![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
What is the histological difference between a normal pituitary gland and a pituitary adenoma? |
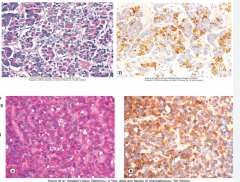
Normal gland - fine capillary network, GH fairly abundant
Adenoma - fairly uniform small cells, less reticulin, stains strongly for GH |
|
|
What proportion of hyperthyroid cases are Grave's? |
85% |
|
|
What is the histological appearance of Grave's? |
Taller folliculocytes with larger nuclei. Colloid scalloping - increased use of stored colloid. Smaller follicles because less colloid. Folliculocytes form papillae. |
|
|
What are the different types of adrenal disorders? |

|
|
|
What are the capillaries in the anterior pituitary? |
Sinusoidal + fine supported network collagen and reticular fibres, cords of CT & BM> |
|
|
What are 3 components of the pituitary stalk? |
Pituicytes - glial cell of posterior pituitary Hypothalamohypophyseal tract, portal vessels |
|
|
What cells are present in the parathyroid hormone? |
Chief cells - produce PTH - act on bones, kidneys, and GI Oxyphil cells - function unknown |
|
|
What is the histological arrangement of zona glomerulosa cells, zona fasiculata cells and zona reticularis cells? |
Glomerulosa - rounded clumps Fasiculata - parallel cords Reticularis - irregular cords |
|
|
What is the blood supply to the adrenal medulla? N.b. chromaffin cells |
DUAL blood supply - arterioles from capsule, and arterioles from cortex that have come from capsular arteries, these are rich in adrenocorticosteroids which also stimulate catechol release. |
|
|
What proportion of the pancreas is A, B, D and PP cells? |
A = 20% B = 70% D= 5-10% PP= 1-2% |
|
|
What lies between the clusters and cords of adrenal cortical cells? |
A fine supporting network of connective tissue {condensed areas of pink material (H&E) or green/brown material (Masson's) between cords} and sinusoidal capillaries |
|
|
Why do many reticularis cells have a foamy unstained appearance? |
TAG main substrate for steroid synthesis, form lipid droplets in cyto. Removed during processing leaving holes. |
|
|
Why does Cushing's produce hypertension? |
Cortisol is a weak mineralocorticoid Aldosterone is a mineralocorticoid |
|
|
What is the difference in deiodination between T4 -> T3 and T4 -> rT3? |
T4 -> T3 via 5 deiodination T4 -> rT3 (inactive) via 3 deiodination |
|
|
What antibodies are likely to be found in the serum of a Hashimoto's patient? |
Anti TPO/Tg/microsomal Abs Defects can occur in: - iodine transport and uptake - dehalogenation - iodotyrosine coupling |
|
|
What is seen in primary bilairy cirrhosis? |
Chronic inflammatory disease centred on bile ducts. Infiltration of walls via lympho, macro, plasma. Formation of granulomas near bile ducts. 90-95% have antimitochondrial antibodies. |
|
|
What is a consequence of primary biliary cirrhosis? |
Portal tract expansion by chronic inflammatory cells, -> interface hepatitis, ultimately fibrosis + proliferation small bile ductules. |
|
|
What is the function of stellate cells? |
Produce ECM Act as capillary pericytes, regulating intralobular flow and hepatic regeneration. |
|
|
What 3 things activate stellate cells to become myofibroblasts? |
1. Chronic inflammation - factors from Kuppfer cells and lymphocyte 2. Cytokines and chemokines from Kuppfer cells, endothelial cells, ductal epithelium, hepatocytes due to ECM disruption 3. Toxins acting directly on stellate cells |
|
|
What are the main classifications of cirrhosis and the causes for both? |
a) micronodular i.e. nodules <3mm caused by alcoholic liver disease b) macronodular i.e. >3mm caused by complication HCC |

