![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
Diagnosis assisted by CXR with widened mediastinum, bloody pleural tap and cultures of blood, pleural fluid or CSF for GPRs
|
Anthrax
Bacillus anthracis |
|
|
GASTROINTESTINAL ANTHRAX
Presents in which 2 ways? |
Oropharnyngeal Anthrax (hard palate, post pharynx)
Cervical edema, necrosis Often fatal, death from bacteremic spread Abdominal Anthrax (large bowel, cecal lesions) Fever, nausea and vomiting 2-5 days stools become bloody, tissue invasion leads to bacteremic spread and death |
|
|
Diagnosis of Anthrax
|
Be able to recognize clinical syndromes
High clinical suspicion in right setting is crucial to diagnosis/therapy due to high mortality Cultures + GPR (skin/vesicles, sputum, pleura, CSF, blood) Toxin assays (ELISA) |
|
|
Bacillus cereus
causes what diseases in which people? |
FOOD POISONING
TRAUMATIC OCULAR INFECTIONS Normal flora, potential culture contaminant Contaminant of drug paraphernalia/heroin Immunocompromised (HIV, corticosteroids, Sickle Cell Disease) host or IVDU, risk of serious infection (bacteremia, meningitis) Immunocompetent hosts, usually contaminant (wounds, cultures) but can see associated |
|
|
Bacillus cereus
Extracellular products contribute to the manifestations of clinical disease: |

Enzymes (collagenase, hemolysin, protease, phospholipase) contribute to tissue destruction
Toxins (enterotoxins) lead to diarrhea/emesis Antimicrobial agents produced by bacteria (examples: polymyxin, bacitracin) help bacteria to compete |
|
|
Two types of Food Poisoning from B. Cereus:
|
EMETIC form (vomiting predominate feature)
Incubation <6 H Similar to S. aureus food poisoning FRIED RICE DIARRHEAL form (cramps, nausea, watery stools) Incubation 10-12 H, improved in 24 H Similar to C. perfringens food poisoning Contaminated meats (turkey) or vegetables |
|
|
Where will you find the toxin of B. Cereus?
|

Due to enterotoxin production
Culture the food! Self-limited, no antibiotic therapy needed. Prevention – avoid cooling foods at RT (keep <10°C) and must be properly reheated to destroy spores (>60°C) |
|
|
Bacilus Ocular Infections
|
B. cereus predominates, other Bacillus sp.
Trauma (soil exposure) or foreign body (particles of dust, soil or metal shrapnel) Intravenous drug abuse (IVDA) Manifests: panophthalmitis, ocular abscess Extracellular enzymes destroy eye tissues Rapid 12-48 H (pain, redness, visual ) Early diagnosis, surgical therapy and antibiotics (IV, intra-vitreal); IV Clindamycin, Vancomycin |
|
|
Aerobic, club shaped, “diptheroids”
|
C. diptheriae – cause of diptheria
C. jeikeium (Group JK) – cause of bacteremia in immunocompromised patients /neutropenia, hospital acquired infections (IV catheters) Resistant to antibiotics, sens. VANCOMYCIN |
|
|
C. diptheriae
|

Non spore forming GPR
Club shaped on gram stain EXOTOXIN Virulence factor Inhibits protein synthesis Extremely potent Responsible for tonsilar/pharyngeal exudate production of DIPTHERIA Antibodies to toxin are protective |
|
|
DIPTHERIA
Epidemiology |
Humans are reservoir
Asymptomatic carrier state (< 5%) on skin and in pharynx Immunization reduces carrier state Infected patient/carrier contacts susceptible host Transmission through bacteria in airborne droplets or contact with secretions/exudate COLDER months, temperate climates, crowded conditions |
|
|
Diptheria: Those at risk today
|
Those at risk today:
Children < 15 yo if unvaccinated Unimmunized or unboosted adolescents/adults (urban poor, those with no access to health care, IVDU) |
|
|
Diptheria
Clinical Manifestations |

Respiratory tract (local disease) incubates 2-3d
Toxin produces inflammation, dense necrotic exudate in pharynx/trachea necrotic collection of cells, fibrin, dead respiratory epithelial cells, RBCs, WBCs and bacteria removal promotes bleeding of submucosa Exudate is tough and leathery, grey Extends and can occlude airway obstruction Soft tissues of the neck can swell, “bull neck” Death can be caused by aspiration of the membrane Fever, sore throat and membrane development (tonsils, posterior pharynx) Cervical lymph nodes common Once toxin is absorbed, can see systemic effects on tissues at distant sites (risk increases with severity of disease) CARDIAC TOXICITY (MYOCARDITIS) 1-2 wks after illness; up to 10-15% infected Lead to arrhythmia, heart block, heart failure if progresses NEUROLOGIC TOXICITY Up to several months later Cranial neuropathies to wide range of presentations |
|
|
Diptheria
Clinical Manifestations |
Fever, sore throat and membrane development (tonsils, posterior pharynx)
Cervical lymph nodes common Once toxin is absorbed, can see systemic effects on tissues at distant sites (risk increases with severity of disease) CARDIAC TOXICITY (MYOCARDITIS) 1-2 wks after illness; up to 10-15% infected Lead to arrhythmia, heart block, heart failure if progresses NEUROLOGIC TOXICITY Up to several months later Cranial neuropathies to wide range of presentations |
|
|
Diagnose Diptheria
|

Use clinical clues to prompt early therapy
Tonsillitis/pharyngitis with associated membrane with febrile/toxic appearance Cervical adenopathy, cervical swelling (“bull neck”) Paralysis of palate, hoarseness or stridor |
|
|
Listeria monocytogenes
|

Small gram positive rod
Cocci, diplococci 25°C TUMBLING MOTILITY Intracellular pathogenesis Rare cause of disease but risk to select population Risk for food borne disease |
|
|
Listeria monocytogenes
Epidemiology |
Zoonosis, ubiquitous in nature (soil, decaying vegetable matter, feces)
Vertical transmission, no other human-human Up to 70% raw vegetables; raw milk, fish, meats (including processed meats), poultry FOODS: coleslaw, unpasturized soft cheeses, ready-to-eat products/meats, smoked fish |
|
|
Those at Risk for Listeria:
|
Neonates and elderly (extremes of age)
Pregnant women Impaired cell mediated immunity, immunosuppression (steroids, transplant recipients) HIV + (100 x more likely than HIV-), low incidence due to prophylactic antibiotics |
|
|
Incubation for Listeria Food Poisoning
|
Incubation ranges 11-70 days
Infection most likely begins with contaminated food ingestion (possible maternal-fetal) Gastric surgery or H2 blockers promote infection (stomach pH increased) |
|
|
Binds epithelial cells, able to escape INTRACELLULAR killing
Survives intracellularly Filopods (bacteria push against membrane) to allow passage to adjacent cells, avoiding exposure to immune system and escaping immunosurveillance |

Pathogenesis of Listeria?
|
|
|
Clinical Manifestations of Listeria
|
Meningitits
Bacteremia Gastroenteritis Neonatal infection Listeriosis during pregnancy |
|
|
Listeria: Neonatal infection
|
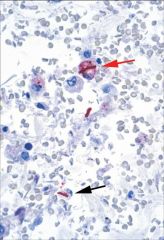
Infection in-utero (placenta) GRANULOMATOSIS INFANTISEPTICA – immediate spontaneous abortion/neonatal death
Infection at parturition - meningitis 2wk post-birth or immediate sepsis after delivery |

