![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
Candida
General Facts |
1. It colonizes most healthy individuals
2. Part of the normal flora 3. Candida albicans causes most Candida sp. infections |
|
|
C. albicans
Morphology |
Dimorphic (yeast cells or hyphae)
|
|
|
C. albicans
What is the confirmatory test? |
1. Germ Tube Test
2. Incubate yeast cells at body temp for 90 min and you should see hyphal growth. 3. Germ tube has different antigens that allow C. albicans to adhere to tube. |
|
|
C. albicans
Adherence Characteristics |
1. Readily adheres to plastic (catheters can be problematic)
2. Adheres to mucosal cells 3. Mech of attachment is the presence of integrin-like molecules that bind to extracellular matrix |
|
|
C. albicans
Problems for Infants |
1. Problematic if bacterial normal flora is not yet established
2. May develop oral thrush or severe diaper rash. |
|
|
C. albicans
Sites of common infection for adults |
Areas of excessive moisture and warmth
1. Opposing skin folds 2. Nail beds |
|
|
C. albicans
Factors that influence vaginal thrush |
1. Doubled risk with pregnancy
2. Antibiotic use increases risk 3. Oral contraceptive Anything disruptive of "balance" |
|
|
C. albicans
Factors that influence muscutaneous candidiasis |
1. Impaired cell-mediated immunity
2. Corticosteroid treatment 3. Any chronic illness or immunosuppressed state |
|
|
What is the most common systemic mycosis?
|
C. albicans (indwelling catheters)
|
|
|
What is the taxology of Pneumocystis jirovecii?
|
Heavily debated between a fungus and a protozoan
|
|
|
What are the reasons for classifying P. jirovecii as a fungus?
|
1. Morphological features
2. Ribosomal RNA sequences 3. Mitochondrial DNA 4. Chitin cell wall |
|
|
What are the resons for classifying P. jirovecii as a protozoan?
|
1. DNA content
2. Absence of highly conserved fungal EF-3 3. Susceptibility to anti-protozoan and not anti-fungal chemotherapeutics |
|
|
P. jirovecii
Replication |
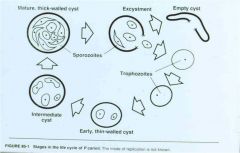
8 sporozoites in each cyst
|
|
|
P. jirovecii
Epidemiology |
1. Highly lethal in immunocompromised patients and premature infants
2. Latent infection 3. Opportunistic pathogen |
|
|
P. jirovecii
Clinical Manifestations |
"Pneumocystis"
1. Alveoli fill with cells, organisms, and fluid 2. Death is by progressive asphyxia |
|
|
Systemic Mycoses
General Characteristics |
1. Initial site of infection is the lung
2. These fungi are opportunistic pathogens 3. Given the opportunity infection will become systemic 4. In systemic infections, each fungus has a specific area it attacks 5. Restricted to geographical regions 6. Not normal flora |
|
|
Systemic Mycoses
What are the organisms responsible? |
1. Cryptococcus neoformans
2. Histoplasma capsulatum 3. Coccidiodes immitis 4. Blastomyces dermatitidis |
|
|
Histoplasma capsulatum
General Characteristics |
1. No capsule
2. Molds grow in high nitrogen soil (bird and bat droppings) 3. Birds not naturally infected; bats may be infected |
|
|
Histoplasma capsulatum
Growth |
1. Intracellular growth in phagocytic macrophages
2. Starts in lung; if becomes systemic, it can involve the reticuloendothelial system |
|
|
Histoplasma capsulatum
Geographic Endemic Areas |
Areas drained by the Ohio and Mississippi Rivers
|
|
|
Coccidioides immitis
General Characteristics |
1. Dimorphic fungus
2. Instead of yeast phaste, large distinct spherules appear in the lung which contain endospores 3. Most virulent of all human mycotic pathogens 4. Fungus grows best in arid soil enhanced by bat droppings |
|
|
Coccidioides immitis
Clinical Manifestation |
"Vally Fever" or "Desert Rheumatism"
1. Malaise 2. Cough 3. Chest pain 4. Fever (lasts 2-6 weeks) 5. Skin lesions from dissemination of primary infection in lungs Most cases resolve |
|
|
Coccidioides immitis
Geographic Endemic Areas |
1. Most geographically restricted
2. Fungus routinely isolated from soil. 3. Arizona, Nevada, New Mexico, western Texas, and southern California |
|
|
Cryptococcus neoformans
Epidemiology |
1. Found worldwide in pigeon droppings and in soil contaminated with them
2. Birds are not infected. |
|
|
Cryptococcus neoformans
Diagnostic test |
Encapsulated yeast from India ink preparation is an approach used to diagnose an infection
|
|
|
Cryptococcus neoformans
Clinical Manifestations |
1. Most common cause of fungal meningitis
2. Cryptococcal meningitis 3. Detection of antigens in cerebrospinal fluid 4. Gives severe headache 5. Skin lesions may result from dissemination of yeast |
|
|
Blastomyces dermatitidis
Epidemiology and Characteristics |
1. Limited to North America and parts of Africa
2. May cause skin lesions if systemic infection develops 3. Dogs are susceptible to infection |
|
|
Aspergillus species
Characteristics |
1. Source of nosocomial infections
2. Often found in ventilation ducts 3. Colonization in lung can lead to extensive growth and invasion of other tissues 4. Forms fungus ball that requires surgical removal |
|
|
Zygomycosis
Characteristics |
1. Abundant in environment
2. Blood vessels, eye, CNS, nose, sinuses, and lungs are most commonly involved 3. Predisposing factors: immunosuppression 4. Represents a serious nosocomial infection |
|
|
What are the 2 basic morphologic forms of Fungi?
Briefly Describe them... |
1. Yeast - UNICELLULAR growth form of fungi (reproduce by budding and fission)
2. Molds - MULTI-CELLULAR hyphal growth by apical elongation (involves production of multicellular, filamentous colonies) 3. Fungi can grow in both forms (Dimorphism) |
|
|
What composes the CELL WALL of Fungi?
|
1. Chitin - a target of anti-fungal drugs (ECHINOCANDINS, NIKKOMYCIN)
*analogous to PG layer of bacteria* |
|
|
Name 4 reasons CHITIN is medically important in fungal infections...
|
1. Mediates attachment
2. Promotes colonization and invasion 3. Promotes antigens 4. Mammalian tissues lack enzymes to degrade chitin |
|
|
Name the UNIQUE plasma membrane lipid in fungi...
|
1. ERGOSTEROL - we use this to target and kill fungi (target of AZOLES, ALLYLAMINES)
*cell membranes are in lipid-bilayer format* |
|
|
How do fungi acquire nutrients?
|
1. they DO NOT engulf their nutrients
2. bacteria SECRETE DIGESTIVE ENZYMES and ABSORB their nutrients |
|
|
Name the MAIN components of POLARIZED GROWTH of hypha...
|
1. Enzymes arrive in vacuoles
2. Rigid cell wall is degraded 3. Other vacuoles arrive with "rebuilding" enzymes 4. Growth in ONE direction **budding in yeast cells use similar concept** |
|
|
Name the MAIN TYPES of FUNGAL DISEASES...
|
1. Allergies - simply an allergic reaction to fungal spores **NO GROWTH OF FUNGUS NEEDED**
2. Mycotoxicoses - Toxins like AFLATOXIN (A. flavus) and AMATOXINS from mushrooms 3. Superficial Mycoses - (details covered on separate flashcard) |
|
|
Name 4 characteristics of SUPERFICIAL MYCOSES...
|
1. noninvasive
2. outermost layer of the skin 3. colonize NONLINING tissue 4. NO IMMUNE RESPONSE |
|
|
Name 4 SUPERFICIAL MYCOSIS clinical manifestations...
|
1. Pityriasis versicolor - found in areas with sweat glands; results in hyper/hypopigmented macular lesions.
2. Tinea nigra - CAN BE CONFUSED WITH MELANOMA; black macular lesions on palms/soles 3. Black piedra - DARK fungus on SHAFT of hair follicle 4. White piedra - WHITE fungus on hair SHAFT |
|
|
Name 5 characteristics of CUTANEOUS MYCOSES...
|
1. **Caused by DERMATOPHYTES** TQ
2. Restricted to KERATINIZED LAYERS (skin and nails) 3. IMMUNE RESPONSE INVOLVED (this determines the severity) 4. Can be of geophilic, zoophilic, or anthrophilic origin 5. Referred to as "ringworm" |
|
|
What are the 3 main genera of DERMATOPOHYTES relating to cutaneous mycoses and what are their targets?
|
1. Trichophyton
2. Microsporum 3. Epidermophyton **they can infect MORE THAN ONE site (scalp, hair, skin, or nails) |
|
|
What clinical manifestation is associated with Tinea pedis?
|
1. Athlete's foot
|
|
|
What clinical manifestation is associated with Tinea cruris?
|
1. Jock itch
|
|
|
What clinical manifestation is associated with Tinea corporis?
|
1. Simply a Tinea infection on the body
|
|
|
What clinical manifestation is associated with Tinea barbae?
|
1. Tinea infection of the BEARD
|
|
|
What clinical manifestation is associated with Tinea capitus?
|
1. Tinea infection of the head (site of hair loss)
|
|
|
Tinea capitus caused by Microsporum canis causes hair loss. Why is this so and what is the site of hair loss called?
|
1. Severe inflammation of the hair follicles causes the hair loss
2. Kerion - site of hair loss |
|
|
How would you diagnose a fungal disease?
|
1. Scrape and KOH preparation
|
|
|
Name 3 characteristics of SUBCUTANEOUS MYCOSES...
|
1. Infection usually from soil/vegetation
2. A lesion usually develops at site of trauma 3. infection is DEEPER than the layer of the DERMIS (can go into muscle or bone) |
|
|
What is one of the most clinically relevant SUBCUTANEOUS MYCOSES (Lymphocutaneous sporotrichosis) ?
|
1. Sporothrix schenkii - causes Lymphocutaneous sporotrichosis
|
|
|
What are the typical clinical presentations of in infection with Sporothrix schenkii?
|
1. You should observe lesions along the lymphatics draining the primary lesion
|
|
|
Where would one be more likely to be infected with Chromoblastomycosis? How do you treat it? Outcome?
|
1. Tropics
2. Surgery 3. You have it for life |

