![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
contributing factor
|
|
Contributing Factors
Infectious disease results from a competition for supremacy between the parasite and the host. If the parasite overcomes the host, there is a change in the general state of good health and disease develops. Several contributing factors are involved in the establishment of infectious disease. These factors determine whether the infecting organism will survive in the body. Portals of entry. In order for a pathogen to gain access to the host, the pathogen must pass through a portal of entry. One of the most common portals of entry is the mucous membranes, especially those of the respiratory, gastrointestinal, and urogenital tracts. Another important portal of entry is the skin. Penetration of the skin occurs during a wound or by a hair follicle. When microorganisms penetrate below the skin, the portal of entry is said to be the parenteral route Dose. The dose of an organism refers to the number of microorganisms required to establish an infection. For some diseases, such as typhoid fever, the dose is a few hundred bacteria. For other diseases, such as cholera, the dose may be several million bacteria. The dose may be expressed as the LD50 , which refers to the dose of microorganisms that will kill 50 percent of the hosts it enters. Invasiveness Invasiveness is a property that encourages disease because it refers to the ability of pathogens to penetrate into the tissues. Those organisms that cause intestinal ulcers, such as Entamoeba histolytica, penetrate the tissue effectively. Tissue invasion often begins with adherence, the ability of pathogens to attach to the tissue by using structures such as pili. The presence of a capsule or glycocalyx encourages adherence because they are composed of sticky materials. Capsules. Microorganisms that possess capsules are able to resist host defenses by interfering with phagocytosis. Normally, the body uses white blood cells to engulf and destroy pathogens. However, toxic substances in the capsule are able to destroy the white blood cells before the white blood cells perform phagocytosis. The organism of pneumonia Streptococcus pneumoniae is well known for the toxic materials in its capsule. Many other pathogens also possess capsules. |
|
|
enzyme and toxin
|
aaa
|
Enzymes and Toxins
Enzymes. Many pathogens produce a series of enzymes to help overcome body defenses and establish themselves in the host. One example is leukocidins, a group of enzymes that destroy white blood cells. This destruction lessens the body's ability to perform phagocytosis. Other bacterial enzymes are hemolysins. These enzymes destroy red blood cells. Streptococci, staphylococci, and certain Clostridium species produce hemolysins. Coagulases are bacterial enzymes that clot the blood. These enzymes convert fibrinogen into fibrin, which forms the threads of a blood clot. The clot helps staphylococci avoid the body's phagocytes and contributes to its pathogenicity. Other important enzymes are streptokinase and hyaluronidase. Streptokinase is a streptococcal enzyme that dissolves blood clots. This activity helps the organism escape the body's attempt to wall off an infection. Hyaluronidase destroys hyaluronic acid, a polysaccharide that “cements” cells together in a tissue. Hyaluronidase thus permits organisms to spread through tissues and establish themselves at sites distant from that of the intial infection. Another enzyme, called collagenase, breaks down collagen in the connective tissues of muscles. It thereby encourages the spread of infection. Toxins. Many bacteria are able to produce poisonous substances called toxins. Toxins act on the body's cells, tissues, and organs and interfere with important body processes, thereby interrupting normal body functions. Those microorganisms that produce toxins are said to be toxigenic. The condition in which toxins are produced is called toxemia. Two important types of toxins are exotoxins and endotoxins. Exotoxins are proteins produced by bacteria during their growth and liberated into their surrounding environment. Exotoxins are produced chiefly by Gram-positive bacteria, and the genes for this production are carried primarily on the plasmids. Various types of exotoxins exist. Neurotoxins interfere with the nervous system, while enterotoxins interfere with activities of the gastrointestinal tract. In response to toxins, the body produces special antibodies called antitoxins, which unite with and neutralize the toxins, providing defense against disease. It is possible to immunize against the effects of exotoxins by injecting toxoids into individuals. Toxoids are preparations of exotoxins chemically treated to destroy their toxigenicity but retain their ability to elicit antibody formation in the body. Toxoids are currently available to protect against diphtheria and tetanus (the DT injection). Endotoxins are portions of the cell wall of Gram-negative bacteria. They consist primarily of lipopolysaccharides and are released when bacteria break apart during the process of lysis. Since lysis occurs during antibiotic therapy, the effects of endotoxins can bring about a worsening of symptoms during the recovery period. This condition is called endotoxin shock. It is accompanied by fever, chills, aches, and cardiovascular collapse |
|
|
virus
|
aaa
|
Pathogenic Viruses
Because viruses lack metabolic capabilities, they rely on other means for overcoming body defenses and causing disease. Viruses avoid body defenses by multiplying within host cells, where antibodies and other components of the immune system cannot reach them. The effect occurring in host cells during viral invasion is referred to as the cytopathic effect. The cytopathic effect can develop when the virus alters the metabolism of the cell and prevents it from producing essential cellular components. Alternatively, the virus may induce cells to cling together in a large mass called a syncytium. In some cases, the virus causes the cell's lysosomes to release enzymes which then destroy the cell. |
|
|
non specific
non specific 1st defense natural genetic innate |
aaa
|
Nonspecific Mechanisms of Defense
The body possesses many mechanisms that impart nonspecific defense. The objectives of these mechanisms are to prevent microorganisms from gaining a foothold in the body and to destroy them if they penetrate to the deeper tissues. Mechanical barriers. Mechanical barriers at the portal of entry represent the first line of defense for the body. These defenses are normally part of the body's anatomy and physiology. The skin is a representative example. The outermost layers of skin consist of compacted, cemented cells impregnated with the insoluble protein keratin. The thick top layer is impervious to infection and water. In the unbroken state, it usually is not penetrated by pathogens. The mucous membranes of the urinary, respiratory, and digestive tracts are another example. They are moist and permeable, but their fluids, such as tears, mucus, and saliva, rid the membrane of irritants. Nasal hairs trap particles in the respiratory tract, and the fluids exert a flushing action. Cilia on the cells sweep and trap particles in the respiratory tract, and coughing ejects irritants. Chemical defenses. Among the nonspecific chemical defenses of the body are the secretions of lubricating glands. The tears and saliva contain the enzyme lysozyme, which breaks down the peptidoglycan of the cell wall of Gram-positive bacteria. The lactic acid of the vagina imparts defense, and the extremely caustic hydrochloric acid of the stomach is a barrier to the intestine. Semen contains the antimicrobial substance spermine that inhibits bacteria in the male urogenital tract. Genetic barriers. The hereditary characteristics of an individual are a deterrent to disease as well. For example, humans suffer HIV infection because their T-lymphocytes have the receptor sites for the human immunodeficiency virus. Dogs, cats, and other animals are immune to this disease because they do not possess the genes for producing the receptor sites. Conversely, humans do not suffer canine distemper because humans lack the appropriate receptor sites for the virus that causes the disease. Inflammation. Inflammation is a nonspecific response to any trauma occurring to tissues. It is accompanied by signs and symptoms that include heat, swelling, redness, and pain. Inflammation mobilizes components of the immune system, sets into motion repair mechanisms, and encourages phagocytes to come to the area and destroy any microorganisms present. Inflammation can be controlled by nervous stimulation and chemical substances called cytokines. These chemical products of tissue cells and blood cells are responsible for many of the actions of inflammation. The loss of fluid leads to a local swelling called edema. In some types of inflammation, phagocytes accumulate in the whitish mass of cells, bacteria, and debris called pus. Fever. Fever is considered a nonspecific defense mechanism because it develops in response to numerous traumas. Fever is initiated by circulating substances called pyrogens, which affect the brain's hypothalamus and cause the latter to raise the temperature. Although excessive fever can be dangerous, fever is believed to have a beneficial role because it retards the growth of temperature-sensitive microorganisms (for example, leprosy bacilli), and it increases the metabolism of body cells while stimulating the immune reaction and the process of phagocytosis. Interferon. Interferon is a group of antiviral substances produced by body cells in response to the presence of viruses. Lymphocytes and macrophages produce alpha-interferon, epithelial cells produce beta-interferon, and T-lymphocytes produce gamma-interferon. The interferons do not directly inhibit viruses. Instead, they stimulate adjacent cells to produce substances that inhibit the replication of viruses in those cells. Interferons produced in response to one virus will protect against many other types of viruses, and for this reason, interferon is considered a nonspecific form of defense. |
|
|
non specific- phagocytosis
|
aaa
|
Phagocytosis
Phagocytosis is a nonspecific defense mechanism in which various phagocytes engulf and destroy the microorganisms of disease. Phagocytes. Among the important phagocytes are the circulating white blood cells called neutrophils and monocytes. In the tissues, the monocytes are transformed into phagocytic cells called macrophages. The macrophages move through the tissues of the body performing phagocytosis and destroying parasites. They are part of the reticuloendothelial system. Phagocytes also initiate the processes of the immune system. The process of phagocytosis begins with attachment and ingestion of microbial particles (Figure 1 ) into a bubblelike organelle called a phagosome. Once inside the phagocyte, the phagosome containing the microorganism joins with a lysosome, which contributes enzymes. The fusion of phagosome and lysosome results in a phagolysosome. Microorganisms are destroyed within minutes, and the microbial debris is eliminated from the cell in the process of egestion. In the immune process, chemical portions of the microorganism called antigenic determinants are displayed on the surface of the phagocyte to stimulate the immune process. Figure 1 The process of phagocytosis, a type of nonspecific defense to disease. Phagocytosis is enhanced by products of the immune system called antibodies. These protein molecules bind to microorganisms and encourage engulfing by phagocytosis. The complement system. The complement system is a series of proteins that circulate in the blood and encourage phagocytosis or otherwise “complete” the defensive process. Many immune reactions stimulate the complement system. The complement system operates in a cascade of reactions. In the pathway, certain complement components react with one another and produce new substances that induce other components to react. The results of the myriad reactions are substances that induce other complement components into action. The overall result is a number of substances toxic to microorganisms. The substances encourage phagocytosis or bring about destruction of microbial membranes. Two general pathways for complement activity exist. The classical pathway operates with the highly specific immune system and is initiated when certain antibodies unite with antigens and stimulate the complement system into action. The alternative pathway is nonspecific and is initiated by tumors, cell wall components of bacteria, and various microorganisms. It is sometimes called the properdin pathway because properdin is one of the proteins operating in it. The alternative pathway invokes a slower and less specific method for ridding the body of parasites, particularly Gram-negative bacteria and viruses. |
|
|
specific immune
|
aaa
|
Immunity is a state of specific resistance to infection. Specific resistance is directed against a particular type of microorganism and is the single most important characteristic of immunity.
The immune system enables the body to recognize a foreign agent as nonself, which is something other than a person's own substances (self). The immune system takes a specific action for neutralizing, killing, and eliminating that agent. The action involves nonspecific resistance as well. On occasion, the immune system activity may lead to tissue damage as seen in allergic disorders and other states of hypersensitivity. The immune system's activity is based on its ability to distinguish characteristic proteins or protein-linked components associated with alien substances. Once this distinction has been made, certain lymphocytes are provoked to produce antibodies directed against the foreign matter, while other lymphocytes are sensitized to the invading agent and react with it directly. Thus, there are two major branches of the immune system: antibody-mediated immunity (also known as humoral immunity) and cell-mediated immunity. |
|
|
specific immune
antigen |
aaaaa
|
Antigens
Immune responses are directed at a series of foreign substances known as antigens, also referred to as immunogens. Most antigens are high molecular weight substances, but low molecular weight substances will also act as antigens if they bind to proteins in the body. The low molecular weight compound is referred to as a hapten. The resulting conjugate may induce an immune response directed against the antigen. The uptake and processing of antigens by macrophages in the tissue is an initial, critical step in most immune responses. The simple act of taking foreign substances into the body does not necessarily invoke an immune response because the substances may be broken down before they are ingested by macrophages. Antigenic determinants. The chemical groups on the antigen molecules that determine their immunogenicity are called antigenic determinants, also known as epitopes. Antigenic determinants may consist of several amino acids of a protein molecule or several monosaccharide units of a polysaccharide. Each species of living thing is chemically and antigenically unique because of differences in its proteins, carbohydrates, and other organic substances. Types of antigens. Certain types of antigens are distinctive. Autoantigens, for example, are a person's own self antigens. Alloantigens are antigens found in different members of the same species (the red blood cell antigens A and B are examples). Heterophile antigens are identical antigens found in the cells of different species. A single organism such as a bacterium may contain a variety of proteins, carbohydrates, and other materials that provoke immune responses. Antigens found on the body cell are called somatic antigens. Antigens in the bacterial capsule are capsular antigens. Antigens of an organism's flagella are known as flagellar antigens (H antigens). Protein substances such as exotoxins are also antigenic. |
|
|
specific immune cells
|
aaa
|
Cells of the Immune System
Cells of the immune system are associated with the lymphatic system of the body and its specialized cells. Lymphocytes of the lymphatic system are derived from stem cells of the bone marrow. These undifferentiated precursor cells proliferate throughout life and replenish the mature cells of the immune system. B-lymphocytes and T-lymphocytes. There are two major pathways for the differentiation of stem cells into immune cells. Certain of the stem cells produce B-lymphocytes (B-cells) while other stem cells form T-lymphocytes (T-cells). B-lymphocytes are so named because in birds, they are formed in the bursa of Fabricius. The equivalent site in humans has not been identified but is believed to be the bone marrow. T-lymphocytes undergo their conversion in the thymus gland, an organ in the neck tissues near the trachea and thyroid gland (Figure 1 ). Figure 1 An overview of the human immune system. T-lymphocytes and B-lymphocytes originate in the bone marrow and then are processed in different body organs before proceeding to the lymph nodes, where they provide the underpinnings of the two types of immune responses. The transformation of stem cells into B-lymphocytes and T-lymphocytes begins about the fifth month after fertilization, and a full set is complete a few months after birth. These cells then migrate to the lymphoid organs in the lymph nodes, spleen, tonsils, adenoids, and other organs of the lymphatic system. To initiate the immune response, microorganisms are phagocytized and their antigens are processed in phagocytic cells such as macrophages. The antigenic determinants are displayed on the surface of the phagocytic cells and presented to the appropriate B-lymphocytes and T-lymphocytes to provoke an immune response. Clonal selection. The clonal selection theory helps explain how lymphocytes recognize antigenic determinants and respond. According to this theory, small populations (clones) of lymphocytes bear receptors on their cell membranes. Production of these receptors is genetically determined. On B-lymphocytes, the receptors consist of antibody molecules, while on T-lymphocytes, they are clusters of amino acids. When lymphocytes encounter an antigenic determinant on the surface of a macrophage, their receptors match with the antigenic determinant and a stimulation follows. A match is also made between a set of molecules called major histocompatibility (MHC) molecules and their receptors. The clonal selection theory suggests that B-lymphocytes and T-lymphocytes exist for all antigenic determinants even before contact with an antigen is made. The theory also says that antigenic determinants stimulate the lymphocytes to endow their progeny with identical specificity. The B-lymphocytes and T-lymphocytes that might potentially react with the body's own cells are deleted or in some way inactivated to ensure that an immune response to the host organism does not develop. Two general types of immunity exist for specific resistance to disease. They are antibody-mediated (humoral) immunity, centered in B-lymphocytes, and cell-mediated immunity, centered in T-lymphocytes. |
|
|
B antibody(humor)
AMI |
aaa
|
Antibody‐Mediated (Humoral) Immunity (AMI)
On exposure to antigenic determinants in lymphatic organs, B-lymphocytes are activated and differentiated to form plasma cells. Plasma cells are specialized, differentiated cells that synthesize and secrete antibodies specific for an antigen. Other activated B-lymphocytes form memory cells. These cells can be activated later to differentiate to plasma cells for rapid antibody production. This antibody production will occur on future reentry of the antigen to the body and is the basis of long-term immunity. The products of plasma cells are antibodies. An antibody is a specialized protein substance produced by the host cells in response to an antigen in the host's tissues. Antibodies are capable of reacting specifically with the antigen that provoked their production. Antibodies are often referred to as immunoglobulins. They circulate in the blood and are associated with the gamma globulin fraction of the plasma. Structure of antibodies. Structurally, the antibodies (immunoglobulins) are composed of four protein chains arranged in a distinctive pattern. Each molecule has two long chains of heavy molecular weight protein (H chains) and two short chains of light molecular weight protein (L chains). The chains are linked by sulfur bonds. At the outer end of each arm of the antibody molecule, a specific amino acid sequence exists. This is where the antibody molecule reacts with the antigenic determinant that provoked its production. The combining site is known as the Fab region. The most common antibody molecules have two Fab regions and are said to be bivalent (having two combining sites). The remaining portion of the antibody molecule is called the Fc region because it can be crystallized. Its amino acid content is relatively constant and characteristic for its class. This portion of the molecule activates the complement system and encourages phagocytosis. When the antibody molecule reacts with the antigen, the two surfaces fit together like the pieces of a jigsaw puzzle. This “recognition” is exquisitely accurate and accounts for the extreme specificity of antibody molecules. Classes of antibodies. Five classes of antibodies (immunoglobulins) are produced by the plasma cells. The first class, called IgM, is the major component of the primary antibody response in adult humans and is the first antibody to appear in the immune reaction. It is composed of five units joined by a J (joining) chain (Figure 1 ). IgM cannot diffuse through cell membranes and is found almost exclusively in the blood. Because of its many binding sites, it is more reactive with antigens than are other kinds of antibodies. IgM is also formed by the fetus during uterine development and is active against the A and B factors of the red blood cells. Many antitoxins formed against bacterial toxins are composed of JgM. Figure 1 Details of an antibody molecule and the structures of the five types of antibody molecules produced by the human body. The principal antibody of the secondary immune response is IgG. This antibody is the most common in the bloodstream and is found in many secretions, such as spinal, synovial, lymph, and peritoneal fluids. IgG crosses the placenta and protects the fetus and newborn. IgG therefore provides a natural type of passive immunity. IgG also forms in the primary antibody reaction after a large amount of IgM has already formed. IgG has the “typical” antibody structure of four protein chains. The third class of antibody is IgA. This antibody is found in external secretions such as those at the mucosal surfaces of the respiratory, gastrointestinal, and urogenital tracts. It is also present in the tears, saliva, bile, urine, and colostrum, and it is transferred in the breast milk. IgA consists of two antibody units held together by a J chain and secretory component. IgA resists infections at the body surface. The fourth class of antibody, IgD, is found in extremely small quantities in the serum. IgD is found at the surface of B-lymphocytes and is believed to be an antigen receptor at this location. IgM is also believed to be a receptor. The final kind of antibody, IgE, occurs in minute concentrations in the serum and is important in hypersensitivity reactions, especially the anaphylactic reaction. A localized reaction is called allergy. The reaction of antibodies with antigens helps neutralize the antigen and restrict the spread of infection. Certain antibodies react with the bacterial surface, while others react with the flagella, pili, or capsules. These reactions encourage phagocytosis. When antibodies react with a virus, viruses cannot attach to host cells and replicate. Antibody reaction with antigens also sets off the complement system, which results in the formation of an attack complex along with increased phagocytosis. Antibody reactions with toxin molecules neutralize the toxins and prevent further damage to body tissues. Types of immunity. Immunity may be broadly classified as innate or acquired. Innate immunity is present from birth. It consists of numerous types of nonspecific factors that operate during times of disease. Acquired immunity is derived from activity of the immune system. The term generally refers to antibodies and is subdivided into two parts: active immunity and passive immunity. Active immunity is acquired when the body produces antibodies. The immunity is usually long lasting because the immune system has been stimulated into action. However, it takes several hours to develop. Active immunity can be natural or artificial. Naturally acquired active immunity develops when a person produces antibodies during a bout of illness or on exposure to a microorganism even though disease does not occur. The B-lymphocytes and plasma cells function, and this immunity occurs during the “natural” scheme of events. Active immunity can also occur by artificial means. Artificially acquired active immunity occurs when a person produces antibodies after exposure to a vaccine. A vaccine consists of bacteria, viruses, or fragments of these. A vaccine may also contain toxoids, which are chemically treated bacterial toxins. Toxoid vaccines are available against diphtheria and tetanus. Viral vaccines are available against measles, mumps, rubella, polio, rabies, hepatitis A, hepatitis B, and yellow fever. Because vaccine exposures do not happen in the natural scheme of events, the immunity is said to be artificial. Passive immunity comes about when the body receives antibodies from an outside source. In passive immunity, the immune system does not operate and the immunity is not long lasting. However, it protects instantaneously. Passive immunity can be either natural or artificial. Naturally aquired passive immunity develops when antibodies pass from mother to child across the placental lining. The newborn is born with IgG, and it receives maternal IgA if it is breast-fed. These antibodies will remain for approximately six months after birth before fading away. For artificially acquired passive immunity, a person is given an injection of antibodies. Usually these antibodies are derived from the blood of another individual who has produced antibodies when confronted with a certain disease. The antibody injected is usually IgG. The antibodies will remain for a period of several days or weeks and then disappear. This type of immunity is given to protect people who have been exposed to tetanus, diphtheria, or botulism. It is also used to protect against certain serious viral diseases. Allergic reactions to the serum proteins (serum sickness) limit the use of the preparations. |
|
|
T Cell meditated(cell bound)
CMI |
aaa
|
Cell‐Mediated Immunity (CMI)
Cell-mediated immunity depends upon the activity of T-lymphocytes. T-lymphocytes have a longer life span than B-lymphocytes and are found in the same lymphatic tissues as the B-lymphocytes. The T-lymphocytes react with certain antigenic determinants and become immunologically “committed.” Part of this commitment is the conversion to a subset of cells called cytotoxic T-lymphocytes. Activity of cytotoxic T-lymphocytes. Cytotoxic T-lymphocytes do not produce antibody molecules. Rather, they leave the lymphatic tissues and enter the circulation. They circulate through the blood vessels and gather at the infection site. Here they interact directly with organisms such as fungi, protozoa, cancer cells, and transplant cells. They also interact with virus-infected cells and bacteria-infected cells (such as lung cells infected with tuberculosis). The T-lymphocytes exert a “lethal hit” on the cells and secrete substances into them that lead to cellular destruction. In addition to their direct interaction, T-lymphocytes also secrete substances called lymphokines. Lymphokines attract phagocytes to the area and encourage them to perform phagocytosis on fungi, protozoa, and infected cells. This activity helps relieve the infection. Lymphokines are also known as cytokines. An important cytokine is interleukin-1, which activates T-lymphocytes, causing them to proliferate further and form clones. Helper and suppressor T-lymphocytes. Helper T-lymphocytes also function in the immune system by encouraging the activity of B-lymphocytes in the production of antibodies. Suppressor T-lymphocytes regulate or suppress the activity of the immune system so that it is not excessive. Natural killer (NK) cells are T-lymphocytes that recognize and destroy many types of target cells without being exposed to antigens. Technically, these are not part of the specific immune response. Finally, the delayed hypersensitivity T-lymphocytes function in hypersensitivity reactions and encourage local tissue inflammations. |
|
|
definition of the epidemiology
|
study of causal agents, occurrence, distribution, and control of health and disease in a defined human population
|
|
|
|
term of the epidemiology
|
study of what is upon the people/population
|
|
|
|
population is
|
Population may be defined by:
Age Gender Ethnic group / economics /education Geography Lifestyle Genetics |
|
|
|
health,disease,sign, symtom, syndrome
|
• Health – condition in which an individual performs all vital functions properly (within normal ranges).
• Disease – condition in which vital functions are abnormal or impaired resulting in Signs and Symptoms (s/s). • Sign – an objective, measurable manifestation of disease. (Ex. skin color, tremors, wheezing/coughing, fever, range of motion, vomiting, swelling, BP, blood chemistry) • Symptom – subjective, non-measurable manifestation of disease. (Ex. tired, pain, numb, nausea, anxiety, hunger/thirst) • Syndrome – all of the s/s associated with a particular disease. (Ex. SARS, AIDS) |
|
|
|
causal agent is:
|
I. Causal Agent – the microbe that causes the disease of interest. Once causal agent is identified, may lead to treatments and preventions.
|
|
|
|
How is causal agent identified?
|
Use s/s (Ex. lockjaw = tetanus)
Collect a sample, use classic micro lab tests for ID (Ex. Gram stain, etc.) Use Koch’s Postulates to ID the causal agent. |
|
|
|
(3) Common Statistics used in Epidemiology:
|
prevalence,morbidity,mortality
|
|
|
|
prevalence
|
1. Prevalence – tells us how common the disease of interest is within the population for a given period of time.
Prevalence = (new + old) # of individuals with the disease / total population size |
|
|
|
morbidity
|
2. Morbidity (Incidence) – tells us if the disease of interest is spreading in the population during the given time period.
Morbidity = # of new cases / total population size |
|
|
|
mortalilty is:
|
3. Mortality - tells us how deadly, lethal the disease of interest may be within the population for a given time period.
Mortality = # of deaths due to disease / # of infected individuals |
|
|
|
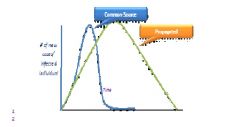
common source is rapidly disappear once eliminated
|
|
|
|
outbreak
|
5. Outbreak – unexpected occurrence of disease usually within a small geographical range or within a small portion of the population.
(Ex. Ebola, SARS, Hanta Virus) |
|
|
|
pandemic
|
6. Pandemic – disease occurs at epidemic levels over large geographical ranges or in large populations (entire countries world-wide).Ex. AIDS, flu in 1960’s, cholera, plague)
|
|
|
|
distribution
|
III. Distribution – examines how the pathogen spreads through the population.
Source / Reservoir – the natural location that supports the growth of the pathogen (causal agent) from which the pathogen may be transmitted to a new host. |
|
|
|
the most common source of the human disease:
|
HUMANS.
When a human is the source, it is called a Carrier. |
|
|
|
the 2 kinds of the source
|
Source may be:
1. Abiotic – non-living source of pathogen. (Ex. food, water, soil) 2. Biotic – living source of pathogen. (Ex. humans, animals |
|
|
|
4 types of the carrier
|
(4) Types of Carrier:
1. Active Carrier – individual has pathogen present, may transmit pathogen to a new host and is showing all s/s of the disease. 2. Convalescent Carrier – individual has recovered from s/s of the disease, but still has pathogen present and may spread pathogen to a new host. 3. Incubatory Carrier – individual has pathogen present, may spread pathogen to new host, but are not YET showing s/s of the disease. 4. Healthy Carrier – individual has pathogen present and may spread to a new host, but will NEVER show s/s of the disease. (Ex. Typhoid Mary) |
|
|
|
tranmission
|
B. Transmission – how does the pathogen travel from the source to a new host?
|
|
|
|
4 main types of the transmission
|
(4) Main Routes of Transmission:
1. Airborne Transmission – a) Aerosols/Droplet Nuclei b) On Dust 2. Direct Contact Transmission 3. Vehicle Transmission – Fomite. 4. vector 1) External V-B 2) Internal V-B |
(4) Main Routes of Transmission: 1. Airborne Transmission – pathogen becomes suspended/airborne from source and travels at least one meter in air to new host. Pathogens may be suspended on: a) Aerosols/Droplet Nuclei – pathogen travels on tiny liquids drops that are usually generated from respiratory secretions. (Ex. sneezing, coughing, laughing, talking) Relatively short-lived, usually only last hours to days. (Ex. flu, pneumonia, TB, measles) b) On Dust – pathogen may travel through air on dust, settled on a surface and become airborne again. Relatively long-lived, usually last days to years. (Ex. staph, strep, anthrax) 2. Direct Contact Transmission – transmission of pathogen requires physical contact between source and new host. (Ex. sex, touching, kissing, placenta, childbirth, nursing, transmission from contact with contaminated food, water, and soil) 3. Vehicle Transmission – pathogen travels from source to a new host via an inanimate object intermediate called a Fomite. (Ex. needle, utensils/glasses, nail, medical supplies, clothing, knobs/rails, shower mats, tooth/hairbrushes) 4. Vector-Borne Transmission – pathogen travels from source to a new host via living intermediate called a Vector. (Ex. mosquitoes, fleas, flies, ticks) (2) Types of Vector-Borne (V-B) Transmission: 1) External V-B Transmission – pathogen is carried on the surface of vector’s body (Ex. Shigella on flies). 2) Internal V-B Transmission – pathogen is carried inside vector’s body, usually in digestive tract. |
|
|
exit mechanism
|
C. Method of Pathogen Exit from Source – how does the pathogen leave?
(2) Mechanisms: 1) Passive Escape – pathogen is expelled/pushed off or out of source with tissue/fluids already leaving the source. Used by MOST pathogens. (Ex. respiratory secretion, feces, urine, etc.) 2) Active Escape – pathogen seeks an exit portal and leaves the source. Used by some parasitic worms. (Ex. lesions, anus, mouth, nose, ears, eyes) |
|
|
|
control
|
IV. Control – identification of individuals in the population that are more susceptible / “at risk” for the disease.
|
|
|
|
(3) Main Factors that Influence Risk/Susceptibility
|
Exposure, Host Defense Mechanisms, Pathogenicity.
|
1) Exposure – how many and which pathogen is an individual likely to come into contact with?
personal hygiene practices occupation geography going to gym / swimming sexual relations diet recreational drug use 2) Host Defense Mechanisms – how good/able is the individual to resist or fight the pathogen? state of immune system – immunocompromised high risk age – elderly and infants high risk/susceptibility genetics vaccinations 3) Pathogenicity – how good/able is the pathogen to cause a state of disease? also known as virulence. |
|
|
virulence
|
pathogenicity
|
|
|
|
infection
|
Infection – a state in which the pathogen is established/growing and dividing in the host, may not be showing any s/s.
|
|
|
|
ID50
|
1. Infective Dose 50 (ID50) – the dose (# of pathogens per unit time) required to cause infection in 50% of an experimental population.
|
|
|
|
lethal dose LD
|
2. Lethal Dose 50 (LD50) – the dose of pathogen required to kill 50% of the experimental population.
|
|
|
|
4 host defense mechanism
|
(4) Main Categories of Defenses:
1. General Barriers 2. Physical and Mechanical Barriers 3. Chemical Barriers 4. Biological Barriers |
|
|
|
4 kinds of general barrier
|
1. Age – infants and elderly are more susceptible to disease/increased severity.
2. Nutrition – state of malnutrition increases susceptibility to and severity of disease. 3. Genetics – genetic diversity/mutations may increase or decrease susceptibility/severity of disease. Ex. Sickle Cell Anemia and Malaria – carriers of sickle cell mutation are more resistant to malaria (protozoan cannot divide in sickled blood cells) 4. Fever – an increase in thermal set point above 98.6F/37C |
|
|
|
Fever
|
4. Fever – an increase in thermal set point above 98.6F/37C
How is Fever Protective? May possibly SLOW the growth of an extremely temp-sensitive pathogen. Speeds metabolism to aid repair of damaged host tissues. Enhances actions of Non-Specific and Specific Immune Systems (part of Biological Barriers). Stimulates Hypoferremia Reduction in available iron in the blood which is required as a macroelement for pathogen growth May slow or stop pathogen growth |
|
|
|
fever causing element
|
Pyrogen, from toxin, endotoxin,antibody complex, cytokine, gram - negative kipid a lps macro interleukinehyperthalmus(prostagladin)
|
|
|
|
(3) Main Factors that Influence Risk/Susceptibility
|
Exposure, Host Defense Mechanisms, Pathogenicity.
|
1) Exposure – how many and which pathogen is an individual likely to come into contact with? personal hygiene practices occupation geography going to gym / swimming sexual relations diet recreational drug use 2) Host Defense Mechanisms – how good/able is the individual to resist or fight the pathogen? state of immune system – immunocompromised high risk age – elderly and infants high risk/susceptibility genetics vaccinations 3) Pathogenicity – how good/able is the pathogen to cause a state of disease? Warm up – What are the (3) Main Factors that influence risk/susceptibility? Exposure, Host Defense Mechanisms, Pathogenicity. PATHOGENICITY – also known as virulence. |
|
|
virulence
|
pathogenicity
|
|
|
|
infection
|
Infection – a state in which the pathogen is established/growing and dividing in the host, may not be showing any s/s.
|
|
|
|
ID50
|
1. Infective Dose 50 (ID50) – the dose (# of pathogens per unit time) required to cause infection in 50% of an experimental population.
|
|
|
|
lethal dose LD
|
2. Lethal Dose 50 (LD50) – the dose of pathogen required to kill 50% of the experimental population.
|
|
|
|
3 mail factors of the viruvalance
|
infectiveness invasiveness, potential
|
(3) Main Factors that Contribute to Virulence:
1) Infectivity – ability to colonize/establish an initial site of infection on the host. Infectivity improved by: • Presence of a glycocalyx – attachment • Presence of a pili and/or fimbriae • Adhesins – compounds on the surface of pathogen that allow it to attach to host cell. 2) Invasiveness – ability to spread beyond the initial site of infection. Invasiveness improved by: • Motility (flagella, cilia, pseudopodia) • Enzymes that facilitate movement of pathogen through tissues of host. Ex. gelatinase, collagenase, hyaluronidase – movement through connective tissue) Ex. neuraminidase – movement through epithelial tissue Ex. streptokinase, staphylokinase – inhibit blood clotting 3) Pathogenic Potential – ability to cause malfunction and/or destruction of host tissues. Pathogenic Potential improved by: Ability to cause (2) Types of Damage a) Direct Damage • Damage is caused by presence/growth of the pathogen. • Pathogen MUST be present to cause damage. • Damage is limited/localized to location of the pathogen in host. Ex. Enteroaggregative E. coli – causes direct damage in large intestine. To body Lumen Water To body Ex. Lysogenic Cycle of Viruses – virus invades host cell, takes over host cell, uses host cell to make more viruses, host cell lyses to release new viruses. b) Intoxication • Damage/malfunction caused by toxins released from the pathogen. • Pathogen may not be present. • Damage usually is not limited to location of toxin release (better spread through host). (2) Types of Toxins i. Exotoxins Always proteins, usually with enzymatic function/ability. Exotoxins are actively made and secreted by the pathogen into host. Once secreted, exotoxins usually travel to a specific tissue target in host. (Ex. neurotoxins, enterotoxins) Once exotoxins reach target tissue, usually enter host cells and cause damage from within cell. Damage may be: • ADP-Ribosylation – exotoxin causes ADP-Ribose to be attached to specific proteins in host cell, once attached, these host cell proteins are inactivated (malfunction). • Inhibit protein synthesis in host cell by cleaving part of the ribosome (no translation). • Exotoxins inhibit intracellular transport within host cell. Ex. Botox – a neurotoxin that blocks the release of neurotransmitters that stimulate muscle contraction. Result = Muscle Paralysis Ex. Tetanospasmin – a neurotoxin that blocks the release of neurotransmitters that inhibit contraction. Result = Uncontrolled Contraction (lockjaw) • Exotoxins usually create very pathogen-specific signs and symptoms. Ex. lockjaw = Tetanus ii. Endotoxins Most are not proteins, no enzymatic ability. Endotoxins originate as structural component of the pathogen. (Ex. part of cell wall) Endotoxins are passively released when pathogen lyses or during cell division. Once released, endotoxins circulate in blood, lymph, interstitial spaces of host (no specific tissue target). Do no enter host cells. Endotoxins cause broader, more general (not pathogen-specific) s/s in host. S/S of endotoxins depends on endotoxin concentration. At Low Concentration • Fever • Aches • Weakness • Chills • Inflammation At High Concentration • Stimulates formation of blood clots • Decrease blood pressure • Septic shock • Death Ex. Lipid A of Lipopolysaccharides (LPS) of Outer membrane of Gram(-) bacteria |
|
|
4 host defense mechanism
|
(4) Main Categories of Defenses:
1. General Barriers 2. Physical and Mechanical Barriers 3. Chemical Barriers 4. Biological Barriers |
|
|
|
4 kinds of general barrier
|
1. Age – infants and elderly are more susceptible to disease/increased severity.
2. Nutrition – state of malnutrition increases susceptibility to and severity of disease. 3. Genetics – genetic diversity/mutations may increase or decrease susceptibility/severity of disease. Ex. Sickle Cell Anemia and Malaria – carriers of sickle cell mutation are more resistant to malaria (protozoan cannot divide in sickled blood cells) 4. Fever – an increase in thermal set point above 98.6F/37C |
|
|
|
Fever
|
4. Fever – an increase in thermal set point above 98.6F/37C
How is Fever Protective? May possibly SLOW the growth of an extremely temp-sensitive pathogen. Speeds metabolism to aid repair of damaged host tissues. Enhances actions of Non-Specific and Specific Immune Systems (part of Biological Barriers). Stimulates Hypoferremia Reduction in available iron in the blood which is required as a macroelement for pathogen growth May slow or stop pathogen growth |
|
|
|
fever causing element
|
Pyrogen, from toxin, endotoxin,antibody complex, cytokine, gram - negative kipid a lps macro interleukinehyperthalmus(prostagladin)
|
|
|
|
fever
|
How is Fever Protective?
May possibly SLOW the growth of an extremely temp-sensitive pathogen. Speeds metabolism to aid repair of damaged host tissues. Enhances actions of Non-Specific and Specific Immune Systems (part of Biological Barriers). Stimulates Hypoferremia Reduction in available iron in the blood which is required as a macroelement for pathogen growth May slow or stop pathogen growth |
|
|
|
Mechanical Barriers
|
parts of host that eliminate pathogens by washing/flushing action. (Ex. tears, sweat, saliva, mucus, vaginal secretions, urination, defecation, ear wax, vomit)
|
|
|
|
Physical Barriers
|
parts of host that directly block pathogens from invading host.
|
|
|
|
2 physical barrier
|
a. Skin
Composed of multiple layers of tough/keratinized cells with tight junction (difficult to penetrate). Dry – invading microbes must be able to adapt to colonize (Osmotolerant). Oily – creates a film on surface that is difficult to penetrate. Mildly Acidic – invading microbes must be able to adapt to colonize. Continuous shedding of skin cells makes colonization difficult. Frequent washing makes colonization difficult. Normal Microbiota of Skin – microbes already living on skin (non-pathogenic on skin). Outcompete invading pathogens for nutrients, attachment sites, etc. (more later, part of Biological Barriers). b. Mucous Membranes – line surfaces of respiratory, digestive, urogenital tracts (secretes mucus which traps microbes and is difficult to penetrate). |
|
|
|
Chemical Barriers –
|
compounds created by the host that protect against pathogens.
|
|
|
|
Examples of Chemical Barriers:
|
1. Transferrin (in blood) and Lactoferrin (in mucus and tears) – iron-binding proteins created in response to infection (reduce available iron).
2. Lysozyme – an enzyme found in saliva, tears, mucus, sweat, which degrades peptidoglycan (most effective against Gram(+) bacteria). 3. Interferon – compounds made by host cells that have been invaded/infected by some viruses. Infected host cell secretes interferon which travels to other (uninfected) host cells and allows them to be protected against the virus. 4. Complement System – compose of about (20) different proteins that circulate in the host in an inactive state. Infection or intoxication may trigger the activation of complement proteins. Activation occurs in a step-wise/cascade fashion. (Ex. The Classical Complement Pathway: Involves C1-C9) Infection/intoxication: Activate c3 The Protective Roles of C3a and C3b: a) C3b – attaches to surface of pathogen, stimulates insertion of the Membrane Attack Complex (MAC) which is composed of C5-C9. MAC creates pores/holes in pathogen leading to lysis. C3b – Attaches to pathogen for Opsonization (“to make tasty”). Acts like handles for phagocytes to grab onto, which facilitates Phagocytosis of the pathogen. b) inflammation C3a – seeks white blood cells (WBC) called Basophils. C3a – stimulates Basophils to release histamine which stimulates/enhances the inflammatory response. C5a |
|
|
|
biological barrier
|
IV. Biological Barriers – protection against invading pathogens/toxins provided by living cells.
1. The Normal Microbiota – microbes that are the non-pathogenic, usual residents of the human body. About 100 trillion from 500-1,000 different species (primarily bacteria). Provide protection by: a) Outcompete invading pathogens for attachment sites, nutrients, etc. b) Modify the local environment to make colonization by invading pathogens more difficult (Ex. acidity of skin and vagina). c) Secrete toxins against invading pathogens. 2. The Immune System – includes: Non-Specific and Specific Immune Systems. Common Goal – to recognize and destroy any foreign/”non-self” pathogens or toxins without harming “self”. Differences between Non-Specific and Specific Immune Systems: Non-Specific Immune System: • Many cells able to respond to pathogens/toxins • Rapid response • Able to recognize and destroy many different pathogens/toxins (target is general) Specific Immune System: • Fewer cells able to response • Slower response • Target is Unique – cells only recognize one particular pathogen/toxin (Antigen-Specific) • Capable of Memory – if the same pathogen/toxin enters host in future, cells mount a stronger, faster, longer-lasting response. |
|
|
|
The Non-Specific Immune Defenses:
|
a) Phagocytes b) Natural Killer Cells (NKCs) – a subset of WBC called Lymphocytes with non-specific recognition (most Lymphocytes are part of Specific Immune Defenses).
c) The Inflammatory Response |
|
|
|
nkc
|
• NKCs are able to recognize host cells that have been invaded by some viruses (Ex. measles, Epstein-Barr) and some cancerous host cells.
• NKCs are stimulated by Interferons or Cytokines from Phagocytes. • NKCs destroy/kill invaded host cell by secreting (2) compounds: i. Perforins – create holes in plasma membrane leading to lysis. ii. Granzymes – cause host cell to begin “programmed cell death” (a.k.a. Apoptosis – cell suicide). |
|
|
|
4) Types of Phagocytes:
|
• Macrophages – compose about 2-10% of WBC population, slower to site of infection/intoxication, but remain longest and most efficient (best “eaters”).
• Neutrophils – most numerous, 50-70% of WBC population, quick to site of infection/intoxication, but not as efficient as Macrophages. • Eosinophils – less numerous, 1-4% of WBC population, only considered weakly phagocytic, but can secrete toxins against some parasitic worms. • Basophils – least numerous, less than 1% of total WBC population, may only be weakly phagocytic, but do release histamine which enhances the inflammatory response. |
Steps in Phagocytosis
i) Adherence – pathogen/toxin sticks/attaches to surface of phagocyte. Blocked by presence of a glycocalyx, but improved by Opsonization (C3b). ii) Engulfment – phagocyte uses extensions of plasma membrane to enclose pathogen/toxin into a membrane-bound vesicle called a Phagosome. iii) Phagolysosome Formation – phagosome fuses with a lysosome (Phagolysosome) allowing digestive contents of lysosome to mix with contents of phagosome. iv) Digestion – digestive enzymes degrade contents of Phagolysosome into small subunits. Any useful compounds can be recycled into the phagocyte. v) Exocytosis of Residual Body – anything remain in Phagolysosome is called the Residual Body and expelled from phagocyte by Exocytosis. In residual body, may have Endotoxins. |
|
|
iflammation
|
c) The Inflammatory Response
Signs and symptoms that include: • Redness • Swelling • Pain • Heat • Reduced range-of-motion if near a joint Goals of Inflammation: • Eliminate any pathogens or toxins • Prevent spread of pathogens/toxins in the host • Set up for and repair any tissue damage (healing) Steps in Inflammation: i. Chemical Alarm – damaged host cells secrete a variety of compounds including: histamine, kinins, prostaglandins, complement proteins. ii. Chemical Alarm causes vasodilation of blood vessels near the injury site (increases the blood flow to area resulting in redness and heat). Heat increases cell metabolism to speed repair. iii. Chemical Alarm increases permeability of blood vessels near the injury (vessels become “leaky”). Plasma (fluid) from blood leaves vessels and flows into tissue around injury (resulting in swelling and pain). Fluid contains: • May dilute concentration of any toxins present. • Brings oxygen and other nutrients to help repair site. • Clotting factors create a barrier around site to prevent spread and serves as a matrix for tissue repair. iv. Chemical Alarm stimulates mobilization of Phagocytes to the site of infection/intoxication. Phagocytes eliminate pathogens, toxins, and damaged host cells: • Basophils release histamine (enhances Chemical Alarm) • Neutrophils (quick, but short-term response) • Macrophages (slower, but longer-term, most efficient) v. Later may have involvement by Specific Immune Defenses and increased complement protection. May lead to accumulation of PUS = combination of dead/damaged host cells, dead pathogen, living host cells, living pathogen, toxins. |
|
|
|
2 kinds of specific immune
|
The Specific Immune Defenses:
Have (2) Branches: 1. Humoral or Antibody-Mediated Immunity 2. Cell-Mediated Immunity • Both branches are Antigen-Specific. • Antigen-Specific – specific immune cells are only able to recognize one particular antigen. • Antigen – any compound (usually large and complex) that is foreign or “non-self” and stimulates BOTH Antibody-Mediated and Cell-Mediated Immunities. |
|
|
|
antigen
|
Chemical Structure of an Antigen could be:
Lipid Carbohydrate Protein – tend to be the most complex – tend to be the strongest antigens Nucleic acid Where do Antigens come from/originate? • Antigens come from microbes/pathogens entering the body. Ex. cell wall component, part of flagellum, part of glycocalyx, Exotoxins or Endotoxins • In the host, antigens may be pathogen-associated, attached to the pathogen. Ex. cell wall component OR free-floating released from the pathogen (toxins) • Antigens may be found circulating in host (blood, lymph, interstitial spaces) • Antigens may be outside of host cells (extracellular antigens) Ex. Endotoxins • Antigens may be inside of host cell (intracellular antigens) Ex. virus after entering host cell (Exotoxins) • One Antigen may have many Epitopes (a.k.a. Antigenic Determinants) Epitope – a region of the antigen that is able to stimulate an independent response from the Specific Immune System. |
|
|
|
Antigen-Specific –
|
• specific immune cells only recognize ONE Epitope of ONE Antigen.
Optional Assignment: Email Pool Deadline for Host Defense Mechanisms = Thu/May 20 Warm up – Define Antigen? Any compound (usually large and complex) that is foreign or “non-self” and stimulates BOTH Antibody-Mediated and Cell-Mediated Immunities. Antigens may be: 1. Pathogen-Associated / Cell-Bound – antigen is attached to pathogen. 2. Free-floating / Soluble – antigen is released from pathogen. 3. Extracellular Antigen – antigen that does not enter host cells. 4. Intracellular Antigen – antigen that enters host cells. |
|
|
|
antibody=humoral
|
b
|
I. Humoral or Antibody-Mediated Immunity Response
• Protection provided by WBC’s called B Lymphocytes (B cells). • B cells originate in the bone marrow. • B cells mature in the bone marrow. • Once mature, B cells display 10,000 to 100,000 receptors on surface. • Each receptor recognizes one Epitope of one Antigen. • Mature B cells circulate in host, migrate to lymph nodes, spleen and wait for their antigen to arrive. • When antigen is seen, it binds to receptors on B cell causing ACTIVATION of the B cells. • Activated B cells divide to form many Clone cells (all identical to original B cell). • Clone cells differentiate into one of 2 cell types: a) Plasma Cells (Most of clone) – Plasma cells make and secrete antibodies, 2,000/second for 4-5 days and then die. Each antibody (a protein) is able to recognize and bind to the same Epitope as original B cell. b) Memory B Cells – remain in body, long-lived, and wait for same antigen to return in the future. If it does, memory cells create a faster, stronger, longer-lasting response. What do Antibodies do? (4) Mechanisms of Antibody Action: 1. Neutralization – antibodies coat the surface of the pathogen which inactivates the pathogen by disabling the pathogen’s ability to interact with host cells. No interaction = No damage 2. Agglutination – antibodies bind to Cell-Bound (Pathogen-Associated) antigens causing them to clump together which inactivates them. 3. Precipitation – antibodies bind to Soluble (free-floating) antigens causing them to clump together which inactivates them. All (3) mechanisms above lead to Opsonization. 4. Lysis by Complement Fixation – antibodies stimulate Complement System activation that leads to: C3b insertion of MAC Lysis C3b opsonizes enhances Phagocytosis C3a seeks Basophils Histamine releases enhances Inflammation Antibodies have a PLAN (Precipitation Lysis Agglutination Neutralization). Antibodies cannot enter host cells, only effective against Extracellular antigens (Endotoxins). What about Intracellular antigens (Exotoxins)? It is Cell-Mediated Response. |
|
|
cell bound
|
t
|
II. Cell-Mediated Immunity Response
• Protection provided by T Lymphocytes (T cells) • T cells originate in the bone marrow. • T cells mature in the Thymus. • Once mature, T cells display receptors on surface with “Double-Recognition” (receptors recognize 2 different compounds simultaneously): a) The Major Histocompatibility Complex (MHC) – is displayed by host cells to identify them as “self”. b) One Epitope of one Antigen – host cells that have been invaded/infected may display Antigens with their MHC. • Mature T cells circulate in host; look for host cells displaying MHC and their antigen. • Once host cell is found, causes activation of the T cell. • Activated T cell divides to form many Clone cells. • Clone cells differentiate into one of 4 cell types: 1. Cytotoxic T Cells – kill the infected/invaded host cell by: Secrete Perforins – lysis Secrete Lymphotoxin – degrades host cell’s DNA (cell death) Secrete Tumor Necrosis Factor – causes “programmed cell death” (Apoptosis – cell suicide) 2. Helper T Cells – stimulate proliferation and actions of other T and B cells, enhance their protective actions. 3. Suppressor T Cells – secrete compounds that suppress the actions of other T cells once pathogen is gone. 4. Memory T Cells – long-lived, remain in body and wait for same antigen to return in the future, if it does, mount a stronger, faster, longer-lasting response. Helper T Cells are the ones being attacked by AIDS virus. |
|
|
antimicrobial drug
|
ANTIMICROBIAL DRUGS
Selective Toxicity – if the drug targets a unique feature (structure or pathway) of the pathogen, then the drug should ONLY damage the pathogen without causing harm to the host. Ex. Penicillin inhibits synthesis of peptidoglycan – good Selective Toxicity (our cells are LACK peptidoglycan, target of the drug is unique to pathogen) Based on Selective Toxicity: • Viruses are relatively difficult to develop drugs against (simple structure and use OUR cell resources to replicate). • Bacteria are relatively easy because they are procaryotes and have cell structure most different from ours (eucaryotes). • Fungi, algae, protozoans are all eucaryotes like us, more difficult to develop drugs against (not as many unique targets). |
|
|
|
Characteristics of Antimicrobial Drugs
|
1. Source of Drug – maybe:
a. Natural – a compound made by another living organism. (Ex. Penicillin made by a mold) b. Synthetic – drug is created/invented in the lab. (Ex. Sulfa drugs) c. Semi-Synthetic – drug begins as a natural drug and then is altered slightly in the lab (often used to restore effectiveness of the drug if resistance occurs). (Ex. Tetracycline) 2. Range and Strength of Action – maybe: • Broad Spectrum vs. Narrow Spectrum • Cidal vs. Static Ex. Penicillin – narrow but cidal Tetracyline – broad but static 3. Therapeutic Index (TI) – a measure of Selective Toxicity. TI = Ex. (2) drugs to treat same infection (A and B): Drug A: 50 mg Drug B: 500 mg 25 mg 25 mg Which is the “better” drug? Drug B (requires a higher dose to be toxic to the host). • Higher TI = better Selective Toxicity = better drug • Lower TI = lower Selective Toxicity = drug will have unintended/undesirable effects on host = Side Effects (Ex. nausea, vomit, diarrhea, cramps, heart attack, death, etc.) |
|
|
|
Mechanisms of Drug Action
|
1. Cell Wall – drug degrades or inhibits the synthesis of cell wall components.
Relatively high TI (target is unique, our cells lack cell walls) 2. Inhibit protein synthesis by binding to/or altering ribosome structure. Relatively low TI (our cells have ribosomes too) 3. Inhibit nucleic acid synthesis (Transcription or DNA Replication). Relatively low TI (enzymes and pathways are similar to ours) 4. Act as a Structural Analogue – the drug mimics a substrate in a metabolic or biosynthetic pathway necessary for pathogen growth. When drug is used by pathogen, it creates a non-functional end-product No pathogen growth. Relatively high TI (our cells do not make folic acid – lack this pathway) Ex. Biosynthesis of Folic Acid (vitamin required for pathogen growth) |
|
|
|
Drug Resistance –
|
pathogen is not killed or inhibited by the drug, drug no longer has an effect on pathogen. Currently, the greatest threat to successful treatment of microbial disease.
Resistance Evolves – has (2) steps: 1) Genetic Change – in pathogen that allows a few individuals in pathogen population to resist the drug. Genetic change through Mutation or Genetic Recombination. 2) Selection – eliminate all susceptible individuals and allow resistant ones to become predominant (the majority). Caused by the use of drug. Mechanism of Drug Resistance: 1) Block entry of drug 2) Efflux – use Active Transport to pump drug out 3) Degrade or inactivate the drug (Ex. penicillinase) 4) Alter the target pathway or structure so it is not recognized by the drug. |
|
|
|
lympocyte cell
|
t,b,nk
|
erythroid stem... RBC
myeloid stem...plateletes,.WBC lymphoid stem...lympocyte(t b nk). |
|
|
WBC
|
a granular...mono..macro, lympo(t,b,nk)
graular..neu,eosi baso |
|
|
|
VIRUSES
|
Currently considered non-living because:
• Simple, Acellular structure/function – no ribosome, cell walls, flagella, metabolism, biosynthesis, active transport, etc. • Have DNA or RNA but never both. • Inability to replicate outside of a host cell. |
|
|
|
Viral Structure
|
1 size
2. Nucleic Acid Core – present in all viruses. 3. Capsid – a protein coat around the nucleic acid (present in all viruses). 4. Envelope – an additional layer exterior to the capsid, NOT present in all viruses. |
1. Size – average 10-400 nm • Smallest viruses – approximately size of procaryotic ribosome. • Largest viruses – approximately size of an average procaryotic cell. 2. Nucleic Acid Core – present in all viruses. Maybe: • ds DNA (Double Stranded) • ss DNA (Single Stranded) • ds RNA • ss RNA Amount of nucleic acid varies: • Small viruses – 3-4 genes • Large viruses – 100+ genes Viruses commonly have Overlapping Genes: • Non-Overlapping - • Overlapping - 3. Capsid – a protein coat around the nucleic acid (present in all viruses). Capsid Features: • Usually composed of one to a few protein subunits called Protomers or Capsomers, repeated over and over. Efficient – fewer proteins require fewer genes in genome. • Capsid proteins are able to self-assemble. Efficient – does not require additional enzymes to construct the capsid. • Common Capsid shapes: a) Helical Capsid – hollow tube shape. Efficient – use only enough capsid protein to cover nucleic acid, no waste space. b) Icosahedral Capsid – roughly spherical, ball-shape. Efficient – an efficient shape for enclosing a space. c) Complex Capsid – usually a combination of helical and icosahedral (may also have accessory fibers, pins, etc.). 4. Envelope – an additional layer exterior to the capsid, NOT present in all viruses. Structure – similar to a Plasma Membrane: • Phospholipid Bilayers • Sterols (if host cell is eucaryotes) • Proteins called Spikes or Peplomers – viral origin, made from viral genes. |
|
|
The Viral Replication Cycle
|
1. Adsorption – the virus uses a protein from capsid or envelope to bind to a receptor on the surface of a host cell.
2. Penetration and Uncoating – virus enters cell and releases viral nucleic acid inside host cell. (3) Entry Mechanisms: a) Naked Virus Entry • Used by non-enveloped viruses. • Only viral nucleic acid enters host cell. • Capsid remains on host cell surface. b) Fusion • Used by enveloped viruses. • Envelope of virus fuses with plasma membrane of host cell. • Capsid enters host cell and releases nucleic acid. • Spikes from viral envelope remain on host cell surface. c) Receptor-Mediated Endocytosis • Viral spikes stimulate endocytosis of entire virus. • Once inside host cell, viral envelope fuses with vesicle membrane to release capsid and viral nucleic acid. • No viral components remain on cell surface. 3. Biosynthesis of New Viral Components – virus takes over host cell energy, resources, machinery to create new viral structures: • Copies of viral nucleic acid • Capsid proteins • Spikes/Peplomers – as made, become inserted into host cell plasma membrane. 4. Nucleocapsid Assembly – capsid proteins begin to self-assemble around the copies of the viral nucleic acid (nucleocapsid). 5. Release of Newly Created Viruses (2) Exit Mechanisms: a) Lysis of Host Cell – used by Naked (non-enveloped) viruses, accumulate inside host cell until host cell explode. b) Budding – used by Enveloped Viruses, nucleocapsid pushes out against host cell plasma membrane (which already contains viral spikes) until a portion of host cell plasma membrane pinches off to become the Envelope. |
|
|
|
Cytotoxic Effects of Viruses on Host Cells:
|
• Lysis when new viruses are released.
• Mutation of host cell genome by insertion of viral genome. • Depletion of host cell plasma membrane by excessive budding. • Virus uses all host cell resources, none left for host cell. • Host cell destructed by host defenses. • Viral components being made cause excessive bulk inside host cell leading to malfunction. • Viral infection stimulates host cell to become cancerous. |
|

