![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
Describe the histological structure of cortical bone
|

- Cortical bone is a series of Haversian systems.
- The space between the Haversian systems is filled with bony lamellae called interstitial lamellae. - Extended around the bone are outer circumferential lamellae. - Each Haversian system consists of concentric lamellae of bone laid down around a central canal and contains blood vessels and collagen fibres in regar form. - Bone surrounded by periosteum. - The periosteal blood vessel runs transversely across the bone in Volkmann’s canal and gives rise to the vessel which runs along the long axis of the bone within the Haversian canal. - Osteocytes sit in lacunae within the lamellae of the haversion systems |
|
|
What does bone develop from?
|
- All the skeletal system (bone, cartilage & joints), develops from mesenchyme
i.e. undifferentiated embryonic connective tissue - Mesenchyme can take on the appearance of spindles or stellate cells |
|
|
What stimulates bone development?
|
- Response to external micr-environment signals and internal linage signals = not well understood
- May be due to cytokines or growth factors |
|
|
Describe the process of intramembranous ossification
|
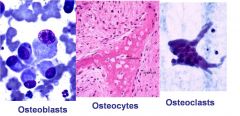
- This method of bone development involves the laying down of bone tissue directly in the primitive connective tissue or mesenchyme = No cartilage pre-cursor
- Flat bones of skull, parts of temporal bone, mandible and maxilla form this way - Develops in a layer of mesenchyme between the brain and the scalp. - Process: 1. Mesenchyme condenses and is highly vascular 2. Mesenchymal cells differentiate into OSTEOBLASTS = do not divide and transform into osteocytes 3. Matrix secretion – OSTEOID = synthesis matrix • Type 1 Collagen • Proteoglycans • Glycoproteins • Alkaline Phosphatase (detect this in blood when there is a high bone turnover as well as in liver disease) 4. Bone osteoblasts trapped – mature into OSTEOCYTES • Encased in matrix • Lie in lacunae • Communicate through canaliculi • No cell division 5. Remodelling - OSTEOCLASTS • Bone resorption = secretes acid and proteases to resorb underlying bone • From monocyte-macrophage system • Multinucleated = up to 50 • Resorption craters – ‘Howship’s Lacunae’ • Osteoclastic & osteoblastic activity linked • Woven bone organised into layers = lamellae • Concentric lamellae form Haversian systems |
|
|
Describe the process of endochondral ossification
|
- Bone formed from pre-existing cartilage model
- Long bones, vertebrae, ribs and pelvis - Process: 1. Chondrocytes undergo hypertrophy and secrete extracellular matrix which calcifies resulting in chondrocyte cell death 2. Osteogenic buds invade the dead cartilage - blood vessels bringing osteogenic cells. Osteoblasts develop which secrete more matrix which in turn becomes mineralised 3. Gradual replacement of cartilage by woven bone 4. Perichondrium becomes the periosteum. Note a few mesenchymal cells deep to the perichondrium undergo intramembranous ossification |
|
|
Describe the process of long bone growth
|

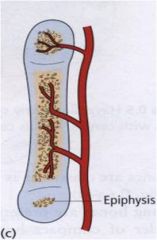
- Primary ossification centre:
• Primary Ossification Centre expands longitudinally in DIAPHYSIS • Increased growth of Periosteal Bone Collar = intramembranous ossification • By 6th months resorption of central part results in the formation of a medullary cavity • Immature woven bone gradually replaced by lamellar bone - Secondary ossification centre • Develops in the cartilage at the ends of the long bones; EPIPHYSES • At birth secondary centre in femur; others appear in cartilaginous epiphyses at varying ages after birth (c.f. bone age) • No perichondrium in the area of articular cartilage and so no periosteum in this area. - Epiphyseal cartilage • Located between the metaphysis and the epiphysis • Known as the EPIPHYSEAL PLATE • Provides growth in length of a long bone by growth of cartilage • Proliferation balances destruction = composed of a number of zones where the chondrocytes are in different phases: 1. Resting zone 2. Proliferation zone 3. Hypertrophic zone 4. Provisional calcification 5. Ossification zone • Very sensitive to growth hormone, thyroid hormones and sex hormones. Oestrogen particularly has a major role in the fusion of growth plates, so if insensitive can grow very tall |
|
|
Describe the process of fracture healing in cortical bone
|
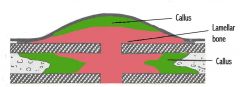
1. Haematoma
- Bleeding of canaliculi and nutrient and periosteal arteries - Forms between fracture ends and under the periosteum - Necrosis of bone closest to the # as no new blood supply 2. Inflammatory reaction and invasion - Macrophages invade and remove and avascular bone around the fracture (#) site - Ingrowth of granulation tissue into the haematoma = myofibroblasts - Osteogenic cells proliferate from the periosteum 3. Callus formation - Clost the the # site osteogenic cells differentiate into chondrocytes and islands of cartilage laid down which is soft and radiolucent - Osteogenic cells further from the # site differentiate into osteoblasts and produce woven bone - Callus imparts rigidity to fracture and provides suppoty - Appears on X-ray as a distinct irregular swelling 4. Consolidation - Cartilaginous components of the callus are gradually replaced by bone through endochondrial ossification - When the # callus becomes sufficiently firm that movement no longer takes place at the # site it is “clinically united" = radiographic union - However much more needs to be done before the bone is restored to its original strength 5. Remodelling - Primary callus is gradually replaced with more mature lamellar bone - Reshaping by osteoclasts and osteoblasts of lamellar bone into appropriate form related to function. - Excessive callus resorbed & medullary cavity re-established - Shape responds to stresed on the bone |
|
|
Describe fracture healing in cancellous bone
|
- Sponge like lattice of trabeculae & surrounding shell of cortical bone
- Rich blood supply → Little necrosis of bone - Endosteal callus rather than periosteal - Osteogenic cells from the endosteum produce woven bone - Woven bone replaced by lamellar bone - Internal remodelling |
|
|
What are the 2 main requirements for bone repair?
|
1. Stability of the fracture
2. Vascularity Also enough mineral supply |
|
|
Name 3 ways that bone repair may be delayed
|
1. Movement of bone ends
2. Poor blood supply 3. Infection |
|
|
Define malunion
|
Fracture heals in normal time but with an unsatifactory position
|
|
|
Define delayed union
|
Fracture heals but takes considerably longer to do so
|
|
|
Define non-union
|
Fracture fails to heal by bone, resulting in formation of a fibrous union or pseudoarthrosis
|
|
|
What are the 3 types of cartilage?
|
1. Hyaline = Type II collagen, found on articular surfaces, respiratory tract and costal cartiliage. Compressible
2. Elastic = Type II collagen and elastin e.g. external ear and epiglottis 3. Fibrocartilage = type I collage e.g. pubic symphysis, intervertebral joints, other places where little movement is required |
|
|
Describe the formation of cartilage
|
- Chondroblasts: immature cells that synthesise matrix
- Chondrocytes: mature cells that occupy lacunae - Extracellular matrix: • avascular • collagen • elastin • ground substance |
|
|
Define non-union
|
Fracture fails to heal by bone, resulting in formation of a fibrous union or pseudoarthrosis
|
|
|
What are the 3 types of cartilage?
|
1. Hyaline = Type II collagen, found on articular surfaces, respiratory tract and costal cartiliage. Compressible
2. Elastic = Type II collagen and elastin e.g. external ear and epiglottis 3. Fibrocartilage = type I collage e.g. pubic symphysis, intervertebral joints, other places where little movement is required |
|
|
Describe the formation of cartilage
|
- Chondroblasts: immature cells that synthesise matrix
- Chondrocytes: mature cells that occupy lacunae - Extracellular matrix: • avascular • collagen • elastin • ground substance |
|
|
What is heterotrophic ossification?
|
The pathologic formation of bony tissue in a location where bone does not normally form, eg within muscle
|

