![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
How do we prove causality of an infectious disease?
|
Koch's Postulate
1. To prove an organism causes a disease: a. Organism must be present in diseased tissue. b. Isolate the organism in pure culture from a sick host. c. Inject a naive host (or experimental animal) and induce the disease. d. Reisolate the organism in pure culture from the second host. 2. Corollary: A rise in serum antibodies or positive skin test responses to the infectious agent are traces left in the immune system of infection. |
|
|
Legionnaires' Disease
|
Caused by Legionella Pneumophilia
Clinical Manifestations Incubation period: 2-10 days Day 1 malaise, myalgia, headache Day 2 fever (97%), chills (74%), rigors (74%), nonproductive cough (86%), rales (80%), chest x ray positive with unilateral or bilateral patchy infiltrate, lobar pneumonia Days 3-5 death or recovery. 16% fatality rate (29/182). Epidemiology- No person to person transmission. Proof of a bacterial etiology: Organisms cultured on agar and isolated. Organisms from agar injected into guinea pigs cause disease. Organisms could be reisolated from sick or dead guinea pigs. Antiserum raised in rabbits to organism reacts with infected tissue. 62/136 seroconvert = 4 fold rise in antibody titer by the indirect fluorescent* antibody test. 39 patients had single titers > 1:128. Mode of Transmission: Aerosols from: showers, decorative fountains, humidifiers, respiratory therapy equipment, whirlpool spas, showers in automotive manufacturing plant, potting soil. Legionella live in water in nature and parasitize amoebae where they divide intracellularly leading to high concentrations of organisms Prevention: Cooling towers - chlorinate Point of use water supplies heat-water to >70oC (158oF) Also note that previous exposures can confer resistance and that about 80% of pt's that get it are imunocompromised sopradic cases (20% in outbreaks). Mechanism of disease: Invades macrophages by coiling phagocytosis and undergoes intracellular replication in ribosome studded vacuoles Secretion of extracellular enzymes, including a metalloprotease, a phosphatase, a lipase and DNase and RNase Classification: Of the Legionella species, L. Pneumophilia causes the most diseas, and of the 10 serogroups, #1 is responsible 90% of the time. Serogroups 1 and 6 can also cause nonfatal Pontiac Fever, as well as other legionella species (no pneumonia, ony recognized in outbreaks) Dx: Isolation on BCYE (buffered charcoal yeast extract) agar Legionella antigens in urine Visualization in smears by direct fluorescent antibody (DF: Add a fluorescein labeled antibody that is raised in rabbits or goats by injecting killed Legionella, so it is know to react with Legionella. This antiserum is a reagent to detect the bugs). 4. Greater than a 4X rise in serum antibody titer between acute and convalescent serum as determined by indirect fluorescence. |
|
|
T/F Finding Legionella pneumophila in lungs of patients who died proves it caused the disease.
|
False. Association does not prove causation. You need to rule out presence of the organism in normal people. Also it could be a secondary invader to an unknown primary causative agent.
|
|
|
T/F Presence of antibodies to an organism proves that it caused the infection from which patient is recovering.
|
False. Antibodies could have arisen from a previous encounter with this organism and persisted. Antibodies may be the result of a previous vaccination for organisms for which there are vaccines (not Legionella). A fourfold rise in antibodies between acute and convalescent sera is needed as evidence of causality.
|
|
|
Pathogenicity
|
ability of an infectious agent to cause disease
|
|
|
Virulence
|
relative degree of pathogenicity.
Virulence is defined as disease-causing potential relative to a specific, normal host. An immunocompromised host may be hypersusceptible. Virulence is measured in animal models by the LD50 = lethal dose needed to kill 50% of the animals. ID50 for viruses can be determined in vitro by the dose needed to infect and destroy 50% of a tissue culture cell monolayer. |
|
|
Opportunistic Pathogens
|
normally nonpathogenic or weakly pathogenic but can cause disease in immunocompromised hosts.
|
|
|
Attenuated Organisms
|
ones with reduced virulence, frequently developed as vaccine strains.
|
|
|
Types of Infections
|
Extracellular - pyogenic or suppurative (pus producing) including Staphylococci, Streptococci, Pneumococci, Hemophilus influenzae, Neisseria, Clostridium tetani, Clostridium botulinum, Clostridium perfringens, Corynebacterium diphtheriae, Bordetella pertussis
Intracellular: nonviral pathogens of macrophages include Mycobacterium tuberculosis, Mycobacterium leprae, Listeria monocytogenes, Toxoplasma gondii, Leishmania spp., Brucella abortus, Legionella pneumophila, Histoplasma capsulatum, Pathogens of any tissue cell - All of the viruses, Prions, Other organisms like rickettsia whivh grow on endothelil cells |
|
|
Extracellular Vs. Intracellular pathogens
|
Extracellular - Acute inflamatory response, presence of PMN's (pus), rapid progression, pathogenesis caused prominently by exotoxins, but also by capsules. The effective immunity is antibody mediated.
INtracellular - Chronic inflamatory response with the presence of macrophages and T Cells (mononulear), slow progression, pathogenesis. The effective immunity is cell mediated. |
|
|
Innate Host Defenses
|
a. Epithelial barriers: skin, mucosal linings
b. Mucous - gastrointestinal tract, gut, respiratory tract c. Ciliary epithelium - respiratory tract d. Low pH of the stomach (gastric acidity) e. Phagocytic cells (professional phagocytes) - PMNs and macrophages (PMNs are polymorphonuclear leukocytes) f. Mononuclear Phagocyte System (MPS) = old RES (Reticulo-Endothe¬lial System) visualized by carbon clearance g. Natural Killer Cells – lymphocyte subset 1) Direct lysis of virally infected cells and neoplastic cells 2) Produce interferon-gamma (IFN-γ) in response to IL-12, which activates macrophages h. Alternate and mannose binding pathways of complement 1) Generate C3a and C5a to amplify an inflammatory response, and deposit C3b on pathogens to enhance phagocytosis. |
|
|
Adaptive Host Defenses
|
a. Specific serum antibody- Activity amplified by classical pathway of complement
b. Secretory IgA at mucosal surfaces c. Cytotoxic T cells d. Th1 cells- IFN-γ leads to macrophage activation/cellular immunity |
|
|
Virulence Factors
|
Toxins:
Exotoxins are generally excreted proteins Endotoxins are part of the outer membrane of gran negatice organisns, composed of LPS. Penetration and spreading factors Adherence Factors Numbers parasitization and killing effector cells of host immune system Microbe initiated immunopathogenicity Hiding Protective coating antigenic variation deoys cleave/bind host antibodies masquerade as host antigen |
|
|
Botulism
|
Clostridium botulinum
Botulotoxin is anticholinergic. Prevents release of acetylcholine at the myoneural junction, re¬sulting in flaccid paralysis. |
|
|
Tetanus
|
Clostridium tetani
Tetanus toxin blocks inhibitory synapses by centrally inhibiting release of neurotransmitters, resulting in spastic paralysis. |
|
|
Gas Gangrene
|
Clostridium perfringens
α-Toxin is a phospholipase C or lecithinase, which is cytolytic, necrotizing, and hemolytic. Tissue destruction. |
|
|
Staphylococcal Food Poisoning
|
Staphylococcus aureus
Staphylococcal enterotoxins stimulate brain or peripheral nerves to produce vomiting (?) |
|
|
Staphylococcal Toxic Shock Syndrome
|
Staphylococcus aureus
Toxic shock syndrome toxin-1 causes fever and shock. |
|
|
Staphylococcal Scalded Skin Syndrome
|
Staphylococcus aureus
Exfoliative toxin causes loss of outer layer of epidermis |
|
|
Scarlet Fever
|
Streptococcus pyogenes (Group A)
Strains which secrete erythrogenic toxin possibly via cytotoxin to blood vessels. Phage coded. |
|
|
Diptheria
|
Corynebacterium Diptheriae
Diphtheria toxin inhibits protein synthesis by ADP ribosylating elongation factor 2 and inhibiting protein synthesis. Damage to internal organs results. Toxin is phage coded. |
|
|
Pseudomonas opportunistic infections
|
Pseudomonas aeruginosa
Exotoxin A - mode of action similar to diphtheria |
|
|
Whooping Cough
|
Bordetella pertussis
One strain produces three toxins: Pertussis toxin ADP ribosylates a GTP binding protein. Adenyl cyclase toxin - effects PMN function. Tracheal cytotoxin - toxic to ciliated tracheal epithelium. May be peptidoglycan. |
|
|
Cholera/E-Coli caused travelers diarrhea
|
Vibrio cholerae/ E. Coli
Cholera toxin and E. coli heat-labile toxin alter water and electrolyte balance in intestine by ADP ribosylating a GTP-binding protein which elevates adenyl cyclase with accumulation of cAMP in epithelial cells in gut. This causes the pumping out of elecrtolyes and water osmoses out in response. |
|
|
penetration and spreading factors
|
Hyaluronidases from Streptococci, Group A- Lysis of tissue group substance
Coagulase from Staphylococcus aureus- Clots fibrin Kinases from Staphylococci/Streptococci-Lysis of fibrin |
|
|
Virulence Factors
|
Toxins:
Exotoxins are generally excreted proteins Endotoxins are part of the outer membrane of gran negatice organisns, composed of LPS. Penetration and spreading factors Adherence Factors Numbers parasitization and killing effector cells of host immune system Microbe initiated immunopathogenicity Hiding Protective coating antigenic variation deoys cleave/bind host antibodies masquerade as host antigen |
|
|
Botulism
|
Clostridium botulinum
Botulotoxin is anticholinergic. Prevents release of acetylcholine at the myoneural junction, re¬sulting in flaccid paralysis. |
|
|
Tetanus
|
Clostridium tetani
Tetanus toxin blocks inhibitory synapses by centrally inhibiting release of neurotransmitters, resulting in spastic paralysis. |
|
|
Gas Gangrene
|
Clostridium perfringens
α-Toxin is a phospholipase C or lecithinase, which is cytolytic, necrotizing, and hemolytic. Tissue destruction. |
|
|
Staphylococcal Food Poisoning
|
Staphylococcus aureus
Staphylococcal enterotoxins stimulate brain or peripheral nerves to produce vomiting (?) |
|
|
Staphylococcal Toxic Shock Syndrome
|
Staphylococcus aureus
Toxic shock syndrome toxin-1 causes fever and shock. |
|
|
Staphylococcal Scalded Skin Syndrome
|
Staphylococcus aureus
Exfoliative toxin causes loss of outer layer of epidermis |
|
|
Scarlet Fever
|
Streptococcus pyogenes (Group A)
Strains which secrete erythrogenic toxin possibly via cytotoxin to blood vessels. Phage coded. |
|
|
Diptheria
|
Corynebacterium Diptheriae
Diphtheria toxin inhibits protein synthesis by ADP ribosylating elongation factor 2 and inhibiting protein synthesis. Damage to internal organs results. Toxin is phage coded. |
|
|
Pseudomonas opportunistic infections
|
Pseudomonas aeruginosa
Exotoxin A - mode of action similar to diphtheria |
|
|
Whooping Cough
|
Bordetella pertussis
One strain produces three toxins: Pertussis toxin ADP ribosylates a GTP binding protein. Adenyl cyclase toxin - effects PMN function. Tracheal cytotoxin - toxic to ciliated tracheal epithelium. May be peptidoglycan. |
|
|
Cholera/E-Coli caused travelers diarrhea
|
Vibrio cholerae/ E. Coli
Cholera toxin and E. coli heat-labile toxin alter water and electrolyte balance in intestine by ADP ribosylating a GTP-binding protein which elevates adenyl cyclase with accumulation of cAMP in epithelial cells in gut. This causes the pumping out of elecrtolyes and water osmoses out in response. |
|
|
penetration and spreading factors
|
Hyaluronidases from Streptococci, Group A- Lysis of tissue group substance
Coagulase from Staphylococcus aureus- Clots fibrin Kinases from Staphylococci/Streptococci-Lysis of fibrin |
|
|
Endotoxin Vs. Exotoxin
|
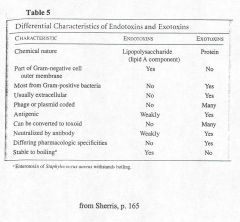
Exotoxin Vs. Endotoxin
|
|
|
Virulence Factor: Nutrient Aquisition
|
Siderophores to chelate Iron
|
|
|
Virulence Factor: Adherence Factors
|
1)Pilus antigens
E. coli and diarrheal disease: CFA = colonization factors for adher¬ence. Bind to intestinal epithelium. E. coli and pyelonephritis: P pili bind to urinary epithelium 2) Bordetella pertussis - filamentous hemagglutinin mediates attach¬ment to tracheal epithelial cells. 3) Streptococcus pyogenes, Group A - lipoteichoic acid binds to fibronectin. |
|
|
Virulence Factor: Parasitize or Kill effector cells
|
Intracellular pathogens of macrophages
2) HIV - infects T cells 3) Leukocidins of streptococci and staphylococci kill PMNs. |
|
|
Virulece factor: Microbe initiated Immunopathogenicity
|
1) Cavitation induced by M. tuberculosis caused by a delayed-type hypersensitivity response.
2) Glomerulonephritis - poststreptococcal immune complex disease 3)Rheumatic fever - poststreptococcal immunopathology causing heart damage 4) Chlamydia and atherosclerosis 5)Guillain-Barré and Campylobacter |
|
|
Virulence factors: Hiding
|
1) Viral latency
e.g., Herpes simplex, herpes zoster (shingles), Epstein-Barr virus (mononucleosis), HIV |
|
|
Virulence Factors: Protective Coat
|
1) Capsules and surface molecules which prevent phagocytosis
a)Streptococcus pneumoniae (pneumococcus) - 83 capsular types - all different polysaccharides b) Hemophilus influenzae, type b, 1 capsular type most frequently associated with meningitis c) Group A streptococci - M proteins 2) Anticomplementary surface Capsules and long chain length lipopolysaccharide of smooth gram-negative enteric pathogens |
|
|
Virulence Factor: antigenic variation
|
e.g., gonococci, trypanosomes, borrelia (relapsing fever), influenza virus
|
|
|
Virulene Factor: Decoys
|
Extracellular capsular polysaccharide is shed and absorbs antibody.
|
|
|
Virulence Factor: Host Antibody Clevage/Binding/Impersonization of antigen
|
1. Clevage- IgA proteases of Hemophilus influenzae, gonococci, and meningococci
2. Bind host antibodies- Staphylococcal protein A binds IgG by the Fc end. 3.Masquerade as a host antigen- The capsule of Neisseria meningitidis Group B is sialic acid identical to that in human neuronal tissue. |
|
|
How can you decide which virulence factor is most crucial for the survival of the organism?
|
A. Dr. Stanley Falkow proposed that we apply Koch’s molecular postulates.
1. The genetic phenotype (i.e. presence of gene for the factor) should be associated with pathogenic isolates. 2. Inactivation of the gene (for example, a toxin) should result in loss of virulence 3. Test the organism to see if it loses virulence (Do an LD50) 3. Replacement of the gene(s) should restore virulence 4. Test to see if virulence is restored. Example: Listeria Monocytogenes 1. By transposon mutagenesis, inactivate the hemolysin (The hemolysis lyses the membrane of the phagosome of the macrophage so the organism can escape into the cytoplasm where it replicates). 2. Organism loses virulence and does not multiply intracellularly 3. Restore the hemolysin gene and virulence and ability to replicate are restored. |
|
|
1. Can a gram-negative organism have an endotoxin and an exotoxin?
|
Yes. Vibrio cholerae is gram-negative and has lipopolysaccharide (LPS) in its outer membrane. It secretes cholera toxin extracellularly.
|
|
|
2. Can capsules be present on gram-negative and gram-positive bacteria?
|
Yes. Pneumococcus is gram-positive. Hemophilus and Neisseria are gram-negative.
|
|
|
3. Can bacteria have more than one virulence factor?
|
Yes and frequently do. In fact, there are regulatory genes which may turn on clusters of virulence factors; for example, a toxin and an adherence factor.
|
|
|
Staphylococcus Aureus
|
1. Gram reaction/Morphology- Gram + cocci aerobe, in grape clusters or alone
2. Synonym, if any- 3. Description of Disease- TSST-1, SSS, 4. Pathogenesis- Protein A (antiphagocytic), Capsule, coag+, Alpha toxin (dermonecrotic, hemolytic, plateletolytic), Exfoliatin, enterotoxin, pyrogenic exotoxin (TSST-1), hyaluronidase, staphylokinase(fibrinolysin) 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- produces golden yellow pigment, B-hemolytic, Catalase +, phage typing possible, coag+, mannitol +, haltolerant 9. Other remarks- penicillinase |
|
|
Staphylococcus epidermidits
|
1. Gram reaction/Morphology-
Gram + cocci aerobe, in grape clusters or alone 2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- opportunistic, 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- white colonies, G-Hemolytic, Catalase + 9. Other remarks- |
|
|
Staphylococcus Saprophyticus
|
1. Gram reaction/Morphology- Gram + cocci aerobe, in grape clusters or alone
2. Synonym, if any- 3. Description of Disease- UTI 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- Catalase + 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |
|
|
?
|
1. Gram reaction/Morphology-
2. Synonym, if any- 3. Description of Disease- 4. Pathogenesis- 5. Transmission/Vector- 6. Therapy- 7. Prevention- 8. Lab Identification- 9. Other remarks- |

