![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is another term for prevalence? |
Pre test probability or probability of disease before the test is known |
|
|
|
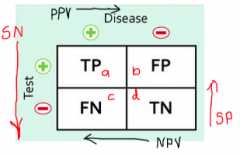
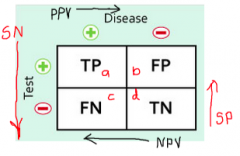
how to calculate PPV (Positive predictive value)? |
a/a+b |
|
|
|
How to calculate specificity with a 2x2 table |
d/d+b How good is the test at detecting the absence of disease in someone who doesn't have the disease. |
|
|
|
How to calculate sensitivity with a 2x2 |
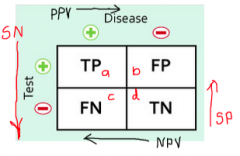
A/a+c |
|
|
|
What are the two things that PPV (Positive predictive value) is determined by? |
1. The accuracy of the test (specificity and sensitivity) 2. The prevalence |
|
|
|
Define incidence? |
The proportion of a population that didn't initially have the illness but develop it in the time studied. |
|
|
|
Likely hood ratios: define LR+? |
LR(+) = Sn / (1-Sp) LR(-) = (1-Sn) / Sp |
|
|
|
When assessing the validity of a study what are the three items? R A M |
Is the population Representative? (Or if comparing were the groups comparable?)
Is there adequate Ascertainment/followup? Were the measures objective, unbiased, and relevant?
|
|
|
|
What does a cross sectional study measure? |
Prevalence of disease |
|
|
|
SN-N-OUT |
A SeNsitive test, when Negative, rules the illness out |
|
|
|
SP-P-IN |
A specific test, when positive, rules the illness in |
|
|
|
If you have a Sensitive test and the result is negative, what does that mean? |
SN-N-OUT A sensitive test, when negative, rules the disease OUT |
|
|
|
What are three important biases that can impact the internal validity of a study? |
1. Selection bias 2. Measurement bias 3. Confounding bias |
|
|
|
What values are most important when INTERPRETING a test? |
PPV (Positive Predictive Value) NPP (Negative Predictive Value) |
|
|
|
8 Cognitive elements of stress. 3L 2P 2E S |
1. Limitations 2. Letting go and acceptance 3. Listening
4. Presence of mind 5. Perceptions
6. Emotions 7. Expanding self interest
8. Self discipline 9. Sleep
|
|
|
|
Define "therapeutic index" |
Lethal dose 50 / (over) effective dose 50 |
|
|
|
What is a screening test? |
-Application of a test to an a-symptomatic population -To detect disease at a stage when treatment is more effective -Used to identify people who require further investigation -Is not primarily a diagnostic test. |
|
|
|
What makes a good screening test? |
1. the condition should be an important health problem 2.There should be a recognisable latent or early symptomatic stage 3. the natural history of the condition, including development from latent to declared disease, should be adequately understood 4. there should be an accepted treatment for patients with recognised disease 5. there should be a suitable test or examination that has a high level of accuracy 6. the test should be acceptable to the population 7. there should be an agreed policy on whom to treat as patients 8. facilities for diagnosis and treatment should be available 9. the cost of screening (including diagnosis and treatment of patients diagnosed) should be economically balanced in relation to possible expenditure on medical care as a whole, and 10. screening should be a continuing process and not a ‘once and for all’ project |
|
|
|
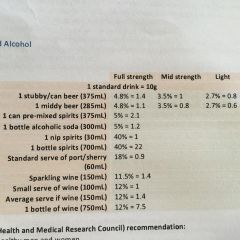
What are the recommended maximums for alcohol consumption? |
-Average 2 standard drinks per day (14 per week) -No more than 4 in one session -Same for males & females - 0 when pregnant |
|
|
|
What are the 6 aspects of a medical professional CanMeds - CACMSP What are the elements of the medical expert as defined by CanMeds? |
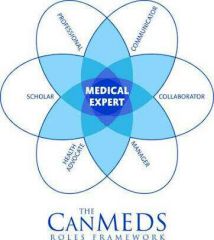
Communication Collaboration Scolar/learner Health advocate Manager Professional-boundaries |
|
|
|
How much alcohol is in a standard drink? |
10 grams of alcohol in a standard drink. |
|
|
|
List 6 of the social determinants of health |
Education Employment Housing Culture Social cohesion, inclusion Political stability/instability Income Transport Access to Services |
|
|
|
Wilkinson & Marmot's studies demonstrated a CVD morbidity among Whitehall civil servants, - morbidity rates highest with lowest self-reported job control. Practical significance of finding? |
A sense of control over one's life is a major determinant of health outcome. So interventions aimed at improving health need to reduce the inequalities between privileged & not-so-privileged groups by providing people with the knowledge, skills and a supportive environment (physical and social) to have more control over their lives, not just address biological factors. |
|
|
|
Clinical placement in a small rural hospital. A 66 year old admitted with community-acquired pneumonia. Sputum sample is taken but results won't be available for days. How would you find what is the best antibiotic? |
1. Formulate the clinical question. - Search terms - include community-acquired pneumonia & Australia & therapy 2. Decide what source Journals or databases OR is there an evidence-based clinical guideline available to this context? Refer to latest version of Australian 'Therapeutic Guidelines: antibiotic' |
|
|
|
Why is it important for doctors & health professionals to pay attention to the illness, as well as the pathophysiological disease process? |
We should be treating people as whole, not body parts. |
|
|
|
List three indicators of health status in which there is a significant difference between urban & rural/remote Australians. |
Higher: total mortality rate, mortality from cardiovascular, & chronic obstructive pulmonary diseases, mortality from motor vehicle accidents, other injuries, cancer, suicide. Higher hospital separation rates for people from very rural/remote areas. |
|
|
|
List 5 reasons contributing to inequalities in health status between urban & rural/remote area Australians |
Lower income Higher unemployment Reduced education opportunities Poorer access to services e.g. communications, transport, recreation & health services Poorer access to healthy foods |
|
|
|
What is social capital? |
Putnam defines it as "features of social organisation such as networks, norms & social trust that facilitates coordination and cooperation for mutual benefit". Bourdieu defines it as "the aggregate of the actual or potential resources which are linked to possession of durable network of more or less institutionalised relationships of mutual acquaintance and recognition. Examples GP teaching medical students or volunteering |
|
|
|
Not every parent wants to vaccinate their children. Outline some of the reasons why this might be so. |
Fear of side effects Complacency Toxic ingredients in vaccines-prefer natural Unconvinced of efficacy Convenience |
|
|
|
What approach can the GP take to facilitate effective communication with parents who have concerns about vaccinations? |
Ask permission to discuss Aim to keep discussion brief but leaving the door open Check importance of vaccines and confidence Don’t dismiss concerns – acknowledge Don’t overstate vaccine safety Provide links to resources if wanted Explore receptivity to a tailored schedule to get them started – explain the risks Offer another appointment when ready |
|
|
|
How might a doctor utilise resources to support vaccine discussions? |
Online decision aids, such as the MMR decision aid tool Fact sheets: such as those available from better health or vaccination handbook Disease surveillance data to aknowledge risks |
|
|
|
Current vaccination schedule |
Birth - Hep B 2 months - Hep B, DTPa, Hib (haemophilus influenza) Inactivated poliomyelitis, Rotavirus 4 months 6 months 12 months - MMR 18 months - MMR 4 years - MMR Ongoing & school programs (HPV etc) |
|
|
|
Impact of colonisation re: racism |
Incidents like Pinjarra massacre & repeated dispute & denial about history - continued racism 1905 Act In WA, particularly bad history of racism Continuum of racism WHO - social determinants of health - Poverty is the greatest threat to health |
|
|
|
What are the steps in Reflective Practice? |
Description - of the event Reaction - feel/do Connect - current/past experience, prior K Extension/Integration - what do you need to learn & how Contemplation |
|
|
|
Categorise qualitative vs quantitative research? |
Qualitative Descriptive & exploratory, narrative reporting, analysis of unstructured info Quantitative Hypothesis driven, statistical reporting, used to ID association &/or causation |
|
|
|
Randomised Controlled Trials |
Experimental study - investigator assigns exposures Random allocation to groups Active attempt to change a factor & alter the progress of disease. |
|
|
|
Cohort Study |
Observational study Testing a hypothesis - analytical Select the exposed vs nonexposed (control) group Follow up prospectively to watch & compare for development of disease (can be retrospective) |
|
|
|
Case-control study |
Observational study Testing a hypothesis - analytical Sampling based on OUTCOME Select cases with disease vs without disease Compare the exposure rate Retrospective Outcome: Odds ratio or risk ratio e.g. breast cancer vs not --> exposures |
|
|
|
Cross-sectional study/ Prevalence |
Observational study Testing a hypothesis - analytical Snapshot of how much disease is present @ a particular point in time Can be done using surveys Good for measuring prevalence e.g. census |
|
|
|
Descriptive study |
Observational study Not testing a hypothesis Used to determine existing patterns of disease - person, time & place DON'T ID causation - correlations Includes: case studies, case series, ecological, & cross-sectional |
|
|
|
Ecological study |
Correlates characteristics of entire population with a measure of disease Can't link exposure with disease Easy & cheap |
|
|
|
Case Series/Reports |
Describes experience of patient/group with the same disease Useful in quality improvement Often retrospectively |
|
|
|
Analytical studies |
Look more critically for causal effects Assess associations between exposure & outcome E.g. case-control & cohort |
|
|
|
Ottawa Charter Principle |
1. Build Public health policy - appropriate footwear 2. Create supportive environments - safe surfaces 3. Strengthen community action - advocacy 4. Develop personal skills - education 5. Reorient health services - Health Dept funding |
|
|
|
How do you identify the objective of a study? PICO question |
P - patient, problem, or population I - intervention C - comparison, control or comparator O - outcomes (resolution of disease or outcome of treatment) |
|
|
|
What are the factors to consider when critically appraising quantitative research? |
The validity of study design - are the results true? What is the impact - size of the benefit? Applicability to my patient population |
|
|
|
What are confounding factors? |
Characteristics of a patient population - might provide an alternative explanation for the results. |
|
|
|
What is prevalence? |
Estimate of the probability or risk an individual will have the disease at a specific point in time. SNAPSHOT. No time units. Prevalence = # of cases of disease at a given time / total population. |
|
|
|
What is incidence? |
The numbers of individuals who develop a specific disease or experience a specific health-related event during a particular time period (such as a month or year). Incidence rate = number of new cases of disease / a given period of time. Total person time at risk of disease in given time period |
|
|
|
What is cumulative incidence? |
Estimate of the probability or risk an individual will develop a disease during a specified period of time. Pre-defined person time element CI Rate = # of new cases of disease over a given period of time Total population at risk of disease in the given time period |
|
|
|
Standard drinks table |
|
|
|
|
Relative Risk (RR) |
Ratio of the risk (incidence) of disease/outcome in those exposed compared to the risk of disease in those not exposed. RR>1 = exposure increases likelihood of outcome |
|
|
|
Relative Difference (RD) |
The additional risk of disease following exposure, over & above that experience by people not exposed. RD = Incidence (exposed) - Incidence (unexposed) |
|
|
|
5 steps of EBM |
1. Formulate a PICO question 2. Get the best evidence 3. Critically appraise the evidence for validity (sample size, research methods), impact & applicability 4. Integrate with clinical expertise & patient values 5. Evaluate our effectiveness & efficient - keep a record & improve the process |
|
|
|
What is sarcopenia? |
Age related loss of muscle mass i.e. non-pathological. |
|
|
|
What is zerostonia? |
Lack of salivation Greater than 70% of the elderly |
|

