![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Metabolic and Toxic Encephalopathy |
Generalized dysfunction of cerebral neurons associated with changes in the brains normal environment caused by metabolic or toxic factors. |
|
|
Clinical signs |
Alteration of consciousness (mild to deep coma) No obvious focal abnormalities. Pupils are usually small and reactive May see myoclonus May have seizures May see asterixis |
|
|
Asterixis |
Tremor of the hand when the wrist is extended Abnormal function of the diencephalic motor centers of the brain, which regulate the muscles involved in maintains posture |
|
|
Asterixis AKA |
Liver flap (but also seen with other metabolic encephalopathy) |
|
|
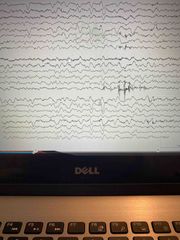
EEG with metabolic and Toxic encephalopathy |
Typically non-focal changes Background slowing Increased theta Polymorphic delta FIRDA most sever cases may have burst suppression and ECI without recovery Triphasic Generalized periodic discharges Epileptiform activity Excessive beta |
|
|
Are focal disturbances possible with metabolic and toxic encephalopathy |
If there is a tumor or stroke May see unilateral delta May have asymmetrical alpha or unilateral voltage suppression Structural lesion must be ruled out |
|
|
Hepatic encephalopathy |
Disease of the liver |
|
|
Causes of hepatic encephalopathy |
Alcohol, chronic hepatitis, nonalcoholic fatty liver disease. Iron buildup in body, cystic fibrosis, hardening and scarring of the bile ducts. Liver is unable to break down toxins Build up of toxins in the brain cause encephalopathy Watch for high ammonia lab results |
|
|
Clinical cues of hepatic encephalopathy |
Jaundice Asterixis |
|
|
EEG with hepatic encephalopathy |
With grade 1 coma, eeg May be normal or have diffuse nonspecific slowing Triphasics are seen in level 3 coma Often frontal dominance |
|
? |
Hepatic encephalopathy more likely to have triphasics |
|
|
Reye’s syndrome |
Seen in children-advised not to use aspirin Often after viral illness, flu, or chicken pox Severe hepatic dysfunction (high ammonia) Hypoglycemia Swelling of liver and brain Confusion, seizures, coma- life threatening of not recognized and treated |
|
|
EEG with Reye’s syndrome |
Slowing, mild to severe, burst suppression Multifocal or focal epileptiform activity |
|
|
Uremic encephalopathy |
Disease of the kidneys Chronic renal disease, end stage renal failure, kidney infection, trauma Kidneys are unable to remove toxins from the blood Watch for high creatinine or high blood urea nitrogen (BUN) lab results Pt May have nausea, lethargy in early stages Later delirium, seizures, myoclonus, asterixis, coma |
|
|
EEG Uremic Encephalopathy |
Disorganization and background slowing Increased theta/delta Paroxysmal and intermittent bursts of semi-rhythmic slow waves Exaggerated arousal response may be seen, bursts of slow waves Triphasics seen in 20% of cases, mostly atypical triphasics-less rhythmic, more irregular Bursts of spike and wave Photo paroxysm is or photomyogenic response |
|

? |
Uremic more likely to have seizures |
|
|
Dialysis Disequilibrium syndrome |
Osmotic disequilibrium, change in electrolytes causes cerebral edema Happens right away after or during dialysis |
|
|
EEG with Dialysis Disequilibrium Syndrome |
Increased slowing Paroxysmal abnormalities Increased photo sensitivity Exaggerated visual evoked response |
|

? |
Encephalopathy following dialysis |
|
|
Earliest change with hypoglycemia |
Exaggerated HV buildup (can be seen in normal person while fasting) |
|
|
EEG- Hypoglycemia |
More slowing with lower glucose levels Intermittent bursts of bisynchronous slow waves Generalized delta in grade II coma May accentuate preexisting epileptiform abnormalities - especially 3Hz spike/wave in absence |
|
|
Hyperglycemia in uncomplicated diabetes, EEG is usually |
Normal or shows mild non-specific irregularities |
|
|
2 other types of Hyperglycemia |
Diabetic ketoacidosis Non ketotic hyperosmolar hyperglycemia |
|
|
Diabetic Ketoacidosis |
Seen most in type 1 diabetes when difficult to control, may also in other types High blood sugar, muscles break down fat stores for energy and release ketones Seizures are not common |
|
|
EEG with Diabetic Ketoacidosis |
Slowing is seen, worsening along with mental status change |
|
|
Nonketotic Hyperosmolar Hyperglycemia AKA |
Diabetic Hyperosmolar syndrome |
|
|
Nonketotic Hyperosmolar Hyperglycemia |
Elevated blood sugar without Ketosis or acidosis Leads to coma - life threatening |
|
|
EEG in Nonketotic Hyperosmolar Hyperglycemia |
Nonspecific EEG changes May have focal seizures or epilepsia Partialis continua with focal EEG abnormalities- often related to underlying focal cortical lesion (usually vascular) activated by the imbalance A lot more seizure related and can be a lot more dangerous |
|
|
Electrolyte disorders Sodium disorders: hyponatremia |
Not enough sodium in the blood Can cause confusion, seizures, coma Generalized slow background Polymorphic delta Bisynchronous slow waves on slow background |
|
|
Dialysis encephalopathy syndrome AKA |
Dialysis dementia |
|
|
Electrolyte disorders Sodium disorders: Hypernatremia |
Too much sodium in the blood Can cause confusion, muscle twitching, focal or generalized seizures, coma Vascular occlusion or hemorrhage May be a complication especially in infants and children |
|
|
Dialysis Encephalopathy syndrome |
Progressive dementia, speech disturbance, apraxia while on dialysis treatment |
|
|
Dialysis Encephalopathy syndrome within months... |
Asterixis, myoclonus, seizures, psychosis Often fatal Aluminum toxicity- seen less due to aluminum free water bath with dialysis |
|
|
Dialysis Encephalopathy syndrome- EEG |
Diffuse slowing Frontally dominate high amplitude slow waves Triphasics, sharp waves, or slow spike/wave |
|
|
Dialysis Encephalopathy syndrome EEGs recorded shortly after dialysis may show... |
More prominent abnormalities and eeg changes may be seen before clinical changes |
|
|
Glucose metabolism |
Encephalopathy from hypoglycemia or hyperglycemia in blood sugar levels |
|
|
Glucose Metabolism EEG |
Slowing May have generalized or focal seizures |
|
|
Glucose metabolism is seen with... |
Poorly controlled diabetes, illness or trauma, alcohol or drug use |
|
|
Who is prone to Hypoglycemia |
Diabetics who take insulin or oral agents |
|
|
3 types of Calcium metabolism |
Hypocalcemia in infants Hypocalcemia in older children and adults Hypercalcemia |
|
|
Other Metabolism disorders: Pyridoxine Deficiency |
Vitamin B6 deficiency |
|
|
Other Metabolism disorders: Porphyria |
Porphyrins build up, can affect skin, CNS, bone marrow, or liver |
|
|
Other Metabolism disorders: Pernicious Anemia |
Vitamin B12 deficiency |
|
|
Other Metabolism disorders: Wilson’s disease |
Copper accumulated in liver |
|
|
Hypsarrhythmia May be seen with |
Pyridoxine deficiency. Others have normal to mild nonspecific slowing |
|
|
Drug Toxicity: Therapeutic levels |
Increased beta with benzodiazepines and coke Mild background slowing possible with carbamazepine, gabapentin and some neuropsychotic drugs (lithium, Tricyclics antidepressant) |
|
|
Toxic levels with barbiturates |
Beta coma or spindle coma (10-16 Hz max frontals) superimposed on delta Burst suppression or generalized suppression |
|
|
Toxic levels with other medications |
Slowing Paroxysmal activity Triphasics (Baclofen) LPD Status Epilepticus (penicillin, carbon monoxide) |
|
|
Hypocalcemia in infants |
Most common known cause of neonatal seizures Focal seizures Focal, multifocal, shifting EEG abnormalities |
|
|
Hypocalcemia (non-infant) |
Diffuse background slowing Paroxysmal bursts of high amplitude slow waves Accentuated slowing with HV Prominent photic response May have photoparoxysmal response Paroxysmal epileptiform abnormalities Abnormalities resolve with return of normal calcium levels |
|
|
Hypercalcemia |
Diffuse background slowing Intermittent and semi-rhythmic slowing - enhanced with HV Prominent photic responses Changes may be related to associated electrolyte changes, renal derangement, complicating factors |
|
|
Thyroid disease Congenital Hypothyroidism (infants) |
Background slowing Decreased voltage Poor reactivity Delay in pattern development- sleep spindles |
|
|
Thyroid disease Hypothyroidism (older kids/adults) |
Low voltage theta background |
|
|
Thyroid disease Hyperthyroidism |
Increased alpha, accentuated beta Toxic levels: generalized theta and delta |
|
|
Hashimoto’s Encephalopathy |
Autoimmune associated with thyroiditis Acute or mostly subacute encephalopathy, seizures, myoclonus, stroke like episodes, psychiatric disturbance |
|
|
Hashimoto’s Encephalopathy EEG |
Generalized slowing or FIRDA May have epileptiform activity or triphasics May have photoparoxysmic or photomyogenic response RARE |
|
|
Other Metabolism disorders: Aminoacidemias |
PKU |

