![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
What is the definition of a myopathy?
|
A disease in which the structure of function of muscle is compromise
|
|
|
What is the definition of muscular dystrophy?
|
An inherited, progressive disorder of muscle, usually due to an abnormality in a structural protein
|
|
|
What are the different kinds of muscuar dystrophies?
|
Dystrophin deficiency
Limb-girdle muscular dystrophy Other reginal muscular dystrophies Myotonic dystrophy |
|
|
What are the epinems associated with dystrophin deficiency?
|
Duchenne's: the most serious
Becker's: less serious |
|
|
What are the clinical features of Duchenne's Muscular dystrophy?
|
Boys only
Normal at birth At the onset of walking -Remain clumsy longer than normal -Gower's sign -Can't run, jump Calf pseudohypertrophy: calves are filled with connective tissue |
|
|
What is Gower's sign. Who shows it?
|
Kids march up the legs with hands to stand up off the floor
Boys with Duchenne's Muscular dystrophy |
|
|
As a kid ages, what are the different stages of Duchenne's Muscular dystrophy?
|
2-6: Gain motor skills, they appear to improve
6-7: start to fall without warning 8-10: lose ability to climb stairs, stand from the floor 12: wheelchair dependent |
|
|
What are the other systemic problems that are present in kids with Duchenne's Muscular dystrophy?
|
Deterioration in respiratory function due to weakness, scoliosis
Cardiac abnormalities Cognitive impairment |
|
|
What are some of the cardiac abnormalities found in Duchenne's Muscular dystrophy?
|
Wall thickness, wall motion, valve motion abnormalitis
Intra-atrial conduction abnormalities |
|
|
What are the two types of dystrophin deficiencies?
|
Duchenne's
Becker's |
|
|
What are the clinical features of Becker's?
|
Average onset of muscular symptoms is at 12...can be as late as 40
Can walk until the late teens, may not need a wheelchair until 20's Cardiomyopathy is common Normal cognition |
|
|
What's the prognosis for the different dystrophin deficiency?
|
Duchenne's:
die in late teens/twenties from respiratory failure (usually) or cardiac failure (occasionally) Becker's: Die in the 5th decade, sometimes later |
|
|
What's the pathology behind the dystrophin deficiency?
|
Lack of the dystrophin protein (duchenne's) or mutations in it (Becker's) causes a lack of stabilization of the muscle fibers
As a result, you get focal tears in the muscle, resulting in more Ca influx, which leads to more tearing, which leads to necrosis due to the activation of proteolytic enzymes, ultimately |
|
|
What changes in the muscles do you see in dystrophin deficiency?
|
Initially:
-Degeneration and phagocytois of single muscle fibers or groups of fibers -Stimulation of regeneration: basophilia of cytoplasm, hyperplasia and nucleolation of nuclei As the disease progresses: -Loss of muscle fibers -Residual fibers that are variable in size -Fibrosis -Increased lipocytes |
|
|
What is the histology of muscles with dystrophin deficiency?
|
Lack of striation
Nuclei in the middle of the cells Lots of connective tissue LATE: -Adipocytes -Fibrosis |
|
|
What genetic changes take place during Duchenne's? Beckers?
|
Duchenne's: deletion of the dystrophin gene
Becker's: dystrophin mutations, but preservation of the correct ORF |
|
|
What tests should you order for a diagnosis of dystrophin deficiency?
|
Blood levels: increased creating kinase
EMG changes Genetic testing of the dystrophin gene |
|
|
What's the management of the dystrophin deficiencies?
|
Prednisone for Duchenne's, not for Becker's
-Benefit lasts for 3 years Supportive care |
|
|
What is the cause of the limb-girdle muscular dystrophies?
|
Mutations in the dystrophin-associated proteins, other muscle proteins
Based on the proteins mutated, you'll get a specific pattern of muscle involvement |
|
|
What are some of the other regional muscular dystrophies?
|
Emery-Dreifuss
Facio-scapulo-humeral Oculopharyngeal |
|
|
What is the inheritance of Emery-Dreifuss regional muscular dystrophy? Where does it effect?
|
X-linked recessive
Cardiac involvement |
|
|
What is the inheritance of Facio-scapulo-humeral regional muscular dystrophy? Where does it effect?
|
Autosomal dominant
Face and shoulder girdle, legs THE FOREARMS ARE SPARED: THEY LOOK LIKE POPEYE |
|
|
What is the inheritance of oculopharyngeal regional muscular dystrophy? Where does it effect?
|
Autosomal dominant (prominent in French-canadians)
Eye muscle weakness, ptosis, then dysphagia |
|
|
What are the clinical features of myotonic dystrophy?
|
Autosomal dominant
Weakness, atrophy Myotonia Multisystem abnormalities |
|
|
What does it mean if someone has myotonia?
|
You can't release the muscle after you contract it:
-Can't let go of the door handle -Legs freeze |
|
|
What is the pattern of weakness in myotonic dystrophy?
|
In order
Face: Ptosis Muscles of eye and mouth closure Temporalis Arms: Small muscles of hands Extensor muscles of forearms Neck: SCM Muscles of the larynx, pharynx |
|
|
What kind of facial appearance does someone with Myotonic dystrophy have?
|
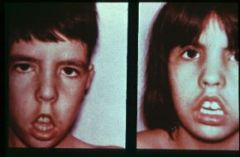
Hatchet mouth
|
|
|
What are some of the multisystem abnormalities that are present in myotonic dystrophy?
|
Cataract
Cardiac conduction defects/arrhythmia Testicular atrophy Early male baldness DM Mild/moderate mental retardation |
|
|
What's the pathogenesis of myotonic dystrophy?
|
Elongated trinucleotide repeat (CUG
RNA transcripts stop splicing, leading into problems with receptors, ion channels It's this that causes the multisystem problems |
|
|
What tests should you order if you suspect someone has myotonic dystrophy?
|
EMG (for myotonia)
Genetic testing |
|
|
How do you treat myotonic dystrophy?
|
It's supportive
If the myotonia is bad enough, you give drugs that effect their sodium channels |
|
|
What are some of the non-dystropic hereditary myopathies?
|
They all impact energy metabolism
Abnormal glycogen metabolism Phosphofructokinase deficiency Mitochondrial myopathies Channelopathies |
|
|
What causes problems in someone with abnormal glycogen metabolism?
|
They cramp with exercise,but they're fine at rest
|
|
|
What are the different kinds of abnormal glycogen metabolism?
|
McArdles: myophosphorylase deficiency
CPT deficiency Acid maltase deficiency |
|
|
How do you differentiate between McArdle's and CPT deficiency?
|
McArdle's: you get a 2nd wind becase you can use FFAs
CPT: the deficiency is in the utilization of FFAs, so you don't get a second wind |
|
|
What are the clinical features of acid maltase deficiency?
|
Weakness that slowly progresses
|
|
|
What other myopathy is similar to PRK deficiency?
|
McArdle's
|
|
|
What are the features of mitochondrial myopathies?
|
migraine
Ataxia Periodic paralyses |
|
|
What are the features of the channelopathies?
|
Periodic paralyses
Myotonic disorders |
|
|
Whatare some of the acquired metabolic myopathies?
|
Hypo, hyperthyroidism
Hyperparathyroidism CUSHING'S EXOGENOUS STEROIDS Chronic alcohol use |
|
|
What are some of the inflammatory acquired myopathies?
|
Dermatomyositis
Inclusion body myositis Polymyositis |
|
|
What are some of the clinical features of dermatomyositis and polymyositis?
|
Symmetric proximal muscle wasting, weakness
Gradual progression Pain is sometimes present, but not severe |
|
|
What findings are common in dermatomyositis?
|
Rash on the face and hands
|
|
|
What are the clinical features of inclusion body myositis?
|
Forearm flexors, knee extensors
Asymmetric Dysphagia Facial muscle involvement |
|
|
If you're young, what inflammatory myopathy do you get? After 50?
|
Kids: dermatomyositis
After 50: IBM |
|
|
If you're old and you've got dermatomyositis, what do you have to be concerned about?
|
SYSTEMIC MALIGNANCIES!
It's present in 10-20% of people with this guy |
|
|
What is the pathology that is present in the inflammatory myopathies?
|
-Segmental muscle fiber necrosis
-Muscle fiber regeneration -Mononuclear cell inflammation |
|
|
What's the difference between the pathology of polymyositis/IBM and dermatomyositis?
|
PM/IBM: cell mediated
DM: humoraaly mediate |
|
|
What are the changes that take place in the muscle fibers in IBM? What other disease processes show these proteins?
|
Vaculolar inclusions in the muscle fibers of beta amyloid, tau, TDP-43!!
Alzheimers, other neural diseases |
|
|
What tests should you order to make a diagnosis of the inflamamtory myopathies?
|
Blood levels: Increased CK
EMG: Myopathic changes, inflammatory characteristics MUSCLE BIOPSY IS GOLD STANDARD |
|
|
What kinds of inflammatory myopathies can you treat? What do you use?
|
DM, PM: prednisone
IBM you can't do anything for In all of them, give symptomatic treatment |

