|
|
|
Endocrine Physiology Review
What is the role of the hypothalamus in the endocrine system? |
Hypothalamus secretes releasing hormones to the pituitary gland. These trigger the pituitary to know what hormones are to be released.
Hypothalamus secretes thyrotropin-releasing hormone (TRH) --> pituitary --> secretes TSH --> thyroid hormones |
|
|
Endocrine Physiology Review
What are the two parts of the pituitary gland? |
Anterior (adenohypophysis)
Posterior (neurohypophysis) |
|
|
Endocrine Physiology Review
What is the adenohypophysis? |
The anterior pituitary lobe that consists of glandular tissue & secretes ACTH, TSH, growth hormone, prolactin, FSH & LH
|
|
|
Endocrine Physiology Review
What is the neurohypophysis? |
The posterior pituitary lobe that contains nervous tissue rather than glandular. Neurons in the posterior pituitary store ADH & oxytocin (released in response from nerve stimulation in the hypothalamus).
|
|
|
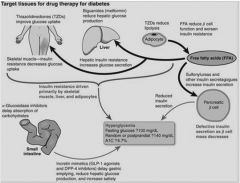
Target tissues for drug therapy for diabetes?
|
|
|
|
What is the ADA recommendations for glycemic control for most nonpregnant adults with diabetes?
|
A1C: 7% (5.5-7%/6)
Before meals: 70-130 After meals: < 180 |

