![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
Medication-related Immunodeficiency
|
– Mycobacterium tuberculosis
– Pneumocystis jiroveci – Aspergillus fumigatus – Strongyloides stercoralis – Listeria monocytogenes – Fusarium solani – Hepatitis B Virus – Babesia microti |
|
|
Asplenic patients
|
– Streptococcus pneumoniae
– Haemphilus influenzae – Neisseria meningitidis – Capnocytophaga canimorsus |
|
|
Transplant recipients
|
– Cryptococcus neoformans
– Cytomegalovirus – Varicella Zoster Virus – BK Virus – Toxoplasma gondii |
|
|
Neutropenia
|
– Pseudomonas aeruginosa
– Staphylococcus aureus – Staphylococcus epidermidis – Viridans Streptococci – Candida species – Trichosporon asahii – Scedosporium prolificans |
|
|
• Humoral immunodeficiency
• Cell-mediated immunodeficiency |
– Legionella pneumophila
– Coccidioides immitis – Histoplasma capsulatum – Cryptosporidium parvuum |
|
|
Medication-related Immunodeficiency
– Corticosteroids |
• Depletion of circulating T lymphocytes and monocytes
• Suppression of phagocyte migration and function • Long-term impaired skin and soft tissue healing • Infections: • All bacteria, particularly M. tuberculosis • Fungi: Pneumocystis jiroveci, Aspergillus, Fusarium • Strongyloides stercoralis |
|
|
TNF-α inhibitors
Medication-related Immunodeficiency |
• TB reactivation
• Listeria monocytogenes – increased susceptibility |
|
|
Rituximab (mAb to CD20)
Medication-related Immunodeficiency |
• HBV reactivation
• Babesia microti – increased susceptibility, high parasite burden, severe clinical manifestations (fever, anemia) |
|
|
Mycobacterium tuberculosis
• Bacteriology |

• Slim, acid fast intracellular rod
• Hydrophobic lipid surface • Mycolic acids • Lipoarabinomannan • Resistant o drying, common disinfectants, acid, alkali |
|
|
Mycobacterium tuberculosis
Epidemio |
• Inhalation of droplet nuclei containing microbe
• Humans may be infected via GI tract through milk from infected cow or through abraded skin • Less than 10 bacilli may initiate pulmonary infection in susceptible individual • Globally 1/3 of population is infected • 30 million with active disease |
|
|
Mycobacterium tuberculosis
Manifestations |
Primary tuberculosis
• Asymptomatic or only fever and malaise • Infiltrates in mid-zones of lung and enlarged draining lymph nodes in hilum • Lymph nodes fibrose and calcify • 5% merges into reactivation type of TB or may disseminate to organs • Reactivation tuberculosis • Reactivation of quiescent TB in individuals over 50 • Associated with immunosuppression • Cough is universal symptom – initially dry and sputum produced as disease progresses • Disease in other organs |
|
|
Mycobacterium tuberculosis
Primary tuberculosis |
• Asymptomatic or only fever and malaise
• Infiltrates in mid-zones of lung and enlarged draining lymph nodes in hilum • Lymph nodes fibrose and calcify • 5% merges into reactivation type of TB or may disseminate to organs |
|
|
Mycobacterium tuberculosis
Reactivation tuberculosis |
• Reactivation of quiescent TB in individuals over 50
• Associated with immunosuppression • Cough is universal symptom – initially dry and sputum produced as disease progresses • Disease in other organs |
|
|
Pneumocystis jiroveci
• Mycology 3 forms |
• Cystic structures within which elliptical subunits grow
• 3 forms • Trophic = founded by cell wall and cytoplasmic membrane that enclose a nucleus and mitochondria • Precyst = nuclei divide to form 8 spores • Cyst = contains spores • Spores = eccentric nucleus, nucleolus, single mitochondrion • No filamentous form |
|
|
Pneumocystis jiroveci
Epidemio |
• Occurs worldwide
• Specific antibodies in nearly all children by age of 4 • Reservoir and mode of transmission unknown • Low virulence in individuals with normal T cell function |
|
|
Pneumocystis jiroveci
Manifestations |
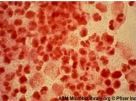
• Pneumonia characterized by alveoli filled with desquamated alveolar cells, monocytes, organisms, and fluid
• Distinct foamy, honeycombed appearance • Hyaline membranes may be present • Cardinal manifestations include progressive dyspnea and tachypnea with cyanosis and hypoxia supervening; non-productive cough (in contrast to TB) • Clinical signs of pneumonia usually absent despite infiltrates on x-ray |
|
|
Aspergillus fumigatus
• Mycology |
• Rapidly growing mold with branching septate hyphae and conidia on the conidiophore
doesnt grow as yeast in tissues |
|
|
Aspergillus fumigatus
Epidemio |
• Widely distributed in nature and found worldwide
• Inhalation mode of transmission • Disease is rare in immunocompetent |
|
|
Aspergillus fumigatus
Manifestations |
Clinical allergies or occasional invasive infection
• Allergic = transient pulmonary infiltrates, eosinophilia • Patients with asthma = bronchopulmonary tree with poor drainage as site for growth of organisms and continuous seeding of antigen • Invasive = mycelial masses form radiologically visible fungus ball within preexisting cavity • May have hemoptysis or erosion into other structures due to fistulas |
|
|
Strongyloides stercoralis
• Parasitology |
• Smallest intestinal nematode = 2mm
• Live in humans as larvae and parthenogenetic females • Infective larvae penetrate skin |
|
|
Strongyloides stercoralis
Manifestations |
• Intestinal infection usually symptomatic; may be pulmonary disease
• Heavy worm loads can present with peptic ulcer-like disease • Peripheral eosinophila • May be vomiting, diarrhea, paralytic ileus, and malabsorption • External autoinfection produces transient, raised, red, serpiginous lesions over buttocks and lower back |
|
|
Listeria monocytogenes
• Bacteriology |
• Gram-positive coccobacillus
• β-hemolytic colonies on blood agar • Catalase positive • Tumbling motility below 30°C • Widespread in animals and the environment • Can grow slowly at refrigeration temperatures |
|
|
Listeria monocytogenes
Pathogenesils |
• Internalin
• Listerolysin O (LLO) • Propels through cytosol via actin polymerization • Survival within macrophages |
|
|
Listeria monocytogenes
Manifestations |
• Associated with uncooked foods like pate, contaminated milk, soft cheeses, coleslaw
• Usually presents as meningitis • Populations at risk • Pregnant women • Immunocompromised individuals • Elderly individuals |
|
|
Fusarium solani
• Mycology |

• Filamentous fungus widely distributed on plants and in the soil
• Normal flora of rice, bean, soybean, and other crops |
|
|
Fusarium solani
Epididemio |
Infections difficult to treat and often fatal
|
|
|
Fusarium solani
Manifestations |
• Superficial and systemic infections in humans
• Disseminated infections in neutropenic and transplant patients |
|
|
Fusarium solani
Treatment |
Treatment
• Amphotericin B alone or in combination with flucytosine or rifampin |
|
|
Hepatitis B Virus
• Virology |
• Hepadnaviridae family
• Enveloped DNA virus • Partially ds with short, ss segment • Spherical virion • 4 major serotypes based on HBsAg • 8 genotypes: A-H with different clinical outcomes |
|
|
Hepatitis B Virus
-Chronic carriers |
• Chronic carriers
|
|
|
Hepatitis B Virus
Manifestations |
• Fever, fatigue, loss of appetite
• Vomiting, abdominal pain • Dark urine • Clay-colored bowel movements • Joint pain • Jaundice |
|
|
Babesia microti
• Parasitology |
• Intraerythrocytic parasite
• Incubation 1 week to 3 months (ave. 3 weeks) |
|
|
Babesia microti
epidemio |
• Northeastern US coasts
• Transmission via bite of Ixodes tick • Affects asplenic patients more severely • Often co-infection with Borrelia burgdorferi |
|
|
Babesia microti
manifestations |
• Influenza-like symptoms that progress to hepatosplenomegaly and hemolytic anemia
• May be thrombocytopenia and leukopenia |
|
|
Babesia microti
Dx |
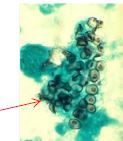
• Intraerythrocytic ring-shaped parasites on Giemsa-stained blood smears
• Maltese cross formation – tetrad of protozoa |
|
|
Babesia microti
Treatment |
• Clindamycin and quinine or atovaquone and azithromycin
• Transfusion may be necessary |
|

|
Babesia microti
|
|
|
Asplenic patients
|
– Due to trauma, malignancy, refractory idiopathic thrombotic purpura, and other hematologic disorders
– Sickle cell = functional asplenia – Severe, overwhelming bacterial infections with rapid onset and high mortality – Immediate treatment with antibiotics against encapsulated organisms – Blood cultures must be obtained – Infections • Streptococcus pneumoniae • Haemophilus influenzae • Neisseria meningitidis • Capnocytophaga canimorsus • Babesia microti |
|
|
Streptococcus pneumoniae
• Bacteriology |

• Gram-positive coccus; aerobic or anaerobic growth
|
|
|
Streptococcus pneumoniae
Epidemiology |
• ~5% of population carry in respiratory tract
• Transmission via respiratory droplets • ~20-30% mortality even if treated |
|
|
Streptococcus pneumoniae
Manifestations |
• Pneumonia, septicemia, and meningitis
• Meningitis in very young (<2 years), elderly, sickle cell disease, splenectomized patients, following head trauma • Clinical features more severe than with N. meningitidis and H. influenzae |
|
|
Streptococcus pneumoniae
Pathogenesis |
• Capsule is anti-phagocytic
• IgA protease CAPSULE IS PROBLEM FOR ASPLENICS |
|
|
Streptococcus pneumoniae
Dx/ Treatment |
• Diagnosis
• Gram stain of CSF and/or blood • Culture on blood agar; shows alpha-hemolysis (green zone around colonies) • Treatment • Heptavalent protein-conjugate vaccine • Vaccination at least 2 weeks prior to planned splenectomy • Vaccination 2 weeks after unplanned splenectomy |
|
|
Haemphilus influenzae
• Bacteriology/ Epidemio |
• Bacteriology
• Gram-negative coccobacillus; non-motile, facultative anaerobe • Epidemiology • Transmission via respiratory droplets |
|
|
Haemphilus influenzae
Manifestations |
• Meningitis in infants and young children (< 5 years of age)
• Also otitis media, sinusitis, and pneumonia • Serious sequelae including hearing loss, delayed language development, and mental retardation • ~5% mortality even if treated |
|
|
Haemphilus influenzae
Pathogenesis |
• 6 types (a-f) based on capsular polysaccharides
• Unencapsulated common and in throat of most healthy individuals • Type b in respiratory tract of infants and young children • Hib (type B) vaccine for children ≥ 2 years of age • Capsule is anti-phagocytic |
|
|
Haemphilus influenzae
Dx/treatment |
• Diagnosis
• Gram stain of CSF and/or blood • Culture on chocolate agar containing hematin (factor X) and NAD (factor V) • Direct detection of capsular antigen • Treatment • Vaccination at least 2 weeks prior to planned splenectomy • Vaccination 2 weeks after unplanned splenectomy |
|
|
Neisseria meningitidis
• Bacteriology/epidemio |
• Bacteriology
• Gram-negative diplococcus • Non-motile • Epidemiology • Asymptomatically carried by ~10-20% in nasopharynx • Transmission via respiratory droplets |
|
|
Neisseria meningitidis
Manifestations |
• Erythematous macules initially
• Petechiae and purpura • Extremities and trunk • Gun metal gray, hemorrhagic, necrotic patches • May develop into symmetrical peripheral gangrene |
|
|
Neisseria meningitidis
Pathogenesis |
• Antigenic polysaccharide capsule
• IgA protease • Pili • Endotoxin • Outer membrane proteins |
|
|
Neisseria meningitidis
dx/treatment |
• Diagnosis
• Gram stain of CSF and/or blood • Culture on Thayer-Martin or chocolate agar • Rapid latex agglutination test • DNA probe • Treatment • Vaccination at least 2 weeks prior to planned splenectomy • Vaccination 2 weeks after unplanned splenectomy |
|
|
Capnocytophaga canimorsus
• Bacteriology/epidemio |
Gram-negative of oropharynx of canines
Epidemiology • Dog bite inoculates bacteria |
|
|
Capnocytophaga canimorsus
Manifestations |
• Severe sepsis and rapid systemic infection in asplenic patients
• Digital necrosis |
|
|
Capnocytophaga canimorsus
Treatment |
Treatment
• Careful cleaning of dog bites • Prophylactic antibiotics after dog bites • Oral amoxicillin-clavulanic acid • Ampicillin-sulbactam, fluoroquinolones, or third-generation cephalosporins for IV therapy |
|
|
Transplant recipients
|
– Community-acquired, nocosomial, and reactivation infections
– Localize to the transplanted organ and surrounding tissues in SOT recipients – Potential opportunitistic pathogens prior to SCT – Early post-transplant period (2 and 6 months) • Opportunistic pathogens • Pneumocystis jiroveci • Aspergillus fumigatus • Cryptococcus neoformans • Reactivation of latent pathogens • Cytomegalovirus • Varicella zoster virus • BK virus • Toxoplasma gondii – >6 months post-transplant • Community-acquired pathogens, particularly encapsulated bacteria • Reactivation of latent viruses • Risk of transplant-associated malignancy due to latent viruses (Epstein-Barr virus and human papillomavirus) |
|
|
Cryptococcus neoformans
• Mycology/epidemio |
• Mycology
• Encapsulated yeast-like fungus • Epidemiology • Found in soil • Transmission via inhalation of air-borne cells |
|
|
Cryptococcus neoformans
Manifestations |
• Influenza-like disease or
pneumonia • Severe meningitis in immunocompromised patients |
|
|
Cytomegalovirus
• Virology |
β-herpesvirus subfamily
|
|
|
CMV
Manifestations |
• Infants
• 1% infants shed in urine or nasopharynx at delivery due to in utero infection • 90% normal or asymptomatic but long term 10-20% develop sensory hearing loss, psychomotor mental retardation, or both • Symptomatic illness = hepatosplenomegaly, jaundice, anemia, thrombocytopenia, low birth weight, microcephaly, chorioretinitis • Fetal damage most likely in 1st trimester • Neonatal infections during or shortly after birth • Rarely associated with adverse outcome • Can be transmission via breast milk • Childhood and adulthood • Usually asymptomatic • May cause mononucleosis syndrome • Immunocompromised = primary infection and reactivation is severe • Bone marrow transplants = interstitial pneumonia leading cause of death • AIDS patients = disseminates to visceral organs causing chorioretinitis, gastroenteritis, and neurologic disorders |
|
|
VZV
all |
• Virology
• Herpesviridae = enveloped dsDNA icosahedral virus • Epidemiology • Transmitted via respiratory droplets or vesicle fluid • Manifestations • HHV-3 = varicella (chickenpox) and zoster (shingles) • Pathogenesis • Axonal travel to latency sites in sensory ganglia |
|
|
– BK Virus
• Virology |
• Polyomavirus family
• Small double-stranded DNA virus with icosahedral capsid |
|
|
BK Virus
Manifesstations |
• Mild respiratory infection in immunocompetent
• Kidney transplant recipients • Ureteral stenosis and interstitial nephritis • Bone marrow transplant recipients • Hemorrhagic cystitis |
|
|
BK Virus
Pathogenesis |
Pathogenesis
• Virus to kidneys and UT - persists for the life • 80% of population - latent virus |
|
|
BK Virus
Dx/treatment |
• Diagnosis
• BKV blood test or PCR • Urine test for decoy cells • Biopsy of kidneys • Treatment • Reduction of immunosuppression • Leflunomide or cidofovir |
|
|
Toxoplasma gondii
• Parasitology |
• Obligate, intracellular protozoa
|
|
|
Toxoplasma gondii
Epidemiology |
• Consuming raw or undercooked, contaminated meat
• Ingesting water, soil, vegetables, or anything contaminated with feces of an infected animal (particularly cats) • Blood transfusion or organ transplant • Transplacental from mother to fetus during pregnancy |
|
|
Toxoplasma gondii
Manifestations |
• Mild, flu-like symptoms in healthy humans
• Associations with attention deficit hyperactivity disorder, obsessive compulsive disorder, and schizophrenia • Encephalitis and chorioretinitis in immunocompromised |
|
|
Neutropenia
|
Neutropenia
– After stem cell transplant or chemotherapy – Increased risk of infection < 100/μL – Infections • Gram-negative enteric organisms • Pseudomonas aeruginosa • Staphylococcus aureus • Staphylococcus epidermidis • Viridans streptococci • Candida species • Aspergillus fumigatus • Trichosporon asahii • Scedosporium prolificans • Fusarium solani |
|
|
Pseudomonas aeruginosa
|
Bacteriology
• Aerobic, Gram-negative bacillus • Polar flagella for motility • Epidemiology • Opportunistic pathogen – can cause infection in almost every body system • Major source of nosocomial infections • Carried as part of normal flora in gut of small number of individuals • Widespread in moist environments • Transmission via direct or indirect contact • Resistant to many antibiotics • Manifestations • Pneumonia in cystic fibrosis patients • Septic shock in neutropenic patients • UTI • Necrotizing enterocolitis in neutropenic cancer patients and premature infants • Skin/soft tissue infections |
|
|
– Staphylococcus aureus
|
• Bacteriology
• Gram-positive cocci that grow in clumps or groups • Non-motile • Facultative anaerobe • Catalase positive • Coagulase positive • Grows as golden, β-hemolytic colonies on blood agar • Epidemiology • Part of the normal flora of the nose, skin, vagina, axilla, perineum, and oropharynx • Manifestations • Skin and soft tissue infections • Osteomyelitis and septic arthritis •*** Infective carditis • ***Sepsis • ***Necrotizing pneumonia • Gastroenteritis |
|
|
Staphylococcus epidermidis
• Bacteriology/epidemio |
• Bacteriology
• Coagulase-negative gram-positive cocci in clusters • Epidemiology • Normal skin flora • Forms biofilms on catheters and indwelling devices |
|
|
Staphylococcus epidermidis
Manifestations |
• Prosthetic-associated infections
• Endocarditis • Sepsis in immunocompromised |
|
|
Viridans Streptococci
• Bacteriology/epidemio/manif |
• Bacteriology
• α-hemolytic gram-positive cocci in chains • S. viridans: S. mitis, S. mutans, S. oralis, S. sanguinis, S. sobrinus • Epidemiology • Commensal flora • Manifestations • Dental caries – S. mutans • Subacute endocarditis |
|
|
Candida species
|
• Mycology
• Budding, round or oval yeast • Cell wall of mannan, glucan, chitin ± protein • Epidemiology • Oropharyngeal, gastrointestinal, female genital flora • Common cause of nosocomial infections • Manifestations • Thrush • Denture stomatitis • Cellulitis • Esophagitis – AIDS-defining illness |
|
|
Trichosporon asahii
• Mycology/epidemio |

• Mycology
• Anamorphic yeast • Epidemiology • Isolated from soil • May be normal flora of skin of humans and animals • Mortality = 42% |
|
|
Trichosporon asahii
manifestations/treatment |
• Manifestations
• White piedra – soft, pale (immunocompetent) nodules on hairs of scalp and body • Invasive infection - progresses rapidly, involving the lungs, kidneys, and spleen (immunocompromised) • Fungemia • Benign funguria in renal transplant recipients • Treatment • High-dose amphotericin B deoxycholate • Voriconazole, posaconazole, ravuconazole |
|
|
Scedosporium prolificans
Mycology/epidemio |

• Mycology
• Filamentous fungus found in soil of houseplants • Epidemiology • Resistant to most antifungals |
|
|
Scedosporium prolificans
Manifestations |
• Immunocompetent – localized skin lesions with bone and joint involvement
• Disseminated disease secondary to myeloblastic leukemia and following lung transplant • Pneumonia, meningoencephalitis, and endocarditis |
|
|
Scedosporium prolificans
Pathogenesis |
• Subcutaneous lesions from injury following "traumatic implantation" by contaminated splinters or plant thorns
|
|
|
Scedosporium prolificans
Treatment |
• Combination of voriconazole and terbinafine
• Resistant strains - posaconazole, miltefosine and albaconazole |
|
|
Humoral immunodeficiency
|
– Congenital immunodeficiencies
– Multiple myeloma, chronic lymphocytic leukemia, and asplenic patients – At risk for infection with encapsulated organisms • Haemophilus influenzae • Neisseria meningitidis • Streptococcus pneumoniae |
|
|
Cell-mediated immunodeficiency
|
– HIV/AIDS patients
– Hodgkin disease – Immunosuppressive medications – Solid organ transplant patients – Chemotherapy – Infections with intracellular microorganisms • Listeria monocytogenes • Legionella pneumophila • Mycobacterium tuberculosis • HSV • VZV • CMV • Cryptococcus neoformans • Coccidioides immitis • Histoplasma capsulatum • Pneumocystis jiroveci • Toxoplasma gondii • Crytposporidium parvuum |
|
|
Legionella pneumophila
• Bacteriology |

• Thin, pleomorphic, Gram-negative bacillus
• Facultative intracellular pathogen • Polar, subpolar, and lateral flagella • LPS less toxic than other Gram-negative bacteria |
|
|
Legionella pneumophila
Epidemiology |
Epidemiology
|
|
|
Legionella pneumophila
Manifestations |
Necrotizing multifocal pneumonia
|
|
|
Coccidioides immitis
• Mycology |

• Dimorphic fungus
• No yeast phase • Large round-walled spherule = tissue invasive form • Uninucleate endospores within spherule • Arthroconidia = barrel-shaped septate hyphae with thick wall; highly infectious |
|
|
Coccidioides immitis
Epidemiology |
• Grow in harsh conditions in environment like sandy alkaline soil with high salinity
• Endemic in areas with hot, dry summers and mild winters with few freezes • Throughout Central and South America • Arizona, Nevada, New Mexico, western Texas, parts of California • Not transmissible from person to person |
|
|
Coccidioides immitis
Manifestations |
• < 50% infected have no symptoms or very mild disease
• Others develop malaise, chest pain, fever, arthralgia • Small number of cases progress to chronic pulmonary form characterized by cavity formation and a slow relapsing course over years |
|
|
Histoplasma capsulatum
• Mycology |

• Dimorphic fungus that grows as a yeast in tissue
• Thick wall and radial, finger-like projections |
|
|
Histoplasma capsulatum
Epidemio |
• Grows in soil under humid conditions, particularly soil containing bird or bat droppings
• Inhalation of microconidia reach terminal brochioles and alveoli • Endemic on all continents except Antarctica • >50% of residents of endemic areas show radiologic evidence of previous infection |
|
|
Histoplasma capsulatum
Manifestations |
• Infection of lymph nodes, spleen, bone marrow, and reticuloendothelial system
• Most infections are asymptommatic or only show fever and cough for a few days • Mediastinal lymphadenopathy and slight pulmonary infiltrates seen on x-ray • More severe cases = chills, malaise, chest pain • Progressive pulmonary disease similar to that of pulmonary TB • Disseminated disease = CNS, skin, GI tract, and adrenal glands may be involved in addition to ulcers on mucosal surfaces |
|
|
Cryptosporidium parvuum
|

• Parasitology
• Protozoan parasite • Epidemiology • Self-limiting in healthy • Severe and chronic, even fatal in immunocompromised • Manifestations • Incubation 2-10 days • Stomach cramps or pain • Dehydration • Nausea, vomiting, and diarrhea • Fever • Weight loss |

