![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
How do salivary glands develop?
|
out-pouchings of the oral epithelium migrate into the surrounding mesenchyme (much like early teeth-forming cells) and migrate to their final position.
|
|
|
major salivary glands
|
-parotid: just anterior to the ear, long duct in the cheek
-sublingual: alongside base of the tongue w/ many small ducts -submandibular: inside angle of the mandible w/ medium length duct at front base of the tongue |
|
|
acini
|
Secretory cells are located in blind-ended cul-de-sacs and secrete:
-Serous solution (water + proteins) -Mucus secretion -Mixed mucoserous solution |
|
|
Describe the journey of saliva from acinus to salivon.
|
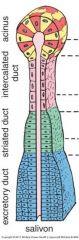
-acinus: cuboidal epith.
-intercalated duct |
|
|
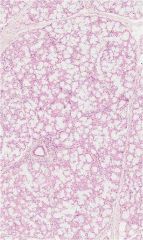
parotid gland
|
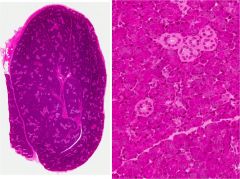
-mostly serous saliva
-basophilic acinar clusters -significant adipose deposits |
|
|
submandibular gland
|
-50/50 mixed serous & mucous
|
|
|
serous demilune
|
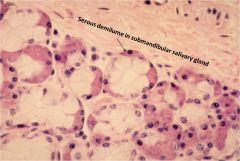
in slide preparation, serous glands get pushed out of the acinar ring to the outside of the mucous glands... in vivo they alternate side-by-side
|
|
|
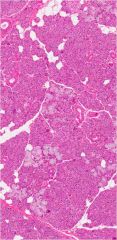
sublingual gland
|
-mixed secretion, but mucous predominates
|
|
|
α-amylase
|
salivary enzyme which begins digestion of carbohydrates
|
|
|
lysozyme
|
salivary enzyme that kills bacteria
|
|
|
sialolith
|
protein and mineral crystalization which can build up in salivary glands and ducts
|
|
|
Why does radiation treatment cause tooth decay?
|
saliva has phosphate and calcium ions to help maintain mineralization of teeth; loss of salivary gland function following radtiation treatment results in severe tooth decay
|
|
|
hemosiderin granules
|
iron storage in the liver
|
|
|
hepatic sinusoids
|
channels formed by hepatocytes through which blood flows; sinusoidal capillaries formed by hepatocyte-endothelial cells
|
|
|
Hepatocytes are stabilized by _____ fibers, which are smaller than type __ collagen and do not impede the flow of blood past the hepatocytes and other cells.
|
reticular, type I
|
|
|
Portal Triad (4 items)
|
-portal vein: deoxy blood from gut tube
-hepatic artery: oxy blood from aorta -bile duct: carries bile from liver -lymphatic vessel: run alongside the other 3 but are not actually visible |
|
|
central vein
|
blood from both the hepatic arteries (oxygenated) and the portal veins (deoxygenated) empty into the hepatic sinusoids and drain to a central vein. This blood will eventually reach the inferior vena cava.
|
|
|
What is the composition of blood that comes from the portal vein?
|
Roughly 75% of the blood comes from the portal vein and contains nutrients, erythrocyte breakdown products from the spleen, and other digested material. Because of this arrangement, hepatocytes rarely receive well-oxygenated blood.
|
|
|
Describe the arrangement of the Classic Lobule.
|
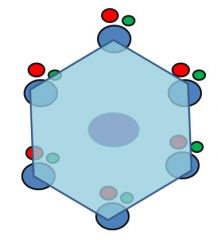
hexagon w/ central vein in the center & portal triads in the corners; highlights flow of blood
|
|
|
Describe the arrangement of the Portal Triangle.
|
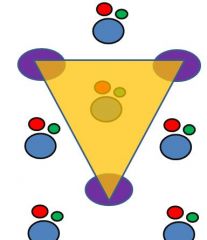
portal triad in the center & central veins in the corners; highlights drainage of bile to ducts
|
|
|
Describe the arrangement of the Liver Acinus.
|
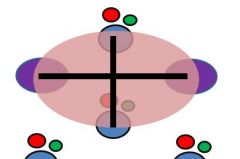
football shaped hexagon w/ two portal triads on the short axis and two cenral veins on the long axis; highlights hepatic metabolism and physiology
|
|
|
For the liver acinus model, in which zone do hepatocytes receive the most oxygenated blood? What is the negative consequence?
|
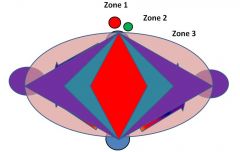
Zone 1 hepatocytes receive the most oxygenated blood because they are closet to the portal triad; consequently, they are the first to be damaged by toxins and/or bile duct occlusion.
|
|
|
Which zone's hepatocytes are the first to die in ischemia or heart failure?
|
Zone 3 hepatocytes are colest to the central veins, so they receive the least oxygenated blood and thus are the first to dies in ischemia or heart failure.
|
|
|
Hemochromatosis
|
Too much iron storage leading to damage of liver and other organs; can cause pain and be mistaken for fibromyalgia. 1/200 ppl of European descent. Tx: bloodletting
|
|
|
perisinusoidal space (of Disse)
|
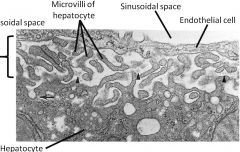
Located between endothelial cells of capillaries and hepatocytes; filled by hepatocyte microvilli that absorb and release their goodies into the perisinusoidal space. Blood forms here in early life and can start again if needed.
|
|
|
Stellate Sinusoidal Macrophages (Kupfer cells)
|
-Location: alongside hepatic endothelial cells
-Fnx: phagocytose foreign material and damaged cells -Other: following splenectomy, removal of damged erythrocytes |
|
|
Hepatic Stellate cells (Ito cells)
|
-Deposit type I collagen in cirrhosis liver repair
-Store vitamin A |
|
|
How is bile produced in the liver kept separate from sinusoidal capillaries?
|
Bile is kept w/in specialized canaliculi that sandwiched between hepatocytes
|
|
|
Trace the path of bile from caniliculi to the duodenum:
|
Bile caniliculi
(btw hepatocytes) ↓ Intrahepatic bile ductules (collect multiple caniliculi) ↓ Interlobular bile ducts (part of portal triad) ↓ Hepatic & common bile ducts (large ducts) ↓ Hepatopancreatic ampulla (pancreatic duct + common bile duct) ↓ Duodenum |
|
|
Cholangiocytes
|
-Cuboidal/columnar cells that line the bile ducts in portal triads
-Microvilli on surface w/ one long sensory cilium that monitors bile flow rate |
|
|
How is bile flow regulated?
|
Endocrine and autonomic nervous system can slow rate of flow, but it never actually stops.
|
|
|
Gall bladder
|
-Stores, concentrates and releases bile produced in the liver.
~90% of water is removed from bile by microvilli of simple columnar epith. cells lining the gall bladder -Active transport of Na+, Cl- and HCO3- ions from the bile causes water to follow passively through specialized channels |
|
|
What causes gall bladder contraction and subsequent release of bile into the duodenum?
|
Fat in the duodenum's lumen stimulates release of hormones to signal for contraction
|
|
|
Gall bladder mucosa
|
-Simple columnar epith w/ microvilli
-Lamina propria covered in fenestrated capillaries |
|
|
Gall blader muscularis mucosa & submucosa
|
There is no muscularis mucosa or submucosa in the gall bladder.
|
|
|
Gall bladder muscularis externa
|
-Very large w/o distinct layering
-Surrounded by very thick layer of DICT -Many vessels and nerves -adventitia where in contact w/ liver -Serosa on its free surface |
|
|
Rokitansky-Aschoff sinuses
|
-Sinus of epithelium extending into and past the muscularis externa
-May be pathologic in and of themselves or serve as reservoirs for bactreria, predisposing to chronic infection and bile stone formation. |
|
|
Gallstones
|
-cholesterol
-degraded Hb from spleen -combination of the two |
|
|
Pancreatic capsule
|
DICT septae that run into the gland; contains vessels and large ducts
|
|
|
Exocrine pancreas
|
Digestive hormones excreted into ducts and released into the duodenum; eosinophilic zymogen granules near the lumen:
-Proteolytic enzymes: cleave peptide bonds -Amylolytic enzymes: cleave sugar polymers -Lipases: cleave TGs to free FAs -Nucleolytic enzymes: cleave nucleic acids to mononucleotides |
|
|
Pancreatic islets (of Langerhans)
|
Synthesize endocrine hormones for metabolic regulation:
-A cells: (15-20%) Glucagon; islet periphery -B cells: (70%) Insulin; islet centers -D cells: (5-10%) Somatostatin; islet centers |
|
|
How is pancreatic secretion mediated?
|
-Endocrine: Enteroendocrine hormones from the duodenum
-Exocrine: Parasympathetic stimulation |
|
|
Centroacinar cells
|
-Flat squamous acinar cells at the base of intercalated ducts
-Add bicarb and water to pancreatic exocrine secretions which neutralize gastric acid and prevent premature activation of pancreatic enzymes |
|
|
How does the appearance of pancreatic duct cells change as they get further away from the acini?
|
they become taller
|
|
|
Pancreatitis
|
Early activation of pancreatic proenzymes due to inflammation or other factors causing autolysis. One cause is gall stone obstruction of the hepatopancreatic ampulla.
|
|
|
Follow the pathway exocrine pancreatic secretions follow from acinus to the duodenum.
|
Intercalated Ducts
(within acini) ↓ Intralobar ducts (collect secretions from acini in a pancreatic lobule) ↓ Interlobar Ducts (collect secretions from multiple lobes) ↓ Main Pancreatic Duct ↓ Hepatopancreatic Ampulla (main pancreatic duct + common bile duct) ↓ Duodenum |

