![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
341 Cards in this Set
- Front
- Back
|
Increased BUN
-causes |
Increased Production
-high protein diet -upper GI hemorrhage Decreased Excretion -Prerenal (dehydration, dec. CO) -Renal (renal failure, neoplasia) -Postrenal |
|
|
Decreased BUN
-causes |
Decreased production
-liver dysfunction (fibrosis, PSS) -low protein diet Increased excretion -high tubular flow rate |
|
|
Increased Creatinine
-causes |
Decreased excretion
-prerenal -renal -postrenal |
|
|
Decreased Creatinine
-causes |
Decreased production
-loss of muscle mass |
|
|
Hypersthenuric USG
-dog |
>1.030
|
|
|
Hypersthenuric USG
-cat |
>1.035
|
|
|
Prerenal azotemia
-causes |
-dehydration
-dec. Cardiac output -clot/thrombus in renal artery |
|
|
Hyposthenuria USG
|
<1.008
|
|
|
Isosthenuria USG
|
1.008 - 1.012
|
|
|
Normal USG
|
1.012 - 1.029 (dog)
1.012 - 1.034 (cat) |
|
|
AKI
-history |
Ischemia (depleted ATP --> Na/K pump failure ---> swelling ---> death)
-hypotension -hypovolemia -prolonged anesthesia -heat stroke -DIC Toxicant (damage to active epithelium) -ethylene glycol -amphotericin -aminoglycosides -NSAIDs Others: Lepto, Lyme, hypercalcemia, immune-mediated |
|
|
CKD
history |
-long history of renal disease
-PU/PD -Weight loss -Poor BCS |
|
|
AKI
-physical exam |
-swollen kidneys
-good body flesh -relatively sever clinical signs for the level of dysfunction (depression, anorexia, vomiting, diarrhea, dehydration) -uremic breath -normal echogenicity |
|
|
CKD
-physical exam |
-small irregular kidneys
-weight loss -relatively mild clinical signs for the level of dysfunction -echogenetic cortices -loss of C/M junction |
|
|
A 10-year-old neutered male mixed breed dog is presented with an acute onset of vomiting that began 4 days ago. On physical examination the dog is 6-8% dehydrated and has dry mucous membranes. There is no dysuria/stranguria or hematuria observed during voiding. You collect blood and urine before any treatment and laboratory evaluation reveals:
• Hematocrit - 38 % (37 - 62) • Total protein - 6.8 g/dl (5.3 - 7.4) • BUN - 38 mg/dl (6 - 28) • Creatinine - 2.2 mg/dl (0.8 - 1.9) • Sodium - 146 mEq/L (140 - 152) • Potassium - 3.0 mEq/L (3.3 - 4.6) • Total CO2 - 24 mEq/L (18 - 32) • Urine specific gravity - 1.038 Which one of the following is the most useful for localizing azotemia in this dog? presence of dehydration magnitude of azotemia severity of acidosis urine specific gravity sodium/potassium rat |
-Urine specific gravity
|
|
|
A high serum urea nitrogen to serum creatinine ratio could be caused by:
-prerenal dehydration -high dietary protein -upper GI hemorrhage -decreased muscle mass -all of the above |
-decreased muscle mass
|
|
|
How to prove prerenal azotemia?
|
-correct dehydration and remeasure
|
|
|
A 10 year-old, SF, terrier-cross is presented to you with a history of vomiting and diarrhea. She is 6% dehydrated with mild to moderate azotemia (BUN = 48 mg/dl, serum creatinine = 2.4 mg/dl), and a urine specific gravity of 1.021. There is no dysuria/stranguria or hematuria observed during voiding. What is the best interpretation?
-Pre-renal azotemia due to the dehydration -Pre-renal azotemia because the urine is concentrated -Renal azotemia because the urine is hypersthenuric -Renal azotemia due to inappropriate urine concentration given the dehydration and azotemia -Post-renal azotemia due to urethral obstruction |
-Renal azotemia due to inappropriate urine concentration given the dehydration and azotemia
|
|
|
AKI
-clin path |
-normal to increased hematocrit
-hyperkalemia -more severe metabolic acidosis -active sediment in urine |
|
|
CKD
-clin path |
-nonregenerative anemia
-normal to mild metabolic acidosis -inactive sediment in urine |
|
|
Renal failure
-define |
-a state of decreased renal function that allows persistent abnormalities (renal azotemia and the inability to concentrate urine) to exist
|
|
|
Renal failure occurs when
|
-loss of > 75% nephrons
|
|
|
Factors that make AKI potentially reversible
|
-nephron repair (if tubular basement membrane is intact and viable epithelial cells are present)
-compensatory hypertrophy *Treat to help buy time for repair and compensation |
|
|
Risk factors that may predispose a dog or cat to AKI
*Potentially correctable |
*Dehydration*
*Hypokalemia* (vomiting/dehydration) *Excessive dose/duration of drugs* *adverse drug combinations* (furosemide with nephrotoxicants) *prior use of aminoglycosides* *anesthesia* *Fever* -sepsis -old age -stage 1/early stage 2 CKD -liver disease -cardiac disease -neoplasia |
|
|
Most adverse risk factor for AKI
|
-dehydration
|
|
|
What would you look for on physical examination or urinalysis that could suggest early renal damage?
|
-dehydration, cardiac output
Urinalysis: -granular casts -renal epithelial cells -cellular debris -normoglycemic glucosuria -tubular proteinuria -enzymuria |
|
|
Using urine production to diagnose AKI
|
-should be > 2mL/kg/hr
|
|
|
Enzymuria
-use in early detection of AKI |
indication of renal tubular leakage or necrosis because most serum enzymes are not filtered through the glomerulus
-look at trough concentrations of aminoglycosides -NAG -GGT -Urine NAG:Creatinine or GGT:Creatinine reflect 24 hr GGT & NAG excretion in dogs if determined before azotemia onzet -determine in all dogs before the use of nephrotoxic drugs -2x-3x increase suggestive of renal tubular disease |
|
|
AKI
-goal of treatment |
buy time for compensation and repair
-eliminate renal hemodynamic disorders and alleviate water and solute imbalances -inc. urine production does not equal improved GFR |
|
|
AKI
-treatment |
-discontinue all potentially nephrotoxic drugs (consider measures to decrease drug absorption)
-start specific antidotal therapy if applicable -Identify and treat any prerenal or postrenal abnormalities -start IV fluid therapy -assess voume of urine production -correct acid-base and electrolyte abnormalities (R/O hypercalcemia neuropathy) -Diuretics to increase urinary volume if necessary (dec. BUN, phosphorus, potassium; dec overhydration ---> pulmonary edema from oliguria/anuria) -Consider peritoneal dialysis |
|
|
AKI
-why should dopamine not be used as a diuretic |
-unpredictable effect on renal blood flow and GFR
|
|
|
AKI
-response to treatment |
-dec. serum creatinine
-inc. urine production |
|
|
AKI
-prognosis |
Biopsy kidney after 3 days
-look for intect basement membranes and viable epithelial cells Prognosis depends on: -severity of dysfunction -response to treatment -ability to control GI signs -renal histology |
|
|
Ethylene glycol ingestion
-early clinical signs |
-ataxia and CNS deficits
-Vomiting -PU/PD -metabolic acidosis with increased anion gap -hyperosmolality with an increased osmolal gap -increased conc. of ethylene glycol in serum and urine -calcium oxalate crystalluria (intermediate sign) -azotemia (late sign) |
|
|
3 Stages of Ethylene glycol toxicity
|
1) CNS (good prognosis)
2) cardiopulmonary 3)renal systems (grave prognosis) |
|
|
Ethylene Glycol Ingestion
-treatment |
Ethanol or Fomepizole
-compete with ethylene glycol for alcohol dehydrogenase -without alcohol dehydrogenase, ethylene glycol can't break down into its toxic metabolites (glycolate, oxalate) |
|
|
Ethylene glycol ingestion
-difference between treating dogs and cats |
-Dogs: within 24 hrs of ingestion
-Cats: within 12 hrs of ingestion (use a higher dose aka fomepizole) |
|
|
Why are the functional alterations associated with CKD irreversible?
|
-irreversible damage to any portion of the nephron renders the entire nephron nonfunctional with healing occurring by replacement fibrosis`
|
|
|
CKD
-goals of treatment |
-identify and treat primary disease process
-slow down the progressive nature of the disease -alleviate patient symptoms |
|
|
Why do patients with renal failure often have GI issues?
|
-buildup of waste products (uremic toxins)
-gastric acidosis (gastrin buildup ---> mucosal irritation/ulceration) |
|
|
Drugs to deal with the GI effects of kidney disease
|
-Metaclopramide
-sucralfate -famotidine |
|
|
CKD
-common cause in dogs |
-glomerular disease
|
|
|
CKD
-likely cause in cats |
-tubulointerstitial disease
|
|
|
CKD
-causes |
Immunologic
-glomerulonephritis -SLE -amyloidosis Tubulointerstitial inflammatory disease -pyelonephritis -renoliths -lepto Chronic hypertension neoplasia congenital conditions -hypoplasia/dysplasia -polycystic kidney disease |
|
|
CKD
-recommendations for dietary protein |
Reduce dietary protein
-decrease quantity increase quality *decreased need for renal clearance of urea and other nitrogenous metabolites |
|
|
CKD
-recommendations for dietary sodium |
Decrease Sodium intake
*first line of defense against hypertension |
|
|
CKD
-recommendations for dietary phosphorus |
-restrict phosphorus intake
*due to decreased renal excretion and increased loss in calcium ----> increased PTH |
|
|
CKD
-recommendations for enteric phosphate binders |
if phosphorus levels remain after implementation of low high for 3-4 wks add binders
|
|
|
CKD
-cause of potassium depletion in cats |
-anorexia
-high protein diet -acidifying diet -PU/PD -vomiting |
|
|
CKD
-clinical signs of potassium depletion in cats |
-generalized muscle weakness
*95% of total body potassium is located within skeletal muscle |
|
|
CKD
-treatment of potassium depletion in cats |
-oral potassium supplement
(typically resolves in 5 days) |
|
|
What factors contribute to anorexia, nausea, and vomiting that frequently occur in patients with CKD?
|
Decreased GFR leads to increased plasma concentrations of uremic toxins (Uremic syndrome) ---> decreased caloric intake --->
1) stimulation of the CRTZ by uremic toxins 2) decreased excretion of gastrin and increased gastric acid secretion 3) GI irritation secondary to uremia |
|
|
Treatment for nausea and vomiting due to uremic syndrom
|
-metoclopramide
|
|
|
CKD
-factors contributing to non-regenerative anemia |
Hormonal disturbances
-decreased production of Epo and calcitriol -decreased RBC survival -GI tract blood loss -uremic toxins such as PTH on erythropoiesis -decreased B vitamins and folic acid |
|
|
CKD
-treatment for non-regenerative anemia |
-exogenous Epo (human recombinant)
|
|
|
How often would you recommend rechecking a CKD patient?
|
depends on the severity of dysfunction
-Stage 1: 6-12 month -Stage 2: 3-6 months (cats) 2-4 months (dogs) -Stage 3: 2-4 months |
|
|
CKD patient check-up
-what parameters should be looked at? |
-Urine protein creatinine ratio (urinalysis)
-azotemia (serum biochem) -electrolyte imbalances -blood pressure |
|
|
How do ACE inhibitors help to decrease the progressive nature of CKD?
|
Renoprotective
-normalize systemic and intraglomerular blood pressures -reduce proteinuria Decrease hypertension |
|
|
ACE inhibitor
|
Benazepril
|
|
|
How does CKD cause hypertension?
|
-decreased GFR activates RAAS
-Renin-angiotensinogen ----> vasoconstriction ---> hypertension |
|
|
Enzyme that converts ang-1 to ang-2
|
-Angiotensin Converting Enzyme
|
|
|
How to treat hypertension associated with CKD in dogs
|
-ACE inhibitor
|
|
|
How to treat hypertension associated with CKD in cats?
|
-Ca channel blocker
-ACE inhibitor |
|
|
CKD
-why supplement vitamin D3 |
-damaged kidneys ---> dec. Vit D3 production ---> supplement to absorb calcium
|
|
|
If a dog or cat is not eating due to CKD what can be done to make sure they receive the necessary caloric requirements?
|
-gastrostomy
-esophagostomy *IF NOT VOMITING |
|
|
CKD
-stages (general) |
-Stage I: non-azotemic CKD
-Stage 2: mild renal azotemia -Stage 3: moderate renal azotemia -Stage 4: severe renal azotemia |
|
|
UP:C
-normal |
-<0.2
|
|
|
UP:C
-Borderline |
> 0.2
|
|
|
UP:C
-glomerular or tubular proteinuria |
>0.4/0.5
|
|
|
UP:C
-glomerular range proteinuria |
>2..0
|
|
|
CKD
-immunologic causes |
-glomerulonephritis
-SLE -amyloidosis |
|
|
CKD
-tubulointersitial inflammatory diseases |
--pyelonephritis
-renoliths -lepto |
|
|
CKD
-overall treatment |
-discontinue potentially nephrotoxic drugs
-identify and treat any prerenal or postrenal abnormalities -R/O treatable conditions (pyelonephritis, renal urolithiasis) -Measure BP -Initiate dietary therapy -Treat vomiting/gastroenteritis -Treat anemia -Provide caloric requirements |
|
|
Polydipsia
-plasma osmolality |
-low osmolality
>80 mL/kg/24hrs *increased thirst ---> increased water consumption |
|
|
Polyuria
-plasma osmolality |
-increased osmolality
>50 mL/kg/24hrs *increased urine production and volume |
|
|
Normal fluid maintenance
|
-60 mL/kg/24hrs
|
|
|
Thirst
-stimulated by |
-increased plasma osmolality
-non-osmotic factors (hypotension, hyperthermia, pain, some drugs) |
|
|
Urine concentration requirements
|
1) adequate ADH
2) responsiveness of kidneys to ADH (> 1/3 total nephron number (exception in cats), hypertonic renal medullary interstitium) |
|
|
ADH release is influenced by:
|
-plasma osmolality
|
|
|
Diagnosis of PU/PD
|
-Primary Polydipsia
-Primary Polyuria |
|
|
Primary polydipsia
-how to diagnose |
-hypersthenuric response to the water deprivation test
|
|
|
Primary polyuria
-how to diagnose |
-no hypersthenuric response to the water deprivation test
|
|
|
Primary polyuria
-aka |
-diabetes insipidus
|
|
|
Primary polydipsia
-types |
-psychogenic (idiopathic) polydipsia
-portosystemic polydipsia |
|
|
Psychogenic polydipsia
-commonly occurs where? |
-in puppies
|
|
|
Primary Polyuria
-primary rule outs |
-Central diabetes insipidus
-Nephrogenic diabetes insipidus |
|
|
Differentiation of Central DI and Nephrogenic DI
|
Central = hypersthenuria with exogenous ADH
Nephrogenic = no hypersthenuria with exogenous ADH |
|
|
Possible causes of Central DI
|
-tumor
-trauma -etc |
|
|
Possible causes of Nephrogenic DI
|
-renal insufficiency/failure
-hyperadrenocorticism -hypoadrenocorticism -pyometra -hypercalcemia -hypokalemia -drugs (diuretics, corticosteroids) -liver disease -renal medullary solute washout -diabetes mellitus |
|
|
Renal insufficiency/failure
-mechanism for nephrogenic DI |
-not enough nephrons to respond to ADH or to maintain medullary hypertonicity
|
|
|
Hyperadrenocorticism (Cushings)
-mechanism for nephrogenic DI |
-cortisol inhibition of ADH binding
-possible inhibition of the posterior pituitary |
|
|
Hypoadrenocorticism (Addisons)
-mechanism for nephrogenic DI |
-possible hypercalcemia
-reduced aldosterone ---> dec. resorption of Na+ ---> decreased medullary hypertonicity -hyponatremia and hypochloremia ----> dec. plasma osmolality ---> dec. ADH release |
|
|
Pyometra
-mechanism for nephrogenic DI |
-endotoxins from E. coli interfere with ADH receptors
|
|
|
Hypercalcemia
-mechanism for nephrogenic DI |
-inhibits binding sites for ADH
|
|
|
Hypokalemia
-mechanism for nephrogenic DI |
-downregulates responsiveness of receptors to ADH
|
|
|
Drugs that can cause nephrogenic DI
|
-corticosteroids
-diuretics |
|
|
Liver disease
-cause for nephrogenic DI |
-dec. urea production ---> dec. urea absorption in collecting duct ---> dec. medullary hypertonicity
|
|
|
Renal medullary washout
-cause for nephrogenic DI |
-lack of a concentration gradient due to high flow through the nephron
|
|
|
Diabetes mellitus
-cause for nephrogenic DI |
-glucosuria ---> solute diuresis
|
|
|
Medullary hypertonicity
-depends on |
-medullary blood flow
-sodium absorption (dependent on GFR and PCT absorption) -Urea absorption(in the collecting ducts under ADH influence) |
|
|
Ways to distinguish PU from PD
|
-water deprivation test
-measure serum osmolality |
|
|
Polydipsia
-WDT results |
-patient produces hypersthenuric urine
|
|
|
What is a good and easy test to rule out Cushing's disease as a cause for PU/PD?
|
-urine cortisol/creatinine ratio
|
|
|
How to rule out StageI/Stage II CKD if there is persistent isosthenuria, possible proteinuria, and a high BUN/creatinine ratio
|
-renal US
-urine culture -GFR study -Blood pressure |
|
|
How to rule out renal medullary solute washout in a patient with known or suspected nephrogenic diabetes insipidus
|
-gradually reduce water intake over 10-14 days before performing a water deprivation test
|
|
|
Plasma osmolality correlates with medullary intersitium (T/F)
|
-False
|
|
|
Snormal serum osmolality
|
-280-310
|
|
|
How to test for a portosyustemic shunt
|
-Bile Acid test
|
|
|
Water deprivation test endpoint
|
-5% loss of body weight
-no need to go further if hypersthenuric urine is formed |
|
|
Reasons for hypercalcemia
|
GOSHDARNIT
-granulomatous disease -osteolytic disease -spurious (make sure it's real) -primary hyperthyroid -Vit. D3 intoxication -Addisons -Renal secondary hyperparathyroid -neoplasia**** -idiopathic -temp |
|
|
Reasons for non-regenerative anemia
|
-acute blood loss
-chronic disease -myelodysplastic disorder (lack of Epo) |
|
|
Which of the following disorders/diseases would be LEAST likely to cause pre-renal azotemia and decreased urine concentrating ability? (Assume the patient has received no treatments)
-congestive heart failiure -diabetic ketoacidosis -hypercalcemia -pyometra -hepatic disease |
-congestive heart failure
|
|
|
Which of the following is not an early finding in ethylene glycol intoxification?
-azotemia -plasma or serum hyperosmolality -PU/PD -metabolic acidosis -ataxia |
-azotemia (need metabolism before nephron damage)
|
|
|
Proteinuria
-define |
-excessive/abnormal urine protein excretion (usually albumin)
|
|
|
Normal plasma albumin level
|
4 g/dL
|
|
|
Normal albumin filtration by the glomerulus
|
2-3 mg/dL
*and most is resorbed by the proximal convoluted tubule |
|
|
Normal albumin concentration found in urine
|
< 1 mg/dL
|
|
|
Reason for albumin not passing through the glomerulus
|
-size
-charge |
|
|
2 types of proteinuria
|
-physiologic
-pathologic |
|
|
Physiologic proteinuria
-causes |
Transient
-exercise -seizures -fever -stress -heat/cold -activity level |
|
|
Types of pathologic proteinuria
|
-nonurinary proteinuria
-urinary proteinuria |
|
|
Nonurinary proteinuria
-causes |
-small molecular weight proteins (bence jones proteinuria, hemoglobinuria/myoglobinuria)
-congestive heart failure -genital tract inflammation |
|
|
Urinary proteinuria
-types |
-nonrenal proteinuria
-renal proteinuria |
|
|
Nonrenal proteinnuria
-causes |
-lower urinary tract inflammation
|
|
|
Renal proteinuria
-causes |
-glomerular proteinuria (PLN)
-tubular proteinuria -renal parenchymal inflammation (renoliths, pyelonephritis, neoplasia) |
|
|
Sign of renal parenchymal inflammation
|
-active sediment
|
|
|
Diseases associated with glomerular proteinuria
|
-glomerulonephritis-immune-complex disease
-glomerular amyloidosis -intraglomerular hypertension -structural abnormalities |
|
|
Diseases associated with tubular proteinuria
|
-acute tubular toxicity
-congenital disorers (Fanconi syndrome ---> proximal tubular necrosis) |
|
|
Proteinuria
-diagnostic methods |
-conventional urinalysis (dipstick & SSA)
-urine protein/creatinine ratio -albumin specific assay (ELISA) |
|
|
Urine dipstick advantages
|
-sensitive to albumin
|
|
|
Urine SSA advantages
|
-can detect very small amounts of protein in urine
|
|
|
Conventional urinalysis
-disadvantages |
Cats
-produce cauxin which will provide false positive readings |
|
|
urine specific gravity effects on proteinuria findings
|
-lower specific gravity with the same dipstick reading as higher specific gravity will probably have more protein present
|
|
|
Nephrotic syndrome
-define |
-glomerular proteinuria where the protein loss is high enough to cause hypoalbuminemia
*liver can keep up with protein loss |
|
|
Nephrotic syndrome
-clinical signs |
-hypercholesterolemia
-proteinuria -hypoalbuminemia -edema -hypertension -hypercoagulability |
|
|
How does the liver regulate protein synthesis?
|
-perihepatic interstitial osmoreceptors
|
|
|
How do immune complexes end up in the glomerulus?
|
-soluble circulating antigen-antibody complexes get deposited and trapped in glomeruli
-form in situ when circulating antibodies react with endogenous glomerular antigen |
|
|
Important marker of kidney disease
|
-persistent proteinuria with inactive urine- sediment
|
|
|
Why is hyperlipidemia seen with nephrotic syndrome?
|
-increased production of lipoprotein
|
|
|
Does an animal with nephrotic syndrome have to have concurrent azotemia?
|
-No, because there can still be enough functional nephrons
|
|
|
Immune-complex formation
-causes |
-drugs
-infections -vaccines -autoimmunity -neoplasia |
|
|
Only definitive method of diagnosing PLN
|
-renal biopsy (light, immunofluorescent, electron microscopy)
|
|
|
Hyaline casts
-form due to |
-excessive amounts of protein in tubular fluid
|
|
|
How to rule out transient (physiologic) proteinuria
|
-complete 2 different urine assays over a 2 week period
|
|
|
How to quantitatively diagnose proteinuria
|
-urine protein/creatinine ratio
|
|
|
Why use urine protein/creatinine ratio
|
-it will not be altered by a change in urine volume
|
|
|
UP/C ratio
-normal |
< 0.2 (
|
|
|
UP/C ratio
-borderline |
0.2-0.4 (cats)
0.2-0.5 (dogs) |
|
|
UP/C ratio
-renal proteinuria |
>0.4/0.5
tubular or glomerular *if persistent with an inactive urine sediment |
|
|
UP/C ratio
-usual glomerular proteinuria |
> 2.0
*normally not much protein is filtered through the glomerulus, so it's too much protein to be associated with a lack of tubular absorption |
|
|
Reasons to quantitate renal proteinuria
|
-assess the severity of disease
-assess the response to treatment/progression of disease |
|
|
Suspected renal proteinuria
-methods of quantitation |
1) collect all urine produced over a 24 hr period
2) UP/C ratio 3) species-specific quantitative albuminuria assays measured in diluted urine |
|
|
How does one differentiate between glomerular amyloidosis and immune complex glomerulonephritis?
|
-diagnose amyloidosis via biopsy and stain with congo red
|
|
|
Glomerulonephropathy treatment
|
-correct any underlying disease process
-immunosuppressive treatment -antiinflammatory/hypercoagulability treatment -supportiive care |
|
|
Immunosuppressive treatment for immune-mediated damage causing glomerulonephropathy
|
-mycofenolate (dogs)
-azathioprine (dogs) -cyclosporin (dogs) -prednisone/prednisolone |
|
|
Antiinflammatory/hypercoagulability treatment for glomerulonephropathy
|
-aspirin (DOGS)
|
|
|
Supportive care for treatment of glomerulonephropathy
|
dietary
-sodium reduction -high qualilty-low quantity protein -fatty acid supplement hypertension -dec. dietary sodium -Angiotensin converting enzyme inhibition (benazepril, Calcium channel blockers) edema/ascites -dietary sodium restriction -furosemide (careful of pre-renal dehydration) |
|
|
Glomerular amyloidosis
-treatment |
-None proven to be beneficial
-recommendation of DMSO and Colchicine |
|
|
How do ACE inhibitors decrease proteinuria?
|
-dec. efferent glomerular resistance ---> decreased glomerular transcapillary hydraulic pressure and decreased proteinuria
-dec. size of glomerular capillary endothelial cell pore (people) -dec. angiotensin and aldosterone ---> dec. fibrosis -slows glomerular mesangial cell growth and proliferation |
|
|
Pollakiuria
-define |
-increased frequency in urination
*not due to increased urine volume (polyuria) |
|
|
Dysuria
-define |
-difficult urination
|
|
|
Stranguria
-define |
-straining during urination
|
|
|
Hematuria
-define |
-RBCs in the urine
-gross or microscopic (>5 RBCs/hpf) |
|
|
Periuria
-define |
-urinating in abnormal/inappropriate locations
|
|
|
Cause of pollakiuria, dysuria, stranguria
|
-inflammation of the lower urinary tract
|
|
|
Lower urinary tract inflammation
-causes |
-bacterial cystitis
-uroliths -uracheal remnants -bladder tumors and polyps -prostatitis -urethritis -idiopathic cystitis in cats |
|
|
Bacterial cystitis
-common in |
-female dogs
|
|
|
Bacterial cystitis
-typical cause |
-ascension of skin and GI flora
|
|
|
Bacterial cystitis
-etiology |
Gram (+)
-staph (skin) -strep (skin/feces) -enterococcus (feces) Gram (-) -E.coli -Proteus -Klebsiella -Pseudomonas -Enterobacter |
|
|
Nonbacterial UTI
-common in |
-healthy, young cats with normal urine concentrating ability
*Bacterial UTI rare in healthy cats |
|
|
Why are LUTIs not as common in male dogs
|
-prostatic secretions contain zinc which is bacteriostatic
|
|
|
Types of UTIs
|
-uncomplicated infection
-complicated infection -recurrent infection |
|
|
Uncomplicated infections
-define |
-no underlying defects in the host immune system
*respond quickly to appropriate antibiotic therapy *often don't need to treat |
|
|
Uncomplicated infections
-cause |
-hygiene
-exposure to bacteria |
|
|
Complicated infections
-define |
-underlying defects in host dfense mechanisms are present
*signs persist after appropriate antibiotic treatment or come back shortly after treatment is ceased |
|
|
Complicated infections
-causes |
-abnormal micturition (urine retention/leakage)
-anatomical abnormalities (ectopic ureter) -mucosal damage (urolith) -alterations in urine volume and/or composition (diabetes mellitus) -systemic immunocompromise (Cushings) |
|
|
Recurrent UTIs
-types |
-relapse
-reinfection |
|
|
Relapse
-define |
-same organism
-relatively short amount of time between episodes |
|
|
Relapse
-primary cause |
-inappropriate antibiotic therapy
*antibiotic resistance *bacteria sequestration from antibiotics |
|
|
How may bacteria become sequestered so that antibiotics have little to no effect?
|
-thickened mucosa
-inside uroliths |
|
|
When a relapse has occurred, what should you focus on for treatment?
|
-owner compliance
-resistance -something going on systemically (GI tract can't absorb antibiotic) |
|
|
Reinfection
-define |
-different organism
-longer time between episodes |
|
|
Reinfection
-causes |
-underlying defect in host defense mechanism
-iatrogenic/spontaneous reinfection |
|
|
What should you focus on for treatment of reinfections?
|
-local anatomic issues
-systemic disease processes |
|
|
Which of the following would be lease likely to cause a complicated UTI?
-hyperadrenocorticism -urine retention or urine leakage -urolithiasis -superficial pyoderma -diabetes mellitus |
-superficial pyoderma
|
|
|
Hematuria that occurs without signs of LUTI typically due to:
|
-kidneys (tumor, clotting defect, etc.)
|
|
|
Steps to manage a urinary tract infection
|
1) diagnose based on history, urine sediment, and urine culture and sensitivity
2) select antimicrobial agent 3) reculture in 3-5 days to determine efficacy of selected antibiotic 4) examine urine sediment 3-4 days before discontinuing antibiotic 5) repeat urinalysis and culture in 1-2 wks following end of antibiotic therapy 6) Recurrent UTIs should be evaluated for underlying predisposing factors 7) Frequent reinfection may need prophylactic antibiotic after initial inflammation cleared up |
|
|
Local host defenses that inhibit bacterial colonization of the bladder and kidneys
|
-anatomical structures
-mucosal defense barriers -antibacterial properties of urine -normal voiding -systemic immunocompetence |
|
|
Antibacterial properties of urine
|
-low pH
-increased urea and weak organic acids -zinc form prostatic secretions in males |
|
|
Anatomical prevention of LUTIs
|
-urethral high-pressure zones
-urethral contraction and peristalsis -longer urethra length in males -vesicoureteral junction |
|
|
Mucosal defense barriers to prevent against LUTIs
|
antibody and mucoprotein production
-coat pathogenic bacteria -form protective barrier Nonpathogenic flora colonization -fill up epithelial receptor sites -produce bacteriocins which interfere with uropathogen metabolism |
|
|
Virulence factors of LUTI bacteria
|
-fibmbriae
-Capsular K antigens -O antigens in endotoxin -cell wall -colicons -hemolysins -beta-lactamase -dulcitol fermentation -erythrocyte agglutination -drug resistance |
|
|
Fimbriae
-function in virulence |
-facilitate attachment to uroepithelium
-on Gram (-) |
|
|
Capsular K antigen
-function in virulence |
-increase invasiveness
-interfere with opsonization and phagocytosis |
|
|
O antigen in endotoxin
-function in virulence |
-decrease smooth muscle contractility
|
|
|
Cell wall
-function in virulence |
-can exist in hypertonic environments (urine, renal medulla)
|
|
|
Colicins
-function in virulence |
-increase vascular permeability
*E. coli |
|
|
Hemolysins
-function in virulence |
increase invasiveness through tissue damage
|
|
|
Beta-lactamase
-function in virulence |
-resistance to beta-lactam antibiotics
|
|
|
Dulcitol fermentation
-function in virulence |
resistance to phagocytosis
|
|
|
Erythrocyte agglutination
-function in virulence |
-uroepithelial adherence
|
|
|
E. coli (gram -) treatment
|
-trimethoprim sulfa
-enrofloxacin |
|
|
Gram + treatment
|
-amoxicillin
|
|
|
Prostatitis
-clinical signs |
-difficulty defecating
|
|
|
Pyelonephritis
-clinical signs |
-painful abdominal palpation
|
|
|
Metritis
-clinical signs |
-vulvar discharge
-painful abdomen on palpation -systemic signs (depression, anorexia) |
|
|
Cystitis
-clinical signs |
-stranguria
-hematuria -dysuria |
|
|
Antibiotics that can cross the blood-prostate barrier
|
-lfuoroquinolones
-trimethoprim sulfa -chloramphenicol*********** (high lipid solubility) -carbenicillin |
|
|
Possible reasons for a poor response when treating bacterial cystitis
|
-ineffective drug/duration
-failed owner compliance -GI or oral disease affecting drug absorption -drug resistance -iatrogenic infection (catheter) -impaired action of drug -mixed infection |
|
|
A 3-year-old neutered male domestic shorthair cat with intermittent episodes of hematuria, dysuria, and urinating outside the litter box is presented to you for evaluation. Another veterinarian in town has prescribed several antibiotic regimens over the past 6 months and the cat seems to respond each time. The owner is concerned that no cause has been identified for the cat’s signs and is coming to you for a second opinion. Which one of the following would be the most appropriate next step for managing this cat?
-switch to a more appropriate antimicrobial (enrofloxacin) -recommend a longer duration of antimicrobial treatment (4-6 weeks) -perform cytoscopy -recommend changing to a therapeutic food for struvite prevention -perform abdominal radiograph |
-perform an abdominal radiograph
|
|
|
Radiodense uroliths
|
-Calcium oxalate
-Struvite |
|
|
Intermediate density uroliths
|
-silicate
-cystine |
|
|
Radiolucent uroliths
|
-urates
|
|
|
Most appropriate method to screen for uroliths
|
-lateral radiograph
-double contrast study |
|
|
Double contrast studies are best for identifying
|
-urate uroliths
|
|
|
Structures found on the periphery of the bladder in a double contrast study
|
-air bubbles
-blood clots |
|
|
Struvite
-composition |
-magnesium ammonium phosphate
|
|
|
Struvite
-common breeds |
-miniature schnauzers
-bichon frise -cocker spaniel -miniature poodles |
|
|
Struvite
-sex |
-female
|
|
|
Struvite
-opacity |
-radiodense
|
|
|
Struvite
-precipitating pH |
-alkaline urine
|
|
|
Struvite
-pathophysiology |
-very commonly due to urease producing bacteria (UTI: Staph. & Proteus)
-high protein diet supersaturating urine with magnesium, ammonium, phosphate (not a large influence) |
|
|
Struvite
-treatment |
Surgical removal
or Dissolution: -Hills s/d diet -Control infection (long term antibiotic treatment based on C/S) -urease inhibitor (acetohydroxamic acid) -urine: acidify <6.5; BUN < 10 mg/dl; USG <1.020 |
|
|
Struvite
-prevention |
-Hills c/d diet
-monitor urine pH, urine sediment, treat infections quickly and appropriately |
|

|
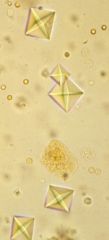
-struvite
|
|
|
Can there be uroliths without crystals?
|
-yes
*and there can be crystals without uroliths *when both are present, likely to be uniform composition |
|
|
Calcium oxalate
-radiodensity |
-radiodense
|
|
|
Calcium oxalate
-breeds |
-yorkshire terrier
-lhasa apso -shih tzu -miniature schnauzer -miniature poodle -bichon frise |
|
|
Calcium oxalate
-sex |
-males
|
|
|
Calcium oxalate
-precipitating pH |
-Acid
|
|
|
Calcium oxalate
-pathophysiology |
-rare from UTI
-occasional hypercalcemia -increased calcium from the gut (postprandial) or defective tubular reabsorption (renal leak) |
|
|
Calcium oxalate
-treatment |
-surgical removal
-decreased intake of oxalates? (grass, greens, etc) |
|
|
Calcium oxalate
-prevention |
-Hills u/d diet?
-potassium citrate (citrate competes with oxalate for calcium, but citrate stays soluble and doesn't form stones; alkalinizing) |
|

|
-monohydrate calcium oxalate crystals
|
|
|
-dihydrate calcium oxalate crystals
*Maltese cross |
|
|
Monohydrate calcium oxalate crystals
-commonly seen in what condition |
-ethylene glycol toxicity
|
|
|
Urate (Ammonium urate)
-breeds |
-Miniature schnauzer (PSS)
-Yorkshire terrier (PSS) -Dalmation |
|
|
Urate (Ammonium urate)
-precipitating pH |
-Acid (urate)
-Alkaline (Ammonium) -can see in neutral pH |
|
|
Urate (Ammonium urate)
-radiodensity |
-radiolucent
|
|
|
Urate (Ammonium urate)
-sex |
-males
|
|
|
Urate (Ammonium urate)
-pathophysiology |
-uncommon UTI
-decreased serum BUN, and albumin -abnormal pre and postprandial bile with PSS -urea cant be metabolized due to bypassing liver |
|
|
Urate (ammonium urate)
-treatment |
Surgical removal
or Dissolution: -Hills u/d diet -Allopurintol -control infection |
|
|
Urate (Ammonium urate)
-prevention |
-Hills u/d diet
-allopurintol (if necessary) ---blocks xanthine oxidase |
|
|
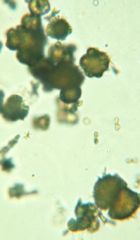
-urate crystals
*thornapple crystals |
|
|
Cystine
-radiodensity |
-intermediate density
|
|
|
Cystine
-breeds |
-Yorkshire terrier
-Dachshund -Bassett Hound -English Bulldog -Irish terrier -Rottweiler -Chihuahua -Mastiff |
|
|
Cystine
-sex |
-males
|
|
|
Cystine
-precipitating pH |
-acid
|
|
|
Cystine
-pathophysiology |
-rare UTI
-primary cause is an inherited disorder or renal tubular defect in cystine reabsorption |
|
|
Cystine
-treatment |
Surgical removal
or Dissolution: -Hills u/d diet -D-penicillamine -MPG |
|
|
Cystine
-prevention |
-Hills u/d/ diet
-thiol containing drugs (if necessary) |
|
|
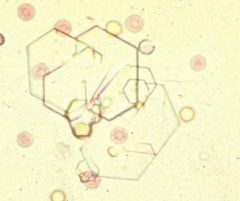
-cystine crystals
*hexagonal |
|
|
Silicate
-radiodensity |
-intermediate/radio dense
|
|
|
Silicate
-Breeds |
-German shepherd
-Golden retriever -Labrador retriever -Old English Sheepdog |
|
|
Silicate
-sex |
-Male
|
|
|
Silicate
-precipitating pH |
-acid/neutral
|
|
|
Silicate
-pathophysiology |
-uncommon due to UTI
-predisposition due to consumption of corn gluten or soybean hulls |
|
|
Silicate
-treatment |
-surgical removal
|
|
|
Silicate
-prevention |
-Hills u/d diet
-prevent consumption of dirt or grass |
|
|
Struvite
-urolith shape |
-jack shaped
*not diagnostic |
|
|
For which of the following disorders is a urine culture most indicated?
-hyperadrenocorticism -hyperparathyroidism -hypoadrenocorticism -hypercalcemia -hypothyroidism |
-hyperadrenocorticism
|
|
|
Struvite Urolith Dissolution
-medical management will be ineffective if: |
-dietary compliance is less than 100%
-urinary tract infection persists -uroliths are not struvite |
|
|
You treat a female dog for UTI based on urine culture and sensitivity
but hematuria and dysuria persist despite the antibiotic treatment. A urinalysis shows alkaline urine (fasted sample), struvite crystalluria, and gram negative rods. Subsequently, you take abdominal radiographs which show a radio-dense urolith within the urinary bladder. Which urolith type and bacteria are most likely? -struvite (proteus) -struvite (E. coli) -calcium oxalate (proteus) -ammonium urate (E. coli) -cystine (klebsiella) |
-struvite (proteus)
|
|
|
Is an infection with stone present indicative os a complicated or uncomplicated UTI?
|
-complicated (effects bladder muscosa ---> inflammation)
|
|
|
Surgical treatment of uroliths
-pros |
-can definitively diagnose urolith type
-concurrent or predisposing anatomica abnormalities can be corrected -urinary bladder mucosal samples can be a=obtained for bacterial culture |
|
|
Surgical treatment for uroliths
-cons |
-anesthesia
-invasive -possible incomplete removal -persistence of underlying causes |
|
|
Medical treatment of uroliths
-pros |
-decrease concentration of calculogenic salts in urine
-increase salt solubility in urine -increase urine volume (dilute calcugenic salts) |
|
|
Medical treatment of uroliths
-cons |
-owner compliance required for weeks to months
-cost (muliple UA, bacterial culture, frequent radiographs) -Calcium oxalate, calcium phosphate, silicate, mixed composition don't respond to treatment |
|
|
Feline Lower Urinary Tract Disease
-define |
Syndrome (not a specific disease) characterized by one or more of the following:
-pollakiuria -dysuria/stranguria -hematuria -urinating in inappropriate location -partial or complete urethral obstruction |
|
|
FLUTD
-recurrence |
-common
|
|
|
Is UTI a major reason for FLUTD?
|
-no
|
|
|
FLUTD
-causes/mimics |
-uroliths
-UTI (rare) -anatomic abnormalities -Trauma (rare) -Neurologic disorder (rare) -Neoplasia (rare) -Behavioral abnormalities *cause usually remains unknown and is classified as idiopathic |
|
|
Feline uroliths
-most common uroliths |
-struvite
-calcium oxalate |
|
|
Feline uroliths
-struvite common in |
-younger cats
|
|
|
Feline uroliths
-Calcium oxalate common in |
-older cats
|
|
|
Feline uroliths
-probable cause for increased Calcium oxalate uroliths |
-use of magnesium-reduced, acidifying diets to prevent struvite urolith formation
|
|
|
Feline uroliths
-Calcium oxalate risk factors |
-breed (Burmese, Himalayan, Persian)
-indoor only housing -lack of dietary variety -overweight -neutered male |
|
|
Feline urolith
-Struvite treatment |
-dissolution
|
|
|
Feline uroliths
-Struvite prevention |
-diet
|
|
|
Feline uroliths
-Calcium oxalate treatment |
Surgery
-can't be dissolved |
|
|
Feline uroliths
-Calcium oxalate prevention |
-diet
|
|
|
Why is bacteriuria observed with FLUTDs even though UTI as a cause is rare?
|
Sample collecting techniques
-cystocentesis = sterile -catheter and voided = not sterile |
|
|
Idiopathic FLUTD
-possible major factor |
-stress
|
|
|
Idiopathic FLUTD
-treatment |
-switch to wet cat food (inc. water intake --> dec. urine concentration ---> dec. uroepithelium concentration)
-dec. stress/environmental enrichment -pain therapy if necessary |
|
|
FLUTI
-antibiotic therapy |
-"response" to antibiotics
-nothing documents efficacy -placebo effect -waxing-waning course of infection that can result in resolution without treatment (high recurrence rate) |
|
|
Bacterial UTI in cats
-due to |
Compromised host defense mechanism
-CKD -Diabetes mellitus -hyperthyroidism -corticosteroids -urinary catheters (indwelling catheters, concurrent fluid therapy --> dec. concentration of urine antimicrobial properties) |
|
|
Idiopathic FLUTI
-diagnosis |
-diagnosis of exclusion
|
|
|
Difference in struvite crystal formation between cats and dogs
|
-Dogs: concurrent UTI (Staph or Proteus)
-Cats: no UTI; high concentrating ability |
|
|
Hyperkalemia
-clinical signs |
-anorexia
-vomiting -dehydration -depression -weakness -collapse -stupor -hypothermia -acidosis -hyperventilation |
|
|
Hyperkalemia
-ECG signs |
-bradycardia
-flattened waves -prolonged PR interval; widened QRS complex -tall T waves -arrhythmias |
|
|
How to manage a male cat with urethral obstruction and hyperkalemia
|
-pass a catheter to relieve urine pressure and to allow potassium to start exiting the body
-IV fluid therapy -IV bolus of insulin followed by dextrose or -IV bolus of bicarbonate or -IV bolus of calcium gluconate |
|
|
What approach would you take with a cat that has pollakiuria, stranguria/dysuria, and hematuria, and an alkaline urine pH with struvite crystalluria? What would you do if there was no response in 5-7 days?
|
-Dietary trial (Hills s/d)
-survey/contrast radiographs (if abnormal surgery/biopsy) |
|
|
How do you diagnose idopathic FLUTD?
|
Absence of an identifiable cause of urinary tract disease
-history (pollakiuria, dysuria/stranguria, hematuria) -PE (rectal palpation of caudal bladder and urethra to determine if masses or calculi) -Abdominal palpation after voiding (determine residual urine volume and if there are residual masses or uroliths) -Complete urinalysis (cystocentesis) |
|
|
How to treat idiopathic FLUTD
|
-canned food
-dec. stress -increased play -increased water -pain meds if necessary |
|
|
Micturition
-define |
Process of:
-storage of urine -voiding of urine |
|
|
Disorders of micturition can result from:
|
-failure of urine storage (leakage/incontinence)
-failure of voiding ---> urine retention |
|
|
Urine retention
-causes |
-decreased bladder tone
-uretheral obstruction |
|
|
Storage phase of micturition
-due to |
sympathetic nervous system
-hypogastric nerve (L1-L4) -alpha-adrenergic stimulation ----> contraction of smooth muscle of the internal urethral sphincter -beta-adrenergic stimulation ---> relaxation of the detrussor muscle |
|
|
Stretching/filling of the bladder
-perceived how |
-sensory fibers of the pelvic nerve S1-S3
|
|
|
Voiding phase of micturition
-due to |
Parasympathetic nervous system
-Pelvic nerve (S1-S3) -Cerebral cortex ---> Pons ---> reticulospinal pathway ---> S1-S3 ---> Pelvic nerve -cholinergic stimulation to the detrussor muscle ---> contraction -reflex inhibition of the sympathetic system |
|
|
External urethral sphincter
-control |
-voluntary control via pudendal nerve (S1-S3)
|
|
|
Ganglia of the hypogastric nerve
|
-caudal mesenteric ganglia
|
|
|
Pudendal nerve
-effects what |
-external urethral sphincter
-perineum |
|
|
Micturition disorders
-classification |
-Big bladders
-Small/Normal sized bladders |
|
|
Big bladders
-due to |
-decreased detrusor contractility (hypocontractility)
-increased urethral outflow resistance |
|
|
Small bladders
-due to |
-increased detrussor contractility (hypercontractility)
-decreased urethral outflow resistance |
|
|
Decreased detrussor contractility
-treatment |
-keep bladder small
-treat with cholinergic drugs |
|
|
Increased urethral outflow resistance
-treatment |
-alpha-blockers
-skeletal muscle relaxants -relieve anatomic obstruction |
|
|
Increased detrussor contractility
-treatment |
-treat underlying cause of inflammation
|
|
|
Decreased urethral outflow resistance
-treatment |
-hormones (estrogen or testosterone)
-alpha-adrenergic drugs |
|
|
Big bladder disorders
-examples |
-upper motor neuron disease
-lower motor neuron disease -reflex dyssynergia -anatomical urethral obstruction |
|
|
Small bladder disorders
-examples |
-urethral sphincter mechanism incompetence
-urge or inflammatory incompitence -congenital anomalies (ectopic ureter, vaginal stricture) |
|
|
Lower motor neuron disease
-causes |
Big bladder
-lesion to spinal cord segments S1-S3 (neoplasia, trauma, cauda equina syndrome) -trauma to the pelvic nerve, pelvic surgery, detrusor atony, canine and feline dysautonomia |
|
|
Upper motor neuron disease
-causes |
Big Bladder
-lesion cranial to S1 (intervertebral disk protrusion, neoplasia, trauma, fibrocartilaginous infarct, meningitis) -cerebral disease, cerebellar disease, brain stem disease |
|
|
Reflex dyssynergia
-causes |
Big Bladder
-inknown |
|
|
Anatomic outflow obstruction
-causes |
Big Bladder
-urethral stricture -neoplasia -cystic or urethral calculi -granulomatous urethritis -prostatic disease |
|
|
Urethral Sphincter Mechanism Incompetence
-causes |
Small/Normal Bladder
-aging changes ---> decreased muscle tone and structural support and/or decreased hormone concentration |
|
|
Urge incontinence
-causes |
Small/Normal Bladder
-bladder irritation -urethral irritation |
|
|
Congenital
-causes |
-Ectopic ureters
-patent urachus -urethral fistula -pseudohermaphroditism -vaginal stricture |
|
|
Lower Motor Neuron
-clinical signs |
-dribbling or urine
-distended bladder that is easily expressed -history of trauma or surgery to the pelvic region |
|
|
Upper motor neuron
-clinical signs |
-distended bladder that is difficult to express but easy to catheterize
-paresis or paralysis may be present |
|
|
Reflex dyssynergia
-clinical signs |
-male, large breed dogs
-urine stream initiated then interrupted -distended bladder that is difficult to express but easy to catheterize |
|
|
Outflow obstruction
-clinical signs |
-males
-dysuria/stranguria -dribbling of urine -bladder that is difficult to express and catheterize |
|
|
Urethral sphincter mechanism incompetence
-clinical signs |
-middle-aged to older neutered or spayed dogs
-dribbling or urine usually occurs when animal is relaxed or asleep (normal voiding otherwise) |
|
|
Urge incontinence
-clinical signs |
-pollakiuria
-dysuria/stranguria -hematuria -bacteriuria (may be idiopathic: overactive bladder syndrome) |
|
|
Congenital abnormalitis
-clinical signs |
-young animal
-constant dribbling of urine may occur but normal voiding otherwise |
|
|
How is there urine leakage with large bladders
|
-with time urine retention causes increase intravesicular pressure which increases past outflow resistance
|
|
|
Gold standard for diagnosing increased outflow resistance
|
-retrograde positive contrast urethrogram
|
|
|
Micturition disorders are more commonly:
|
-small/normal sized bladder disorders
|
|
|
How to differentiate decreased outflow resistance from bladder hypercontractility
|
Decreased outflow resistance
-relaxed sphincter leakage most evident when relaxed/sleeping Bladder hypercontractility -abnormal household behavior -may have red cells, white cells, crystals ----> urine inflammation |
|
|
Cholinergic drug used to keep the bladder small
|
-Bethanecol
|
|
|
Drug to treat increased outflow resistance
|
alpha blocker
-phenoxybenzamine -prazosin |
|
|
When passing a urinary catheter, what should be administered?
|
-alpha-blocker
|
|
|
How to diagnose ectopic ureters
|
-intravenous pyelogram
|
|
|
Urinary system anatomic abnormalities are usually accompanied with
|
-incompetent urethral sphincter
-do a urethral pressure profile through the sphincter |
|
|
A lesion of the S1-S3 spinal cord segments would be most likely to cause which of the following?
-reflex dyssynergia -urine retention with a bladder that is east to express -normal to increased anal tone -incontinence with a small bladder -none of the above |
-urine retention with a bladder that is easy to express
|
|
|
Which one of the following drugs affects urinary bladder detrussor tone?
-phenylpropanolamine (alpha agonist) -phenoxybenzamine (alpha antagonist) -bethanecol (cholinergic) -diethylstilbestrol (hormone replacement) |
-bethanecol (cholinergic)
|
|
|
Pelvic nerve
-function |
Parasympathetic
-sensory: sense bladder fullness -motor: stimulation of detrussor muscle to contract |
|
|
Cystocentesis
-significant number of bacteria |
>1000
|
|
|
Catheterization
-significant number of bacteria |
>10,000
|
|
|
Voided or Expressed urine
-significant number of bacteria |
>100,000
|

