![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
MS
|
• Chronic inflammatory demyelinating disease of the CNS
|
|
|
MS epidemiology
|
• Most common cause of neurological disability in young adults
• Prevalence ~70/100,000, F:M 2.6:1, average age onset 34 yrs |
|
|
Aetiology
|
• Unknown cause:
– Genetic factors • MZ vs DZ twins (30% MZ vs 5% DZ) • HLA-DRB1*1501 – Environmental factors • Latitudinal gradient • ?? Sunlight/age exposure to viruses • Increasing prevalence and incidence |
|
|
Clinical Course
|
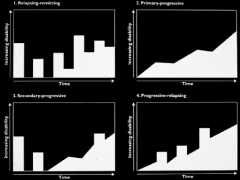
1. RR (80%)
2. PP 3. SP 4. PR - benign or no progress between attacks |
|
|
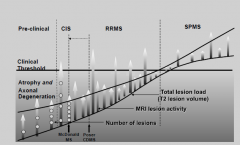
Clinical Threshold
|
|
|
|
Clinical MS
Sx at onset |
• Characterised by dissemination of lesions in space and time
• Classification by disease course • Typical symptoms at disease onset – Weakness – optic neuritis – sensory symptoms – unsteady gait – Vertigo – double vision – sphincter disturbance • Tempo of symptom onset and offset |
|
|
Clinical MS:
relapses |
– Majority recover in early disease (resolution of acute inflammation, resolution of conduction block remyelination)
– Incomplete recovery may lead to stepwise accrual of disability REMYELINATION ability is there if the axon is intact but in MS they gradually loss this ability to repair |
|
|
Secondary progression
|
– Gradual decline in function between attcaks
– Occurs in the majority of patients with a relapsing presentation – Correlates with axonal loss |
|
|
Sx in estabilsed disease
|
– motor : UMN weakness, spasticity
– sensory : paraesthesiae, sensory loss, pain, Lhermitte’s – cerebellar: incoordination, intention tremor, gait ataxia, dysarthria – ophthalmological : optic neuritis, diplopia, nystagmus, INO – sphincter disturbances: urgency, frequency, incontinence, constipation – sexual disturbances : loss of libido, impotence – psychological disturbances : depression, cognitive dysfunction |
|
|
Motor Aspect of MS
|
– Main initial complaint in 50%
– Uhtoff’s: feebleness after exercise or exposure to heat – Parapareses or hemipareses: subacute onset or slowly progressive – Spasticity (the cause of much disability) • Central disinhibition of myotatic reflex arc • Worse in legs than arms • Extensor spasticity may aid standing and walking • Gait affected - simultaneous activation agonist /antagonist • Flexor spasms: falls without warning, may be painful • Extensor spasms • Adductor involvement affects sphincters |
|
|
Sensory Aspects of MS
|
– Numbness (limbs or face): the most frequent early complaint
– Paraesthesiae / dysaesthesiae – Sense of swelling or constriction around limbs (dorsal column) – Sense of constricting band around trunk (spinal) – Impaired JPS/useless hand: plaque in dorsal column (cervical) – Lhermitte’s phenomenon: plaque in cervical cord – Trigeminal neuralgia – Painful tonic spasms – Shooting paroxysms of extremities |
|
|
Ophthalmological in MS
|
– Optic neuritis
• Common early symptom • Blurred vision or visual loss in one eye • Pain on eye movement or pressure on eye • Vision improves over days to weeks. Some impairment of colour vision may persist. • Swelling of disc only in anterior lesions • Visual field examination shows central or paracentral scotoma (red target) • Optic atrophy – Binocular diplopia: brain stem lesions – Nystagmus: horizontal, torsional, pendular • Association with head tremor, truncal ataxia • Internuclear ophthalmoplegia: lesion in MLF |
|
|
Prognosis
|
– Highly variable
– No reliable predictor at disease onset – Benign course more likely if • early age onset • rapid remission of initial symptoms • monosymptomatic onset • long period to second relapse • minimal pyramidal and cerebellar deficits in first five years – 50% will need assistance with walking after 10 yr – Over 1/3 able to work full time, 2/3 part-time 5 yr after onset – One quarter work full time after 10 yr – Mean survival of 30 yr after onset (longer in modern era- approx normal lifespan) |
|
|
MS pathogenesis
|
- white matter demyelination and grey matter disease due to loss of axons
- may be a problem initially with the oligodendrocytes NOT JUST Th1 cells • Lymphocytes may be absent from early lesions • Cuffs may be present in NAWM in MS • CD8+ > CD4+ cells, clonally expanded • Polar capping of IgG in macrophages • Ig/complement products on myelin sheaths • Plasma cells ++ in subacute plaques • ? Benefit of PLEX/IVIg/RTX |
|
|
Natalizumab
|
Ab blocks the entry of Tc into the CNS (across BBB)
- most effective MS Tx - however leaves the brain with no cellular immunity thus more risk of infection |
|
|
Myelination of CNS and PNS
|
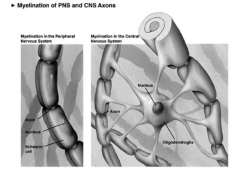
thus one dead = lots of myelin gone
|
|
|
Pre and Post Phagocytic Lesion
|

|
|
|
MRI
|
• High signal intensity (bright) lesions on T2/FLAIR sequences
• Typical Distribution: – bordering lateral ventricles – corpus callosum – brain stem, cerebellum – spinal cord • Typical morphology: globular, radial orientation from cc • Gd enhanced lesions (‘active’) indicate current sites of inflammation, BBB breakdown • T1 black holes correlate with progression, axonal loss • ***UBOs: white matter lesions carry a DDx*** |
|
|
MS Dx
|
1. at least one Gd enhancing lesion (means a new or active lesion in the past 2wks) OR 9 T2 non-Gd lesions
2. at least one infratentorial lesion 3. at least one juxtacortical lesion 4. at least 3 periventricular lesions |
|
|
CSF in MS
|
Protein level:
• mildly raised in 30% (rarely above 1.0 g/L) • Cell count: • usually normal, may be raised in attack, rarely >50 cell / mm3. • Gamma Globulin: • CSF IgG index > 0.7 in 90% • CSF oligoclonal IgG present in 90% |
|
|
Oligoclonal Bands in MS
|

• CSF oligoclonal IgG present in 90% (thus if absent strong evidence against MS)
- predominately IgG1 |
|
|
Electrophysiological Tests in MS
|
eg right eye delay 10m/s indicating optic neuritis
- thus most insult at the mylein |
|
|
MS Differentials
Polysymptomatic |
• Monophasic
– ADEM • Monophasic or Relapsing – Autoimmune • SLE / Antiphospholipid syndrome • Primary Sjogrens disease – Sarcoidosis – Behcet’s disease – CNS Vasculitis – CADASIL – Cerebral lymphoma – Mitochondrial disease – Chronic CNS Infections |
|
|
MS Differentials
Monosymptomatic |
• Spinal cord syndromes
– Chronic • Compression • Chiari • Spinal Dural AVM • HTLV-1 • Primary lateral sclerosis – Acute • Compression • Spinal cord stroke • Transverse Myelitis (can be relapsing) • Infective myelitis • Visual loss – AION – LHON – Central serous chorioretinopathy – CRION – Paraneoplastic optic neuropathy – Neuroretinitis – Autoimmune (lupus, Sjogrens) optic neuropathy • CPM |
|
|
Multiple Sclerosis Medical Therapy
|
1. ACUTE for relapses:
IV methylprednisolone plasma exchange IVIG 2. immunomodulatory Tx 3. Symptomatic and adjunctive Tx - Spasticity: physio/baclofen/tizanidine/botox/cannabinoids - pain - depression - fatigue - sphincter dysfunction |
|
|
Traditional Immunotherapy
|
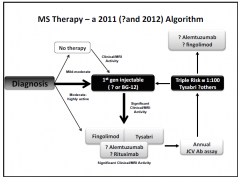
- interferon b1b,b1a
glatiramer acetate |
|
|
MS overview
|
1. irrevesible axonal injury occurs in the newly forming MS lesion
2. inflammation predominates early in the disease and significantly contributes to axonal injury 3. recuirtment of systemic immune cell pools to the CNS predominates in early disease 4. The inflammatory response is progressively compartmentalised and therefore inaccessible to traditional immunomodulatory therapies |
|
|
Fingolimod
|
S1P1 receptor agonist, internalising the receptor thus blocks emigration of lymphocytes on LN, BUT doesnt impair immune surveillance
|
|
|
Alemtuzumab
|
Binds CD52 on Tc, monocytes, long term depeltion
|
|
|
Oral fumaric acid
|
protects oligo and neurons from inflammatory & metabolic injury
|
|
|
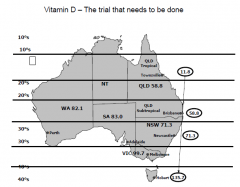
Vit D
|
|
|
|
Myelin Function
|
- allows saltatory (leaping from one Node to the next) conduction
- one oligodendrocyte myelinates upto 40 axons |
|
|
Classification of myelin disorders
|
•
Primary demyelination – Damage to oligodendrocyte cell body or myelin sheath • Secondary demyelination – Damage to axon, with secondary loss of myelin • Dysmyelination – Abnormal formation of myelin |
|
|
Relapsing-remitting MS
|
•
Typically begins in early adulthood • Twice as common in women – Appears to be increasing in women – Women more likely to relapse than men – Risk of MS in women low when vit D levels high • Variable prognosis • 50% of patients will need help walking within 15 years • Average survival 30 years |
|
|
Relapsing-remitting MS Clinical features
|
•
Common signs – Optic neuritis – Sensory disturbances – Diplopia – Limb weakness – Ataxia – Neurogenic bladder • Symptoms may worsen with heat • Cortical signs usually not dominant |
|
|
Lesion sites
|
–
Periventricular regions – Optic nerve – Brain stem – Cerebellum – Spinal cord |
|
|
Axonal Loss in MS
|
–
High incidence of acute axonal loss in lesions during active myelin destruction – Low level of continuous axonal destruction in chronic plaques |
|
|
Progressive MS
|
•
Can be primary or secondary to relapsing-remitting MS • Axonal loss important • Can monitor axon loss over time with optical coherence tomography • Serum levels of complement factor H are higher in secondary progressive than relapsing-remitting MS (could be a useful biomarker) |
|
|
•
What is the cause? |
•
Genetic • First degree relative studies show genetic effect •Monozygotic 30% concordance, dizygotic 3% (similar to non-sibs risk) •MS susceptibility is associated esp. with the class II region of the MHC – e.g. rare variant • Environmental – e.g. virus • Gene-environment interaction |
|
|
MS Epidemiology
|
•
Prevalence varies around the world • Prevalence increases away from the equator – Genetic or migration effect? • Lack of sunlight/vitamin D • Exposure to some agent when young? |
|
|
EBV in MS
|
•99% seropositive in MS, 90% in controls
•Later age of infection (“hygiene” hypothesis) with MS 10 years later •EBV resembles some myelin proteins (“innocent bystander”) |
|
|
MS: Common hypothesis
|
•
An immune-mediated disorder in genetically susceptible people • Activated, autoreactive T cells within the lesions drive the chronic inflammatory process and activate local or hematogenous macrophages that destroy myelin • However, there probably are various pathological mechanisms, and different patients have variable plaque structure and immunology |
|
|
Disruption of BBB by T cells
|
•
Autoreactive T cells penetrate the blood-brain-barrier • alpha4-integrin (expressed on surface of T cells) mediates adhesion with endothelium • BBB may be disrupted by environmental and/or genetic factors • Local factors may upregulate endothelial adhesion molecules to facilitate T cell entry • Perivascular T cells are also seen in retina, which has no myelinated axons (suggests endothelial injury is a primary event) |
|
|
Activated T cells
|
•
Stimulate type 1 helper (Th1) T cells – Macrophage activation (via gamma-IF) – Destructive cytokines • Stimulate type 2 helper (Th2) T cells – B cell activation produces antibodies • Stimulate CD8 cytotoxic T cells – Direct injury |
|
|
Myelin damage
|
•Damage to myelin
–Macrophages –Macrophages + antibody –Antibody + complement –Cytokines •Damage to oligodendrocyte cell body –CD8 cytotoxic cells –Antibody + complement –Cytokines |
|
|
Remyelination in MS
|
•
“Shadow” plaques • Remyelination may be spontaneous from surviving oligodendrocytes • New oligodendrocytes may proliferate from progenitor cells • Spread of sodium channels from node of Ranvier can restore conduction early |
|
|
MS treatments I
|
•Decrease T cells
–Deplete circulating T cells –Vaccinate against T cells –Whole body irradiation and replacement of T cells –New oral agents (e.g. terifluonamide which blocks the proliferation of rapidly dividing lymphocytes) •Prevent inflammatory cell vascular adhesion and migration –Anti-alpha4 integrin agents (oral agents now available, possible side effect of PML) •Blood-brain-barrier –Transiently restore with corticosteroids •Block TCR/antigen/class II MHC interaction (glatiramer) •Multiple actions –Interferon ß: reduces MHC II expression, proliferation of T cells, TNF production •Antibodies –Remove antibodies with plasma exchange •Remyelination –Stimulate or prevent death of oligodendrocytes with growth factors –Oligodendrocyte transplantation/stem cells |

