![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
What is the function of the MHC? |
1. Display peptide fragments for recognition by antigen-specific T cells |
|
|
What are the classes of MHC? |
1. I 2. II 3. III |
|
|
Where are class I MHC molecules present? |
1. All nucleated cells |
|
|
What encodes for MHC I? |
1. HLA-A 2. HLA-B 3. HLA-C |
|
|
What is the structure of MHC I? |
1. Heavy a-chain linked to B2-microglobulin |
|
|
To what do MHC I molecules present? |
1. CD8 cells |
|
|
Where are MHC II found? |
1. Only on antigen-presenting cells |
|
|
What encodes for MHC II? |
1. HLA-DP 2. HLA-DQ 3. HLA-DR |
|
|
What is the structure of MHC II? |
1. a-chain 2. B-chain |
|
|
To what does MHC II present? |
1. CD4 cells |
|
|
How are HLA genes linked together? |
1. Haplotype on chromosome 6 2. Inherited en bloc |
|
|
What is responsible for tissue compatibility between donor and recipient? |
1. MHC molecules |
|
|
What is cellular rejection? |
1. T cell mediated graft rejection 2. Destruction by CD8 cells 3. Type IV HSR triggered by CD4 cells |
|
|
What do T cells recognize in direct cellular rejection? |
1. MHC molecules on APCs in the graft 2. CD8 cells destroy |
|
|
What do T cells recognize in indirect cellular rejection? |
1. MHC antigens of graft donor after they are presented by recipient's own APCs 2. CD4 cells enter graft and recognize antigens |
|
|
What are the classifications of renal graft rejection? |
1. Hyperacute 2. Acute 3. Chronic |
|
|
What are the characteristics of hyperacute rejection? |
1. Ab mediated 2. Abs present in blood of recipient 3. May have arisen from prior transfusion, pregnancies, or previous transplants |
|
|
What is the consequence of a hyperacute rejection? |
1. Irreversible 2. Graft must be removed
|
|
|
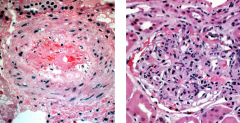
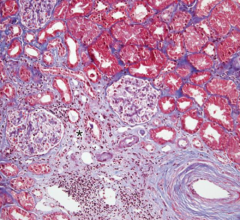
What is the histopathology of hyperacute rejection? |
1. Complement and Ig are deposited in vessel wall, causing endothelial injury and thrombi in renal vessels 2. Variable infiltrate of leukocytes in glomeruli, peritubular capillaries, and interstitium |
|
|
1. Hyperacute rejection |
|
|
In what patients does acute rejection occur? |
1. Recipients not previous sensitized to transplantation antigens 2. Exposure to donor HLA antigens may provoke production of Abs which initially target graft vasculature |
|
|
What are the possible mediators of acute rejection? |
1. Ab (humoral) 2. T cell (cellular) |
|
|
When can acute rejection occur? What are the signs of acute rejection? |
1. Anytime 2. Most often seen in first few months 3. Ssx: Abrupt onset of decreasing urine output and increasing BUN/creatinine |
|
|
What is the reversibility of acute rejection? |
1. Possibly reversible with appropriate immunosuppressive tx |
|
|
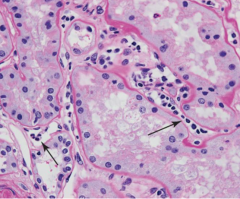
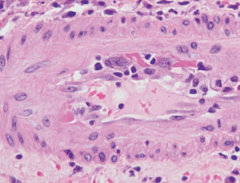
What is the histopathology of acute humoral rejection? |
1. Damage to blood vessels--- 2. Necrotizing vasculitis 3. Necrosis of renal parenchyma |
|
|
Acute rejection capillaritis |
|
|
Acute rejection vasculitis |
|
|
When does chronic rejection occur? |
1. Several years after transplantation 2. Several episodes of acute rejection 3. MC after initial 6-12 mos. |
|
|
What is the reversibility of chronic rejection? |
1. Irreversible |
|
|
What is the presentation of chronic rejection? |
1. Progressive renal failure 2. Rise in serum creatinine over 4-6 mos. |
|
|
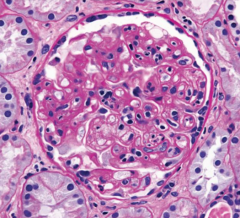
What is the histopathology of chronic rejection? |
1. Vascular changes 2. Interstitial fibrosis 3. Tubular atrophy 4. Glomerular scarring |
|
|
Chronic rejection |
|
|
Chronic rejection |
|
|
What is graft v. host disease? |
1. Immunocompetent lymphocytes engrafted in bone marrow or liver may reject tissues of recipient |
|
|
Where does GVH disease usually occur? |
1. Skin 2. GI tract 3. Liver |
|
|
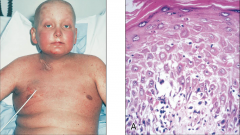
What are the ssx of acute and chronic GVHD? |
1. Acute-- rash, diarrhea, abdominal cramps, anemia, liver dysfunction 2. Chronic-- dermal sclerosis, dry eyes and mouth (Sicca), immunodeficiency |
|
|
1. GVHD |
|
|
How do you increase graft survival? |
1. HLA-match donor and patient 2. Screen donor for preformed antibodies 3. Immunosuppressive tx 4. Pretreatment of graft with antithymocyte globulin |
|
|
What are the reasons for HLA testing? |
1. Pre-transplantation workup-- find a close match 2. Determine risk of certain diseases--- HLA-related diseases |
|
|
What should you do in pre-transplant testing? |
1. ABO and Rh 2. HLA recipient and donor lymphocytes 3. Look for pre-formed Abs 4. Test recipient's serum against donor's lymphocytes |
|
|
What organs do not require HLA testing? |
1. Heart 2. Lung 3. Liver 4. Pancreas 5. DO CHECK FOR ABO |
|
|
Corneal transplant. What's the deal? |
1. MC transplant 2. Don't need to test HLA or ABO 3. MC lost graft |

