![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
10 Cards in this Set
- Front
- Back
|
Monitoring depth of anaesthesia
|
Electrical cortical activity decreases with increasing depth of anaesthesia
- Bispectral indec: 0 isoelectric - 100 awake Used in human Not used in vet - spp differences and varies w anaesthetic |
|
|
How could you measure CV function?
|
1. ECG - r. cheap, non-invasaive, easy to use monitor - records electric activity of heart, allows diagnosis of arrhythmia NO info on mechanical function of heart or cardiac output HR may not be accurate - may count T waves as well as QRS complex 2. BP monitor Arterial pressure = Qt(cardiac output) x SVR(systemic vascular resistance -> Indirect BP measurement a) Oscillometric - cuff around tail/distal limb b) Doppler - ultrasounds placed over peripheral limb / tail artery and detects flow -> audible signal - useful indication of mechanical cardiac activity (esp. v. small animal). Cuff attached proximal to probe -> systolic BP -> Direct BP measurement (invasive) a) Arterial - accurate & continuous systolic, mean and diastolic BP. Monitor will also give HR (based on mechanical activity) -> arrhythmia. Uses intra-arterial catheter -> BP on screen. Routine use in horse and cow under inhalant anaesthesia. Risks - sepsis/haematoma, thrombus formation. Subjective info on SV and contractility can be obtained from pressure waveform b) Venous - Measures directly central venous pressure via a long cannular placed in jugular v. |
|
|
Measuring pulse oximetry - what info do you get? - how do you do it? - what affects the results? |
Probe placed on peripheral tissue measures % of Hb saturated with O2 in that tissue. - tongue, ear, toe, prepuce, vulva - also rectal and nasal mucosa large animal Probe emits and receives IR light - difference in absorption between the 2 wavelengths determines amount of oxy-&deoxyHb present (more oxy in systole). Monitor displays HR, %O2 saturation (SpO2) and a trace or plethysmograph indicating signal intensity. When pulsatile trace is present indicates mechanical functioning of heart Results effected by: - vasoconstriction - compression of tissue by probe - movement - pigmented/hairy skin - ambient light - pathological forms of Hb (MetHb, CO-Hb) - IV dyes |
|
|
Core-periphery temperature difference - how? - what does it tell you? - normal value? |
Thermistors placed peripherally (lip) and centrally ( oesophagus)
Normal gradient 2-4 degrees C Indicative of peripheral perfusion |
|
|
Methods of measuring respiratory function
|
2. Capnography 3. Pulse oximetry 4. Arterial blood-gas analysis |
|
|
Apnoea monitor - how does it work? - what does it tell you? |
Gives no indication of adequacy of ventilation May be misleading, can also be affected by chest movements induced by external forces (e.g. scrubbing chest wall) |
|
|
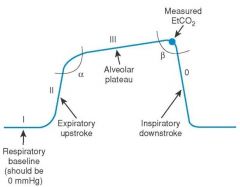
What does capnography measure?
|
Tidal volume needs to be large enough to allow gases to reach sampling site. In normal conditions EtCO2 is related to arterial CO2 conc (PaCO2) and therefore inversely related to alveolar ventilation |
|
|
What info can you get from capnography?
|
Detects hypoventilation and apnoea. Can also detect rebreathing (FiCO2 will increase), disconnections, resp and cardiac arrest. Can give rapid indication of falling cardiac output and adequacy of CPR. If EtCO2 < 10 mmHg compressions are not effective. Confirms correct ET tube placement. Use in conjunction with pulse oximetry |
|
|
What are the 3 main elements that effect EtCO2?
|
2. Cardiac output (will affect delivery of CO2 produced in tissues to lungs) 3. Ventillation (VA) |
|
|
What does a normal capnogram look like?
|
|

