![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
94 Cards in this Set
- Front
- Back
|
Aerobic |
must have oxygen to grow |
|
|
anerobic |
cannot grow in the presence of oxygen, usually C02 |
|
|
facultative anaerobe |
can grow in either environment, with or with oxygen but usually grows best in the presence of oxygen |
|
|
Thioglycolate broth |
all purpose media for most all bacterial organisms. -contains sulfhydryl groups which bind free oxygen rendering it inert and creating an anaerobic environment. |
|
|
capnophile |
organism that grows in high concentrations of C02 |
|
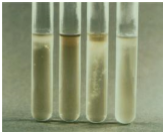
Thioglycolate broth |
• Gas exchange occurs in top 1/3 of tube allowing aerobes to grow. • Anaerobes grow in bottom 2/3 of tube • Facultative organisms grow throughout • Resazurin is added as an indicator . Pink in presence of oxygen, colorless w/o oxygen |
|
|
sterilization |
destroys all forms of life including spores |
|
|
4 types of sterilization |
1. heat 2. filtration 3. chemical 4. ionizing radiation or/and UV light |
|
|
4 types Heat Sterilization |
1. moist heat - autoclaving (heat and pressure)
2. boiling (100C for 10 min, not sterile) 3. incineration (ie open flame to a loop) 4. dry heat (160C for 2 hours - used for glassware) |
|
|
autoclaving |
heat under pressure, 15psi for 15 min @ 121C |
|
|
Filtration |
used in sterilization of heat sensitive solutions -vaccines/antibiotic solutions - pushed by a pressure of vacuum -used for liquid or air -HEPA filters in our everyday lives |
|
|
chemical |
used for solid and heat labile materials -ethylene oxide most common used for sterilization (surgical and other hospital equipment) - most chemical agents used mostly as disinfectants (alcohols and aldehydes -toxic to humans but kills spores) |
|
|
non-ionizing UV and Ionizing radiation |
-poor penetration to disinfect surfaces -causes direct damage to DNA of organisms -UV light is used in biohoood but only over night (long exposure) -radiation is short wavelengths used to sterile disposable syringes/gloves |
|
|
viewing organisms: living state |
less organism distortion -determine motilitiy -some organisms do not stain easily and should be observed live |
|
|
viewing organisms: fixed state |
allows for different staining techniques - gram stain |
|
|
Bright field microscopy |
most common in clinical laboratory -background is light, organism is dark -cells are stained |
|
|
5 different types of stains |
1. gram stain 2. acid-fast stain 3. capsular stain* 4. flagellar stain* 5. spore stain * *not used in this lab |
|
|
Gram stain process |
Primary stain - Crystal Violet 30s Mordant - iodine 30s Decolorizer - alcohol 5s Counter stain - safranin - 30s |
|
|
Gram stain reading |
+ purple (thick cell walls) - pink (thin cell walls) |
|
|
Gram stain principle |
bacteria with thick cell walls containing teichoic acid (retains the crystal violet) retain the crystal violet-iodine complex, identifying them as gram positive. - other bacteria with thinner cell walls containing lipoplysaccarides do not retain the dye, so the alcohol/decolorizer is necessary to damage the thin lipid layer for the counter stain to complex to bind. |
|
|
Acid Fast stain |
red rods and bright blue background |
|
|
capsular stain |
exhibit a zone of clearing with colored backgrounds. -halo of external polysaccharides |
|
|
flagellar types |
1. polar (at one end) 2. bipolar ( at both ends) 3. peritrichous (surrounds the bacteria, looks like a hot mess) |
|
|
spore |
spores present in 2 types 1. terminal (at one end) 2. sub terminal or central (middle) |
|
|
Fluorescent Microscopy |
UV light is used to visualize chemically treated organisms. - Fluorochrome - immunofluoresence (PCP) |
|
|
Dark Field Microscopy |
uses indirect light - organism is bright on a dark background. - useful for motility and organisms that will not stain with routine stains |
|
|
electron microscopy |
can be used to identify viral particles not common in most labs uses electron beam |
|
|
2 techniques for obtaining a pure culture |
1. pour plate (common in food and dairy micro - colonies are inside the agar) 2. streak plate method (most common in a clinical lab - allows for quantitative growth) |
|
|
streak plate |
a calibrated loop (disposable) is used to place the specimen onto the media by inoculating right down the plate. - cross streaks are started at the top and move down the plate - colonies can be counted after incubation. |
|
|
streak plate technique |
everything other than urine is streaked into 3rd and 4th quadrants for isolation. -isolated colonies are used for susceptibility tests |
|
|
Primary media = non-selective media |
-sheep blood agar --used to grow most organisms of clinical interest -chocolate agar --heated sheep blood with added nutrients to grow more fastidious organsims -tryptic soy agar |
|
|
differential media |
Have biochemical compositions that cause certain bacteria to take on a distinct appearance -macconkey agar - lactose fermentation -Mannitol Salt Agar MSA differential for Mannitol fermentation. |
|
|
selective media |
Has chemical components that select for the growth of some organisms and prevent the growth of others • Campy-blood agar – Contains nutrients and antibiotics that allow for the growth of Campylobacter species while inhibiting other organisms • Hektoen enteric agar – Selective for GNR’s – Also differential for lactose fermentation and Hydrogen sulfide (H2S) production |
|
|
Enrichment media |
-Inhibit most normal flora Increases the number of a desired organism while inhibiting undesired organisms • Usually a broth based media .• Example: LIM broth for Group B Strep – Most specimens are rectal/vaginal swabs with lots of normal flora – LIM inhibits most all organisms except “Strep B” – Lim is inoculated and incubated overnight and then subbed to a BAP. – BAP is incubated and then examined for typical Group B Strep colonies |
|
|
Collection |
– Collect prior to administration of antibiotics – Collect where organism is most likely to be found - collect appropriate amount of specimen -sterile containers -prompt delivery (30 min to 2 hours) - do not refrigerate CSF -examine motile specimens immediately - flagella breaks off after 30 min and it looks like a white cell |
|
|
Urine |
#1 clinical specimen micro sees - needs to be in the lab within 2 hours of collection. - if refrigerated good up to 48 hours - preservative cup, good up to 72 |
|
|
UTI |
if it is greater than 100,000 CFU per mL then it is a true UTI, for females of child bearing age, anything over 10,000 is based on clinical presentation |
|
|
surgical specimens |
ALWAYS PROCESSED STAT |
|
|
Gram positive cocci |
1. micrococcus (pairs or clusters) 2. staphylococcus (grapes or bunches) |
|
|
Micrococcus |
-usually in a tetrad formation and typically confused with S. aureus, only they are much bigger than staph. -occasionally cause infections (usually in immunocompromised patients) -not typically pathogenic -found in normal flora (skin and mucous) |
|
|
ways to distinguish Micrococcus from S. aureus |
1. Staph produce acid from glucose anaerobically 2.Staph are susceptible to lysis by lysostaphin 3.Staph produce acid from glycerol in the presence of erythromycin 4.Micrococcus produce a bright yellow pigmented colony Neon Yellow 5.Micrococcus are modified oxidase positive |
|
|
Staphylococcus |
• Gram positive cocci • Occur in pairs and clusters • Catalase positive – Used to distinguish species of strep • Reduce nitrates to nitrites • Can grow in high salt concentrations (7.8% and above) • Non-motile and non-spore forming • Most are facultative anaerobes • 3 main species – Staphylococcus aureus – Staphylococcus epidermidis – Staphylococcus saprophyticus |
|
|
S. aureus |
#1 pathogen of human interest -found in normal flora -usually beta hemolytic (complete lysis of RBC) -MSA (Ferments Mannitol Salt Agar- changes from pink to yellow) |
|
|
S. aureus characteristics |
1. definitive bound coagulase production 2. produces heat stable nuclease 3. smells like a dirty sock |
|
|
S. aureus pathogenicity |
1. entertoxins 2. exfoliative toxin 3. cytolytic toxins 4. cellular componets |
|
|
serological agglutination test |
-uses latex particles coated with IgG and fibrinogin, tests for clumping factor (bound coagulase) and Protein A (binds to Fc on IgG - found in S. aureus cell wall) takes 20 seconds but is super expensive |
|
|
S. aureus enterotoxins |
- entertoxins A and D cause diarrhea and vomiting - indicative of food poisioning **symptoms present 30 min to 2-4 hours after ingestion** --tsst-1 exotoxin that causes toxic shock syndrome - symptoms include; high fever, vomiting, diarrhea and severe shock. (super antigen reacts with many t-cells and heat stable up to 30 min at 100C) |
|
|
S. aureus exfoliative toxin |
-epidermolytic toxin -causes epidermal layer of skin to slough off by splitting the intracellular junctions of the skin - aka scalded skin or Ritter's disease -typically effects children under the age of 5 years old with spontaneous recovery - adults infected have a 50% mortality rate |
|
|
S. aureus cytolytic toxins |
-hemolysins and leukocidins (alpha) cause the hemolysis of RBC's bur also destroy platelets and tissue damage. -beta toxin hemolyizes RBC 37C and 4C hemolysis is enhanced - gamma toxin less toxic than alpha or beta |
|
|
S. aureus diseases |
1. septicemia 2. endocarditis 3. Pneumonia 4. osteomylitis 5. abcess of organs and muscle 6. UTI 7. common skin infections - boils - wound infections - cellulitus - impetigo |
|
|
S. aureus antibiotics |
> 90% resistant to Penicillin 40 - 55% are now resistant to Methicillin, nafcillin or oxacillin. Vancomyosin is the second best option |
|
|
coagulase negative Staphylococcus |
-95% are S. epidermidis -normal skin flora -most common contaminant of blood cultures |
|
|
S. epidermitis pathogenicity |
- opportunistic pathogen -endocarditis - SBE (subacute bacterial endo) -seen in IV drug users, immunocompromised patients, and patients with defective heart valves and indwelling medical devices (biofilms) - treat with vancomycin |
|
|
Biofilms |
gel like slime that moves with elasticity, can vary anywhere from an acute to a chronic infection (they like selective pressures). - colonization is started with surface proteins - once organisms start a biofilm they change genetic expression to lose their flagella and produce and adhesion mechanism. - biofilms do not break easily (elasticity) - phagocytoic cells cannot penetrate the biofilm, if they try they it can damage tissues) - penicillin cannot attack because the bioflim organisms slow down their metabolism and penicillin has no method of attack. |
|
|
S. epidermitis |
- coagulase negative - does not ferment mannitol (MSA) - not usually beta hemolytic - most common cause of nosocomal UTI |
|
|
Gram positive Cocci with negative or weak catalase reaction |
1. streptococci 2. enterococci 3. Leuconostoc and Pediococcus 4. Gemella and Stomatococcus 5. Aerococcus |
|
|
Streptococcus characteristics |
- gram positive cocci (occurs in pairs or chains) - all produce latic acid when fermenting sugars (not inulin) -non-soluble in bile salt - do not reduce nitrites to nitrates - catalase negative - facultative anerobes - some are capnophiles - |
|
|
Staph vs Strep |
to distinguish these two organisms you would use: - Gram stain Staph bunches - Strep chains - catalase Staph positive - Strep Negative - Nitrate Staph reduces - Strep does not reduce |
|
|
2 different classifications for Strep |
1. Browns - hemalytic properties -- Beta - complete hemolysis of RBC - zone of clearing -- alpha - incomplete hemolysis - greening of the agar -- gamma - no hemolysis 2. Lancefield groups -- antigenic properties of polysaccharide "C" substance on the cell wall surface. ABCDFG are clinically significant and are beta hemolytic except D which is alpha. |
|
|
strep test |
rips antigen off of cell and puts it into solution to identify strep |
|
|
Group A Streptococcus (GAS): Streptococcus pyogenes |
- beta hemolytic --- 2 types of hemolysis O and S --> O causes hemolysis in anerobic conditions --> S causes hemolysis in aerobic -stab agar method is used: hemolysis throughout = S hemolysis at the bottom = O |
|
|
GAS Pathogensis |
Produces hemolysins, toxins, and enzymes: Infections: pharyngitis --symptoms: sore throat, malaise (feeling sick), fever and headache - traditional strep (testing for group A - rapid strep test) - spread by droplet transmission and direct contact. pyodermal: impetigo, cellulitis, wound infections, and gangrene. |
|
|
GAS Necrotizing faciitis |
- flesh eating bacteria (strep pyrogene) - GAS gets between the skin and muscle and spreads rapidly. - difficult to treat - usually results in amputation - high mortality rate |
|
|
GAS: Erythrogenic toxins |
- effects red blood cells - Scarlet Fever --> associated with strep throat --> red, spreading rash 1-2 days after infection - like Toxic shock syndrome --> usually with a severe initial infection |
|
|
GAS: poststreptococcal infections |
1. Rheumatic fever --> complication of GAS pharyngitis --> fever and inflammation of the heart and joints and blood vessels and subcutaneous tissues 2. acute glomerulonephritis --> after cutaneous or pharyngeal infection - antigen antibody complex deposit in glomerulus causing damage - resulting in impairment of kidney function. --> rapid death in a few days |
|
|
GAS: Morphology |
- small white pinpoint colonies with a large zone of beta hemolysis - susceptible to bactracin (0.04 units) "A" disc -PYR positive |
|
|
Group B: Streptococcus agalactia infections |
Newborns -Pneumonia -septiciemia - meningitis -organmisms transmitted from the mother Adults -endometritis - wounds - endocarditis - osteomyelitis - upper respiratory infection - UTI's specimens taken from vaginal area or rectum |
|
|
Group B: Streptococcus agalactia screening |
• All pregnant women should be screened at 35-37 weeks gestation • Collect vaginal and/or rectal swabs • Place in enrichment broth (LIM) and incubate overnight • Sub broth to sheep blood agar and incubate overnight • Examine for Group B Strep colonies *screen twice if negative |
|
|
Group B: Streptococcus agalactia morphology |
- colonies present grayish white and mucoid, surrounded by a small zone of beta hemolysis (very discrete, typically right under the colony and not expanded past) - lancefield group B antigen - Hippurate hydrolysis Positive ( hippuric acid is hydrolyzed to benxoic acid and glycineby enzymatic action of hippuricase) - CAMP TEST positive (test for beta hemolytic group b organisms) |
|
|
Group C and G beta Streptococci |
-May cause pharyngitis - septicemia - endocarditis - meningitis - skin infections - there are some reports of post infectious complications such as glomerulonephritis and rhuematic fever - diagnosis is by Lancefield antigen typing -strep equi = group C strep canis = group G |
|
|
Group F and Microaerophilic Streps |
- Group F streps are Beta hemolytic and typically have very small colony sizes. - Microaerophilic strpes have very small colony size, alpha hemolytic and typically smell like butter. - both groups of organisms can cause bacteremia |
|
|
Streptococcus pneumoniae Identification |
- lancet shapped diplococci - usually encapsulated - typically small, shiny flattened colony with distinct zone of alpha hemolysis. often appears sunken in the center - nail head colony- caused by auto lysing characteristic. |
|
|
Strep pneumo diseases |
pneumonia -usually community aquired - septicemia -conjunctiva - otitis media - meningitis -endocarditis ear and eye |
|
|
strep pneumo identification |
- optochin susceptibility (p-disc) - bile salt soluable (bile enhances auto lysing) - ferments inulin - Neufeld-Quellung reaction - test for capsular antigens |
|
|
Strep pneumo treatment |
- penicillin - cephalosporins - vancomycin -east TN has developed the highest rate of resistance in the country over the last several years - susceptibility test - screening test 1 microgram disc and a zone greater than 20mm is considered to be susceptible. less than 20mm needs more testing |
|
|
Viridans streptococci |
- includes all alpha hemolytic strep that lack Lancefield group antigens and are not Strep. pneumoniae - includes small colony variants of beta hemolytic streps in groups A, C, F, G (usually S. anginosus has a butterscotch odor) - nonhemolytic species are also classified as viridans streptococci -->S. mitis group, S. mutans group, S. salivarius group, S. bovis group, S. anginosus group. - part of the normal upper respiratory flora, female genital tract and GI tract |
|
|
Viridans streptococci |
- drug of choice tetracycline when resistant to penicillin - oportunistic pathoghen, low virulence - may cause SBE (subacute bacterial infection), meningitis, abscesses (S. anginosus group), dental caries and osteomyelitis - often found in brachial brushings |
|
|
Group D Streptococci: Strep bovis and strep. equinus |
- alpha hemolytic, hydrolize bile-esculin and do not grow in 6.5% NaCl, PYR negative. - produce endocarditis, UTI's, abscesses in wounds and bacteremia. - a link has been made between Strep bovis and the presence of GI tumors |
|
|
Enterococcus |
• Includes Enterococcus faecalis and Enterococcus faecium • They are all α-hemolytic and possess the group D antigen • They hydrolyze bile esculin, are PYR positive and grow in 6.5% NaCl • All look similar – gray colonies with discrete α-hemolysis • They are normal flora in the intestinal tract. • Associated with UTI’s, wounds, and SBE • Drug of choice is ampicillin if susceptible. Vancomycin may also be used although some resistance is now seen. |
|
|
Organisms that resemble Streptococcus |
• Aerococcus – Appear similar to viridans strep on blood agar – Rarely encountered in the clinical lab. • Leuconostoc and Pediococcus – Appear similar to viridans strep on blood agar – Rarely encountered in the clinical lab. – Resistant to Vancomycin • Gemella and Stomatococcus – Appear similar to viridans strep on blood agar – Rarely encountered in the clinical lab. • All may cause endocarditis except Pediococcus |
|
|
Gram Negative cocci: general characteristics |
- Neisseria and Moraxella catarrhalis -GNC usually diplococci - catalase positive - oxidase positive - most grow on sheeps blood and chocolate agar - coffee bean shape - ID by CTA sugar fermentation patternsn (yellow is positive) - DO NOT grow on MacConkey |
|
|
Neisseria Meningitidis |
- ferments glucose and Maltose - can be normal flora of upper respiratory tract of carriers - causes endemic and epidemic meningitis and meningococcemia (gotten into the blood stream) - school aged children - young adults bc they live in close quarters. - spread by respiratory droplets and contact |
|
|
Neisseria Meningitidis: symptoms |
• Meningitis – Characterized by abrupt onset of frontal headache, stiff neck, and fever • Meningococcemia may occur with or without meningitis – Petechial skin lesions may develop – DIC and septic shock – Waterhouse-Friedrickson syndrome may occur (bleeding in the adrenal glands) • Death may occur 12 to 48 hours from onset. |
|
|
Neisseria Meningitidis: characteristics |
- super sensitive to temperature extremes and dehydration. - refrigeration will kill this organism - Grows SBA (sheep blood agar) and Choc. agar - grows best in C02 - does not require it - CTA postitive for glucose and maltose --> Neg for sucrose and lactose |
|
|
Neisseria Meningitidis: treatment |
- Penicillin drug of choice - prophylaxis of people who had close contact --> ryphanthasin or sulfunamide - vaccines only used for managing epidemics - seria groups for vaccine -- polysaccaride A,C, Y, W-135 - seria group B is the most common meningitidis but it is poorly immunogenic . |
|
|
Neisseria gonorrhoeae |
- aka gonococcus or GC - humans only natural host - acute pyogenic infection of columinar and transitional epithelium. - never normal flora, always pathogen - can be found intracellular in PMN's - fastidious (hard to grow) |
|
|
Neisseria gonorrhoeae: symptoms |
- conjuctival - pharyngitus - transmitted by sexual contact - Asymptomatic carriers (typically women) -2-7 day incubation - discharge - gram stain discharge and diagnose from only discharge (only in MEN) and dysuria |
|
|
Neisseria gonorrhoeae |
Women - endocervix- vaginal discharge, lower abdominal pain and vaginal bleeding Disseminated infections -purulent arthritis -septicemia -fever and rash on extremities |
|
|
Neisseria gonorrhoeae: growth |
3 requirements for growth in culture - appropriate agar - enriched media, choc. Martin-Lewis or Thayer-Martin - temp 35-37C - 3-10% C02 |
|
|
Neisseria gonorrhoeae: presumptive ID |
• Isolated from selective media • Microscopic morphology – Gram negative kidney bean-shaped diplococci • Colonial Morphology – Small, gray, translucent, and raised after 24-48 hours • Oxidase test – Positive |
|
|
Neisseria gonorrhoeae: definitive ID |
• CTA Sugar fermentation pattern – glucose only • Monoclonal Fluorescent Antibody stain • Immunologic coagglutination – antibody coated latex particles • Chromogenic enzymes – RapID NH • ELISA’s • DNA probes |
|
|
Neisseria gonorrhoeae Treatment |
• Several single dose antimicrobials are available – Ceftriaxone – Spectinomycin – Ciprofloxacin • Penicillin may be used if βlactamase negative • Doxycycline or azithromycin should also be given because of the high percentage of people infected with GC are also infected with Chlamydia *if beta lactamase NEGATIVE large dose of penicillin - drug of choice * beta lacta POSTIVE has beta lactam inhibitor - ceftriaxone is drug of choice |
|
|
Moraxella catarrhalis |
Formerly known as Neisseria catarrhalis, then Branhamella catarrhalis • Normal commensal of the respiratory tract • Is an opportunistic pathogen (when in large numbers) associated with: – Pneumonia (sputum) – Sinusitis – Otitis media -not reported unless dominant |
|
|
Moraxella catarrhalis: Identification |
• Gram negative diplococci • Oxidase positive • Butyrate esterase positive • Asaccharolytic in carbohydrate tests • Growth on Sheep blood and Chocolate agar – smooth, opaque, gray to white colonies --> hockey puck type colony • Usually β-lactamase positive -CAT disc |

