![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
|
3 types of capillaries
|
Continous capillaries
Fenestrated capillaries Discontinous Capillaries |
|
|
Organ location continuous capillaries
|
(skeletal muscle, cardiac muscle, skin, lung, fat, CT, BBB)
|
|
|
Organ location fenestrated capillaries
|
((sinusoids)glomerulus, exocrine gland, intestinal mucosa, ciliary body, choroid plexus, synovial lining joints & endocrine glands)
|
|
|
Organ location discontinous capillaries
|
(“sinusoids” in liver, bone marrow, spleen)
|
|
|
Description Continous capillaries
|
Circumference = 1-3 endothelial cells(very active cells, NO production) + basement membrane. Endothelial cells connected w/ tight jxs. Limiting exchange, BUT lipid insoluble transfers this way.
|
|
|
Description fenestrated capillaries
|
Have endothelial cells like continous subtype BUT has fenestra (perforated windows) w/ thin (5nm) diaphragms. Fenestra ↑ exchange 10X
|
|
|
Description discontinous capillaries
|
inter-endothelial gaps (100nm wide) (compare to fenestra 5nm). Additionally, basement membrane discontinous. Allows large particles to move into blood/tissue.
|
|
|
Transcapillary Fluid Filtration & Reabsorption Formula
|
J_f= L_p*S [(P_C-P_T )- σ (π_C-π_T )]
Jf = transcapillary fluid flux Lp = HYDRAULIC CONDUCTIVITY (FLUID PERMEABILITY) S = capillary surface area PC = capillary hydrostatic pressure PT = tissue hydrostatic pressure π_c = capillary colloid pressure π_t = tissue colloid pressure σ = plasma protein reflection coef.(accounts permeabilty specific protein) |
|
|
General trend transcapillary flux
|
So fluid flux is dependent on Hydrostatic pressure gradient and the oncotic pressure gradient. Lp desscribes how the fluid viscosity would affect the flow.
|
|
|
Define edema
|
Edema – accumulation of fluid in interstitial space. Results when net filtration > lymph drainage rate.
|
|
|
3 examples of how changes in starling forces causes edema
|
1.Arteriolar vasodilation ↑Pc increasse in capillary hydrostatic pressure = ↑flux
2.Liver failure ↓π_C decrease protein production causing decrease oncontic pressure 3. Burns/Inflammation ↑LP Δ in capillary integrity = ↑ conductivty & ↑ net flux |
|
|
4 functions of lymphatic system
|
1. Return of Excess filtered fluid – 7200L pumped per day. Net flow from vessel results in 3L/day . Lymphatic system returns this to venous circulation.
2. Defense against disease – lymph travels through lymph nodes. Lymph nodes have resident phagocytic cells that kill bacteria. Additionally, mature B & T lymphocytes reside here and mediate anti-body & cell meddiated immune responses. 3. Transport of absorbed fat – Packaged particlesto large cross GI cappilaries. BUT they can enter GI lymph for transport. 4. Return of filtered protein – If abnormal amts. protein pass through capillary then fluid will follow (oncotic pressure). This would be dangerous and thus excess protein is returned to venous system. |
|
|
define lymphadema
|
Compromised normal lymphatic function. Causing ↑ interstitial fluid accumulation = swelling. Occasionally the mmune system will become involved in theis pathology.
|
|
|
4 factors augment venous return
|
1. Sympathetically-induced venous contraction – scattered smooth muscle in venous system is highly innervated by sympathetic system. Constrict = ↑pressure = ↑gradient (→ venules constriction> vein)
2. Skeletal muscle pump – squeezing vessels + unidirectional valves = ↑ venous return. i.e. Calf Muscle Pump & sitting airplane too long. 3. Respiratory activity – Inspiration = ↓chest cavity pressure (below atmosph.) = distension vena cava = ↑ venous return w/ inspiration 4. Cardiac Suction Effect – W/ each atria relaxation pressure ↓ causing suction = increase gradient & venous return. |
|
|
Virchow's Triad
|
Virchows triad are risk factors for DVT. Frequently DVT develop behind valves. (a FOUNDATIONS TOPIC). Predispoistion to DVT occurs when 2/3 risk factors are present.
1. Blood stasis 2. Blood vessel injury 3. Hypercoaguable state |
|
|
definition central venous pressure
|
Central Venous Pressure – BP venous system near RA (measured if catheter = thoracic vena cava near RA)
|
|
|
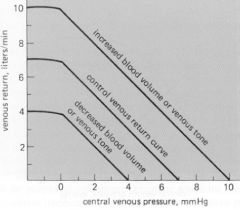
Factors that shift Venous return curve (verbal)
|
1. Venous blood volume (↑ vol = ↑venous return) & (↓ vol = ↓ venous return)
2. Venous tone (↑vasoconstriction = ↑venous return) |
|
|
Venous Return Curve Shift
|
|

