![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
What % of muscle mass is made up from muscle? |
40% |
|
|
What percentage of body water is contained in muscle? |
80% |
|
|
What are 2 important (non-motor) functions of muscle? |
1. Store for intracellular ions e.g. potassium.
2. Important for heat production. |
|
|
What are the features of skeletal muscle? |
It is made up of multinucleate cells. 10cm in length 10-100um Nuclei are located peripherally. |
|
|
What are the feauters of the NMJ? |
NMJ is an interface between the axon of the motor neurone and the muscle fibre.
Action potential propagates along the motor axon via saltatory conduction due to myelinated neuron. Depolarisation opens voltage gates ca2+ channels, ca2+ influx results in vesicles of Ach being released. Ach diffuses across the synaptic cleft - binds to Ach receptor sites on Na+ channels. these open releasing Na+ which propagates along the neurone. (Acetylecholinesterase breaks down Ach) |
|
|
What are the phases of muscle contraction? |
1. Latent period.
2. Period of contraction.
3. Period of relaxation. |
|
|
What is the key difference in muscle contraction between the muscles: gastrocnemius, extraocular muscles and soleus? |
All contract in response to a single stimulus.
the percenatage of maximum tension reached is the same.
but the extraocular muscle contrasts faster and for less time- contraction and relaxation period are short.
gastrocnemius and soleus - contrast slower and have a much longer period of contraction and relaxation (soleus is the longest). |
|
|
What are the 2 different types of muscle fibres? |
Slow type 1 Fast type 2. |
|
|
What are the relative compositons in an average person? |
50:50 |
|
|
What are the %s after spinal injury? |
4:96
(i.e. way more fast). |
|
|
What are the %s in a couch potato? |
40:60 |
|
|
What about in a sprinter? |
20:80 |
|
|
What are the %s in a marathon runner? |
80:20 |
|
|
What is the general patter in proportion of muscle fibres? |
Spinal injury- have way more fast fibres, same in an inactive individual and a sprinter.
In a marathon runner they have fast more slow type 1 fibres- allowing sustained contractions.
Normal person has equal amount of them both. |
|
|
What is the result of loss of innervation in an adult to a muscle? |
Muscle fibres will be small and angulated.
Indicates that a single motor neurone is damaged. |
|
|
What determines the muscle fibre type? |
The fibre type is determined by the primary motor neuron. |
|
|
What happens when a muscle fibre is denervated? |
the remaining motor axons will sprout to innervate denervated fibres. motor units enlarge. fibres become grouped.
(if these motor neurones die group atrophy occurs) |
|
|
What are the feature of infantile hypotonia? |
Decreased muscle tone. Floppy infant.
Most fibres are small and round with a few massively hypertrophic fibres. |
|
|
What is the abnormalitiy in muscle fibres in infantile hypotonia? |
Large type 1 muscle fibres are normally paler, and small type 2 are normally darker.
in infantile hypotonia: there is a congenital fibre type disproportion: small fibres are the type 1 fibres whereas the type 2 fibres are normal to larger in diameter. (i.e. sizes switch) |
|
|
What are the symptoms of a muscle disorder? |
Pain and weakness Tenderness, twitching and cramps. Muscle wasting and contractures. |
|
|
What conditions/factors are related to muscle disorders? |
Neurological symptoms e.g. primary muscle, secondary to peripheral nerve damage.
Connective tissue disorders Family history Drug exposure Endocrine disorders. |
|
|
Name 2 infalmamtory myopathies: |
Polymyositis Dermatomyositis |
|
|
What are the associations with inflammatory myopathies? |
Ass with microbial infection. Autoimmune
|
|
|
What is the key feature of inflammatroy myopthaties? |
Proximal muscle weakness |
|
|
What is the incidence? |
5-10 million cases per year. 2:1 prevalence in females. 40-60 peak indicence. |
|
|
What ar ethe clinicla features? |
Symmetrical involvement of the large proximal muscles of the shoulders, arms and thigh.
Serum creatine kinase is elevated.
EMG; typical irritability is 90%.
|
|
|
What is the most definitive diagnostic too;? |
Biopsy: variation in fibre size, central nuclei, necrosis and regeneration, infiltrate of inflammatory cells. |
|
|
Zooming in on a biospy, what is seen? |
Lymphocytes surround and invades the individual muscle fibres = CD8+ T lymphocytes. some macrophages to remove necrotic fibres. |
|
|
What is a dermatomyositis rash? |
It is a rash that is purplish in colour and often has a streaky pattern.
Heliotrope rash over the eyelids with oedema.
|
|
|
Where are subcutaneous calcifications seen? |
In autoimmune connective tissue disease.
ANA positive in 90% of cases. Anti-Jo1 antibody in 20-40% of cases.
- these calcifications are in muscles and under the skin. |
|
|
How are inflammatory myopathies treated? |
1. Corticosteroids: high dose 1mg/kg prednisone per day. maintain until creatine kinase is normal. if stopped early flares will be hard to control.
Azanthioprine Methotrexate |
|
|
What is the 5 and 8yr surival? |
80% and 73% |
|
|
What are the causes of death? |
Malignancy, infection and pulmonary involvement |
|
|
In what circumstance is death more liekly? |
if Anti-Jo1 positive. |
|
|
What is the most common muscle disease of the elderly? |
Inclusion body myositis.
-characterised by muscle weakness: -fingers and wrist flexors more than extensors and shoulder abductors. -knee extensors more than hip flexors.
PLUS -loss of quads reflex -dysphagia -ass. polyneuropathy |
|
|
In who is it most common? |
More common in males.
(see mild elevation of creatine kinase levels). |
|
|
What is the prognosis? |
Poor. |
|
|
What are the features on biospy? |
Vaculoes contain amyloid like material (congo red colour) |
|
|
What are the properties of the filamentous inclusions of IBM? |
Have optical properties: of amyloid, and contain beta amyloid, hyperphosphorylated tau and apolipoprotien E, presenlin 1, prion protein and other proteins. 1. beta amyloid 2. hyperphosphorylated tau 3. apolipoprotein E 4. Preselin 1 5. Prion protein.
|
|
|
What are muscular dystrophies? |
They are progressive genetically determined degenerative myopathies.
X-linked, AR or AD. |
|
|
Name 3 X-linked dystrophies: |
1. Duchenne and Becker muscular dystrophy.
2. Limb girdle muscular dystrophy.
3. Emery-Dreiffus |
|
|
Which 2 of these are also AR? |
1. Limb girdle 2. Emery-Deiffuss |
|
|
Name 4 AD muscular dystrophies: |
1. Facioscapulohumeral. 2. Oculopharyngeal
Plus 3. Limb girdle. 4. Emery- Dreiffus. |
|
|
Describe the mechanism of damage in muscular dystrophies: |
ss |
|
|
Describe which areas of the body are affected by different msucular dystrophies: |
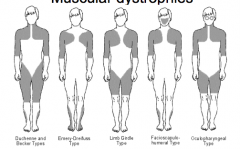
Grey = affected area. |
|
|
What are the Becker types of dystrophy? |
Less severe and slower progressing forms of Duchenne musucalr dystrophy. |
|
|
What is the incidence of Duchenne MD? |
20-30 cases per 100,000 MALES per year. |
|
|
What are the clinical features? |
Proximal muscle weakness during the first 2 years of life.
Continuous slow decline- unable to walk by 7-12 years. Death usually by mid-late teens.
CK elevated. |
|
|
What are the biopsy feature of DMD? |
FIbre size variability Endomysial fiborosis. Degenerating muscle fibres undergoing myophagocytoiss. |
|
|
What happens to the muscles later on- on biospy? |
later the muscle is replaced with fibrotic material and fat. |
|
|
What 3 drugs can induce myopathies? |
1. Corticosterioids. (fluorinated steroids dose dependent) type 2 fibre atrophy.
2. Statins: approx 10% of patients. rhabdomyolysis.
3. Alcohol- chronic slow proggressive proximal weakness. actue - single heavy session. |
|
|
What is fibromyalgia? |
Widespread muscle pina
Both sides of the body above adn below the waist are effected in axial skeleton.
Combo of 11 out of 18 speicifc tender points.
Antipolymer antibodies: 50% of pts positive.
Ass fatigue and sleep disturbances. 30-60 year old age group. 80-90% of patietns female. |
|
|
What is teh cycle of fibromyalgia? |

|
|
|
What are the co-morbid conditions? |
Sytemic: Pain, weight gain, cold symptoms, multiple chemical sensitivity. Skin- various Musucalr- fatigue, twitchiness Urinary problems, Joint- morning stiffness Central- chronic headaches, dizziness, memory impariment, depression/anxiety etc. |
|
|
What are the 4 key treatment options? |
1. Tricyclic antidepressants : amityiptyline.
2. SSRIs : fluoxetine
3. Exercise
4. Complementary therapy. |

