![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back
|
Dilation of the bile duct is found without evidence of an obstructing lesion
|
Biliary Cyst should be suspected
The finding of fusiform dilatation of the common bile duct in the absence of obstruction or stones is characteristic of a type I biliary cyst. Intermittent chronic pain and episodic jaundice are the most common symptoms. Though biliary cysts are rare (1:10,000 to 1:15,000 births in the United States), recognition is important because a biliary cyst confers a risk for recurrent bouts of cholangitis and a high risk for biliary cancer (up to 75%) -- therefore, the cysts should be resected. Extrahepatic dilatation of the common bile duct is the most common type of biliary cyst and is seen in 50% to 80% of cases. |
|
|
Biliary Cysts
|
The diagnosis of a biliary cyst should be considered when dilatation of the bile duct is found without evidence of an obstructing lesion. Symptoms of biliary cysts include chronic, intermittent abdominal pain and recurrent bouts of cholangitis or jaundice. When abdominal ultrasound or CT suggests a biliary cyst, MR cholangiography, endoscopic cholangiography, or endoscopic ultrasound can be used to define cystic dilatation of the bile ducts and the absence of obstruction. There is a 20-fold increased risk of cholangiocarcinoma in patients with biliary cysts. Therefore, surgical excision of the entire cyst with formation of a hepaticojejunostomy is indicated. Operative resection of biliary cysts not only reduces risks of malignancy but can also alleviate development of further bouts of cholangitis.
|
|
|
Most common cause of SVC syndrome
|
Lung cancer (2/3), but also lymphoblastic and diffuse large B-cell lymphoma, Hodgkin Lymphoma, and germ cell tumors
Approximately 60% of patients present with SVC syndrome as the initial manifestation of a previously undiagnosed malignancy. The most common radiographic findings include mediastinal widening and pleural effusion; however, 16% of patients have a normal chest radiograph. Mediastinoscopy is routinely used to obtain tissue biopsy samples for histologic diagnosis. The complication rate from this procedure is only 5% in patients with SVC syndrome. Percutaneous transthoracic CT-guided needle biopsy appears to be a safe alternative to mediastinoscopy and has a sensitivity of 75%. The goal of treatment, which can usually be delayed while a tissue diagnosis is obtained, is to reduce symptoms and treat the underlying malignancy. Primary therapy for the underlying disorder using chemotherapy, radiation therapy, or combined chemotherapy and radiation therapy is usually associated with rapid and complete resolution of symptoms and physical findings of SVC syndrome. Improvement generally occurs within 2 weeks after therapy is begun. When only partial patency is reestablished, anticoagulation is appropriate in some patients. Endovascular stenting, angioplasty, surgery, and thrombolytic therapy have only a limited role when primary treatment is ineffective. |
|
|
What percentage of all nail dystrophies are caused by conditions other than fungi?
|
50%
Because up to 50% of all nail dystrophies are caused by conditions other than fungal infection, the diagnosis of onychomycosis should be confirmed before treatment is initiated. Nail infections can be diagnosed with potassium hydroxide (KOH) examination or culture; however, periodic acid-Schiff staining of a clipping of the nail has proved more sensitive (85%) than either of the former tests. The test is simple to perform and gives results in a few days. |
|
|
If all 20 nails are affected or all 10 toenails or all 10 fingernails are affected, what is the most likely cause of the nail dystrophy?
|
Noninfectious - such as psoriasis or lichen planus
|
|
|
When is treatment for onychomycosis indicated?
|
Treatment is usually indicated if the onychomycosis is symptomatic (painful) or if there are comorbidities (diabetes mellitus). Before oral treatment is instituted, it is important to confirm the diagnosis by potassium hydroxide (KOH) examination of the nail, a fungal culture, or by histologic examination of the nail clippings. Oral antifungal therapy is the most effective approach when treatment is indicated; topical antifungal agents have limited efficacy and are not recommended.
Oral terbinafine is first-line therapy for toenail involvement (250 mg/d for 12 weeks) and for fingernail involvement (250 mg/d for 6 weeks). Liver chemistry tests should be performed prior to initiation of therapy because rare cases of liver failure have occurred with the use of terbinafine for the treatment of onychomycosis. Drug monitoring for neutropenia, leukopenia, and liver toxicity should be done for those on therapy more than 6 weeks. |
|
|
When should autuimmune blistering disease be considered as apart of the ddx?
|
When a patient presents with unexplained blistering or erosion of the skin
|
|
|
Patients with celiac disease are at increased risk for what cancer?
|
Gastric Lymphoma
|
|
Immunofluorescence stain demonstrates granular deposition of IgA in the papillary dermis in a patient with rash on his torso and diarrhea
|
Dermatitis herpetiformis
|
|
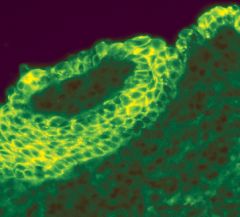
Immunofluorescence shows intrecellular IgG deposition in a patient with bullous skin lesions, characterstic of what disease?
|
Pemphigus Vulgaris
|
|
|
What is the threshold to treat for adrenal insufficiency in patients who are critically ill with hypoproteinemia (albumin <2.5) ?
|
random serum cortisol level greater than 12 micrograms/dL (331 nmol/L) in a critically ill patient with hypoproteinemia (albumin level <2.5 g/dL [25 g/L]) makes the diagnosis of adrenal insufficiency unlikely and treatment with hydrocortisone unnecessary.
|
|
|
Hepatic venous outflow tract obstruction
|
Budd-Chiari syndrome is diagnosed by the finding of hepatic venous outflow tract obstruction on cross-sectional imaging; ultrasonography is recommended as the diagnostic test of choice based on its widespread availability. RHF and constrictive pericarditis must be ruled out.
Patients with PV or other causes of polycythemia are at increased risk. Initial treatment of BCS includes anticoagulation therapy for all patients regardless of whether an underlying prothrombotic disorder is discovered. |
|
|
Risk factors for Budd Chiari syndrome?
|
An underlying risk factor for thrombosis is found in up to 80% of patients with BCS, with myeloproliferative diseases accounting for about 50% of cases. Other causes include Behçet syndrome, antiphospholipid antibody syndrome, and oral contraceptive use.
|
|
|
Most successful long-term and safest weight loss strategy in obese and overweight patients.
|
Consistent reduction in daily dietary caloric intake is the most successful long-term and safest weight loss strategy in obese and overweight patients.
|
|
|
Options for reducing blood pressure in the setting of stroke if BP >180/>105
|
Labetalol or Nicardipine
|
|
|
Why should you avoid using nitroprusside in patients with acute ischemic stroke or hemorrhage?
|
Nitroprusside is relatively contraindicated in patients with acute ischemic stroke or hemorrhage because of the possibility of increasing intracranial pressure.
|

