![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
What is bone remodelling?
(inc average rates) |
• Coordinated osteoclastic resorption and osteoblastic
proliferation • Maintains skeletal structure • Annual rate of turnover Cortical - 4% Trabecular - 25% |
|
|
What are the six steps of the Bone Metabolic Unit as the basis of bone remodelling?
|
1.Activation: Osteoclasts
2.Resorption: Bone matrix 3.Reversal: pre-osteoblasts 4.Formation: osteoid formation 5.Mineralization: 6.Quiescence |
|
|
How do bone grow?
|
•Endochondral ossification - longitudinal
•Subperiosteal apposition - width •At the same time endosteal bone resorption – medullary cavity expansion |
|
|
When does bone growth/remodelling stop and on what does it depend?
|
It goes on throughout life and its rate depends upon
•Growth •Hormones and growth/biochemical factors •Mechanical stress ••During growth -- turnover high, formation> resorption so net bone gain ••During adulthood -- turnover moderate, formation< resorption so net bone loss |
|
|
What is the chemical composition of bone?
|
2/3 Inorganic - calcium hydroxyapatite
1/3 Organic - •Type 1 collage (tensile) •Proteoglycans (compressile) •Osteocalcin – bone proteins •Cytokines/IL |
|
|
What is woven bone?
|
- Collagen fibres and cells – no specific arrangement
- Weak - Temporary - Forms on fibrous tissue –Immature –Healing |
|
|
What is lamellar bone?
|
•Collagen fibres - parallel
•Osteocytes - in between and organised - It is laid only on existing bone surface Two forms –Cortical –Cancellous/trabecular – less mass, but more surface area |
|
|
What are the main bone cells?
|
Osteoblast : bone formation
At the end of bone remodelling cycle they remain as resting osteocytes. Osteocyte : dormant; sensitive to stimuli and communicate to osteoblasts Osteoclast : bone resorption. Derived from monocyte precursors in marrow |
|
|
What are the age-related changes in bone mass?
|
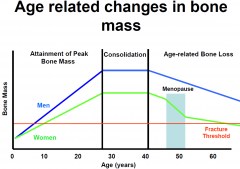
•Puberty onwards 2-3% increase in bone mass upto peak 30yrs.
•Steady till about 35-40 •Then bone loss 0.3-0.5%/yr •After menopause in women : rapid bone loss 2-3% per yr for the next 8-10 yrs (mainly trabecular) •>60 rate of loss slows down to 0.5%/yr |
|
|
What main molecular factors determine bone turnover?
|
•Calcium & Phosphates
•Parathyroid hormone (PTH). •Cholecalciferol and Calcitriol (Vit.D3). •Estrogen and other Sex hormones. •? Calcitonin. |
|
|
What other factor affect bone turnover?
|
•Local factors
•Insulin-Like Growth Factor I (somatomedin C) –increased osteoblast proliferation,regulated by growth hormone •TGF –increased osteoblast activity, accounts for coupling and resorption •IL-1/Osteoclast Activating Factor –increases osteoclast activity •PG’s –increased bone turnover (in fractures & inflammn) –Causes hypercalcaemia in metastatic bone disease •BMP –bone formation |
|
|
What are bone metabolic diseases?
|
Abnormalities of formation ( bone morphology )
and Metabolism of bone ( functions ) |
|
|
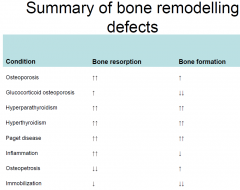
What is the pathology of the major diseases of bone?
|
Loss of MineralizationLoss Mineralization : osteomalacia/ricketsosteomalacia/rickets
Low bone mass: osteoporosis,Osteogenesis Imperfecta High bone mass: osteopetrosis High bone turnover: pagets, hyperparathyroidism, thyrotoxicosis ••Low bone turnover: adynamic disease, hypophosphatasia |
|
|
How are potential bone metabolism diseases assessed?
|
•History
–duration –drug Rx –aetiological associations •Exam: Features of underlying endocrine disorder - moon face(hypercortisonism), - hairless skin(testicular atrophy) , - physical underdevelopment (rickets) •X-rays - plain and specialist • - shows loss of horizontal trabeculae in osteoporosis • - stress fractures (prox tibia and femur), compression fractures in vertbrae. •Bone density (DEXA) •Biochemical tests •Rarely bone biopsy |
|
|
What biochemical tests are used?
|
•Serum Ca/PO43- (rarely ionised calcium)
•Alkaline phosphatase (bone turnover) •PTH •Vit. D activity (measured by 25-HCC ) •Specific endocrine test •Markers of bone turnover •FGF-23 |
|
|
What is osteomalacia/rickets?
3 points |
osteomalacia (adults)/rickets (children)
Poorly mineralised osteoid Severe/long standing Vitamin D deficiency Reduced availability of calcium and phosphate |
|
|
What is osteoporosis?
|
•Reduced total bone mass
•Adequate mineralisation of present osteoid •Many factors (inc Oestrogen deficiency) •Relatively increased bone resorption |
|
|
What is Paget's disease?
|
•Rapid bone turnover
•Both bone resorption and formation are increased •Disorganised structure •Reduced bone strength •Risk of fracture •Linked to osteosarcoma tumour suppressor gene |
|
|
What is corticosteroid-induced osteoporosis?
4 points |
•Increased osteoclastic activity
•Decreased osteoblastic activity •Impaired collagen formation •Increased bone turnover and poor bone formation and healing |
|
|
What is osteopetrosis?
|
•‘Failure’ of remodelling – decreased turnover
•Unregulated osteoblastic activity, though not necessarily increased •Impaired osteoclastic activity •Dense but weak bones |
|
|
What is Fluorosis?
|
Defective mineralisation
Fluoride replaces calcium in the matrix |
|
|
What is Primary hyperparathyroidism?
|
•Unregulated PTH secretion
•Hypercalcaemia (low phosphate) •Markedly increased bone turnover •May retain bone mass, but in elderly or other risk factors, often osteoporosis |
|
|
More about rickets
|
•Rickets
–Nutritional rickets –Congenital rickets –Rickets of prematurity –Genetic rickets –Neoplastic rickets –Hypophosphataemic rickets –Drug-induced rickets •Renal causes - Renal osteodystrophy, Fanconi syndrome •Tumor-induced osteomalacia •Other causes –Hypophosphatasia –McCune-Albright syndrome –Osteogenesis imperfecta with mineralization defect (syndrome resembling osteogenesis imperfecta) |
|
|
What is renal rickets(osteodystrophy)?
|
•High Phosphate – only type of rickets
•Combines with Ca – hypocalcaemia •Excess phosphate excreted into gut –combines with Ca in gut •2° hyperPTH •Aluminium excess – dialysis •Types - Adynamic (30%; ↓osteoblastic activity) - Hyperdynamic (↑bone turnover). |
|
|
What is Osteogenesis imperfecta?
|
•Genetic bone disorder
•Defect/deficiency Collagen I •Various types – different severities •Recurrent childhood fractures •Deformities •Ligamentous laxity; low muscle tone •Bluish sclerae |

