![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
Name the syndrome: Multiple basal cells, odontogenic keratocysts, palmar and plantar pits, calcification of falx cerebri, bifid ribs, hypertelorism, broad nasal root. |
Nevoid basal cell syndrome (Gorlin's syndrome)1, 11 ▸Autosomal dominant inheritance pattern on chromosome 9q22.3–q31 |
|
|
Which skin lesion present at birth has a 10-15% risk of malignant degeneration to BCC? |
Nevus sebaceus of Jadassohn ▸Present at birth on scalp or face ▸Well-circumscribed, hairless, yellowish plaque that becomes verrucous and nodular at puberty ▸10%–15% malignant degeneration to BCC |
|
|
Most common type of basal cell carcinoma? |
Nodular •Most common histologic type: 50%–60% •Well-defined borders, flesh-colored, pearly nodule with overlying telangiectasias •May be ulcerated: Central ulcer surrounded by rolled border; historically called rodent ulcer |
|
|
Which type of basal cell is most aggressive? Three different names for it? |
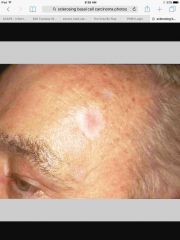
Morpheaform (sclerosing or fibrosing) •2%–3% of BCCs, most aggressive •Typically described by patients as an “enlarging scar” without history of trauma •Usually an indurated, flat, or slightly elevated papule or plaque with white to yellow scarlike appearance •Rarely ulcerates •High incidence of positive margins after excision |
|
|
Basal cell carcinoma margins: How much for small primary lesions on the face or other low risk? How much for higher risk tumors on the trunk/extremities? |
▸Current literature recommends 4 mm margin for small primary BCC on face or other low-risk lesions. ▸10 mm margins are recommended for primary resection of high-risk larger tumors on trunk or extremities. |
|
|
Bowen's disease of the glans penis, vulva, or oral mucosa; malignant transformation in 30%. What is this called? |
Erythroplasia of Queyrat |
|
|
▸Smooth dome-shaped mass of squamous cells and keratin grows rapidly over 1–6 weeks and ulcerate with central crusting. ▸Once stabilized, tumors spontaneously regress over 2–12 months and heal with scarring. ▸ resembles SCC histologically. ▸Larger or atypical lesions should be treated as SCC. What does this describe? |

Keratoacanthoma |
|
|
Squamous cell metastasis: Where do local mets go? How are distant mets spread? 5 most common places of metastasis? Risk of metastasis for trunk vs face/extremity? |
▀Local metastasis occurs to regional nodal basins. ▀Distant metastasis occurs by hematogenous dissemination most commonly to the lungs, liver, brain, skin, or bone. ▀Metastasis from primary: •2%–5% on trunk •10%–20% on face/extremity |
|
|
Which depth & thickness of SCC convey increased risk of death? |
Tumors that penetrate dermis or are thicker than 8 mm are associated with high risk for death. |
|
|
Wide local excision of SCC: Margin needed for lesions <2cm, grade 1, low risk? Margin needed for >2cm, grade 1-3, high risk? |
▸Generally 4–6 mm margins are recommended. ♦Smaller than 2 cm, grade 1, low-risk region, depth to dermis: >4 mm margins ♦Larger than 2 cm, grade 2, 3, or 4, high-risk region, depth to subcutaneous fat: >6 mm margins |
|
|
Does Mohs or wide local excision have higher recurrence rate in SCC? |
Five-year recurrence rates for primary cutaneous SCC with Mohs 3.1% (versus 8.1% for surgical excision, and 10% for RT) |
|
|
Lifetime risk of congenital nevus becoming melanoma? |
Congenital nevus: 6% lifetime risk depending on size |
|
|
Pigmented lesions > X mm in diameter are more likely to be malignant than benign. |
Pigmented lesions >5-10 mm in diameter are more likely to be malignant than benign. |
|
|
Name the lesion: Juvenile melanoma of children and young adults •Smooth surface, dome shaped, red or pink |

Spitz nevus •Juvenile melanoma of children and young adults •Smooth surface, dome shaped, red or pink •Telangiectasias typically are present •Most common on head and neck •Typically less than 6 mm in diameter •Often noticed after rapid change in size or color •Proliferation of enlarged spindled/epithelioid melanocytes |
|
|
Melanoma resection margins: How much for 1 mm thick? How much for 3 mm thick? |
▸<1 mm: 1 cm margin ▸1–4 mm: 2 cm margin ▸<4 mm: 2 cm margin |
|
|
Melanoma SLN indications: Which stages? If ulcerated or with >1 mitotic figure, which thickness? Cut off thickness where everyone gets a SLN biopsy? |
Indications ♦Stage IB melanoma or stage II ♦0.76–1 mm thick with ulceration or mitotic rate ≥1 per mm2, or more than 1.0 mm thick ♦In transit stage III if resectable |
|
|
A 48-year-old right-hand–dominant man is referred for treatment of a biopsy-proven subungual malignant melanoma in situ of the right thumb. Which of the following is the most appropriate treatment? A) Amputation to the interphalangeal joint with no reconstruction B) Amputation to the metacarpophalangeal joint with toe-to-thumb transfer C) Chemotherapy D) Radiation therapy E) Wide local excision with split-thickness skin grafting
|
The correct response is Option E. While the literature lacks randomized control data, there is mounting evidence that melanoma in situ can be appropriately treated with wide local excision alone. This is associated with considerably less morbidity than amputation with or without reconstruction. |
|
|
What size margin for lentigo maligna? |
Surgical resection remains the standard of care for treatment of lentigo maligna. In 1992, the National Institutes of Health Consensus Conference on Melanoma recommended a 5-mm margin for excision of lentigo maligna. However, the use of 5-mm margins has been associated with recurrence rates of 8 to 20%. In 2008, the National Cancer Comprehensive Network released guidelines indicating that 5-mm margins may be inadequate for treatment of lentigo maligna. The use of a staged excision technique has shown that 10-mm margins or greater were required in a majority of patients and resulted in low (1.7%) recurrence rates at 2 years. |
|
|
An otherwise healthy 65-year-old man comes to the clinic because of a 3-cm ulcerated lesion of the scalp. There are no palpable regional lymph nodes. Chest x-ray study shows no abnormalities. A punch biopsy is performed and a diagnosis of well-differentiated squamous cell carcinoma is made. Wide local excision of the lesion is planned. Which of the following is the recommended minimum surgical margin in this patient? A) 1 mm B) 2 mm C) 4 mm D) 6 mm E) 12 mm
|
The correct response is Option D. Cutaneous squamous cell carcinoma (cSCC) is the second most common skin cancer after basal cell carcinomas. They are broadly categorized into low- and high-risk lesions depending on size, location, depth of invasion, recurrence, and patient factors such as immunosuppression. A 4-mm margin of healthy tissue is recommended for lower-risk lesions. This category includes well-differentiated tumors smaller than 2 cm in diameter that do not occur on the scalp, ears, eyelids, lips, or nose, and do not involve subcutaneous fat. Therefore, simple excision is most valuable in the treatment of small primary squamous cell carcinomas on the trunk, extremities, or neck, where tissue sparing is less essential. The recurrence rate after the excision of low-risk lesions ranges from 5 to 8%.
A 6-mm margin of healthy tissue is recommended for lesions that are larger than 2 cm, invasive to fat, or in high-risk locations (i.e., central face, ears, scalp, genitalia, hands, feet). Given the cosmetic and functional impact of these wider margins, tumors in this latter category are often removed via Mohs micrographic surgery to achieve high cure rates while sparing healthy tissue. The depth of an excision should always include a portion of the subcutaneous fat. |
|
|
Key treatment for angiosarcoma? |
Angiosarcoma is a rare (2% of all soft-tissue sarcomas) but highly aggressive tumor that is most commonly found in the face and scalp in older Caucasian men. Fifty percent of all cutaneous angiosarcomas are found in the head and neck, and they are also commonly found in the breast and extremities, particularly in patients with a history of lymphedema or radiation therapy. It appears initially as a purple plaque which is often confused with a bruise or cellulitis, which can delay diagnosis. It is frequently multifocal, and local recurrences are common, so wide local excision is recommended, frequently combined with radiation therapy. Preoperative serial punch biopsies of the surrounding tissue can help in determining appropriate resection margins. The tumor can microscopically infiltrate normal tissues for some distance away from the obvious tumor, so wide local excision is necessary. |
|
|
A 39-year-old woman is evaluated because of a 6-month history of a growth on the face. A biopsy is planned. Which of the following findings on pathology can be safely treated with observation only in this patient? A) Cylindroma B) Eccrine poroma C) Nevus sebaceous D) Trichoepithelioma |
The correct response is Option D.
Trichoepitheliomas are neoplasms of follicular differentiation. Trichoepithelioma usually presents as multiple, yellowish-pink, translucent papules distributed symmetrically on the cheeks, eyelids, and nasolabial area. The lesions are more frequently seen in women. Lesions are benign but can be confused with basal cell carcinomas clinically and histologically. As they are benign, no further measures should be taken. However, in cases of desmoplastic trichoepithelioma, complete excision or Mohs surgery may be needed to clearly differentiate this entity from a carcinoma. |
|
|
A 47-year-old man comes to the office because of an asymptomatic lesion of the anterior abdominal wall that has been enlarging gradually for the past 10 years. The lesion has accelerated in growth during the past several months and recently ulcerated. Examination shows a 6-cm, raised, indurated, and irregularly shaped violaceous plaque consisting of firm, irregular nodules. Examination of a specimen obtained on incisional biopsy shows a soft-tissue malignancy arising from mesenchymal cells in the dermis. What is this lesion? What is the most appropriate treatment? |
The diagnosis of the described lesion is dermatofibrosarcoma protuberans (DFSP). It accounts for less than 0.1% of all malignant neoplasms and approximately 1% of all soft-tissue sarcomas, but is the most common type of cutaneous sarcoma. It is a malignant mesenchymal tumor that arises in the dermis and is characterized by latency in its initial detection, slow infiltrative growth, and local recurrence if not adequately treated. Distant metastasis is rare and generally occurs as a late sequela after repeated local recurrences. DFSP is most commonly found on the trunk followed by the proximal extremities, and rarely in the head and neck. These tumors have irregular shapes, frequent finger-like extensions, and an infiltrating growth pattern extending beyond clinical margins that result in incomplete removal and a propensity for local recurrence. Treatment primarily consists of wide surgical excision to include margins of 2 to 3 cm beyond the clinical tumor border if possible. Mohs micrographic surgery has been used with good outcomes in aesthetically sensitive areas such as the head and neck where tissue sparing is important. Reconstruction with tissue rearrangement or flaps should be performed after negative margins are confirmed. Most recurrences occur within 3 years of the primary excision, and close follow-up is indicated. |
|
|
A recent meta-analysis of the literature concluded that for basal cell carcinomas 2 cm or less, a X mm margin is sufficient to achieve at least a 95% chance of cure. A surgical margin difference of 1 mm can mean the difference in flap requirements, aesthetic outcome, and in some cases, functionality of the affected area. |
A recent meta-analysis of the literature concluded that for basal cell carcinomas 2 cm or less, a 3-mm margin is sufficient to achieve at least a 95% chance of cure. A surgical margin difference of 1 mm can mean the difference in flap requirements, aesthetic outcome, and in some cases, functionality of the affected area. |
|
|
A 38-year-old woman has severe hidradenitis suppurativa of the groin and axillae. Which of the dermal appendages are located in these areas and implicated in the disease process? |
Apocrine glands |
|
|
Which skin lesion dimples when pinched from the side? |

Dermatofibroma |
|
|
40-year-old, right-hand-dominant man comes to the office because of a 2-mm pigmented lesion beneath the thumbnail of the left hand. He says that he first noticed the lesion within the last week. The patient recalls no trauma to the thumb. He has no other fingernails or toenails with similar streaking. Biopsy of a subungual lesion is most appropriate after which period of time has passed without change? |
4-6 weeks |
|
|
After thickness, ____ is the most important prognostic indicator for melanoma, and has become an important component of T staging. |
After thickness, ulceration is the most important prognostic indicator for melanoma, and has become an important component of T staging. |
|
|
Subungual melanoma risk factors: width of band? What is it called when there’s extension onto the skin? |
Characteristics that are concerning for subungual melanoma are: age 50 to 70, longitudinal band greater than 3 mm or irregular border, change of lesion size or coloration, extension onto periungual skin (Hutchinson sign), personal or family history of melanoma, and single finger involvement. |

