![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
List the cytokines involved in:
1. Vasodilation 2. Vascular permeability 3. Chemotaxis 4. Fever 5. Pain 6. Tissue damage |

|
|
|
What is chronic inflammation?
|
- Long standing inflammation.
- Characterised by cells involved = the chronic inflammatory / mononuclear cells - Results in tissue destruction, fibrosis and repair → scar tissue and always some loss or function. - Granulomatous inflammation is one specific pattern of chronic inflammation |
|
|
How does chronic inflammation arise?
|
- May take over from acute inflammation → If disease lasts more than a few days, insult cannot be removed or damage is significant
- May arise de novo → Chronic infections, auto-immune disease → Chronic irritation - May develop alongside acute inflammation → In more severe persistent irritation |
|
|
Give 4 specific causes of chronic inflammation
|
1. Persistent infections e.g. syphilis, TB, viral hepatitis, HP related gastritis.
2. Prolonged exposure to toxins, e.g.silica, atherosclerosis endogenous lipids 3. Autoimmune diseases e.g. Graves disease, ulcerative colitis, primary biliary cirrhosis. 4. Non resolving acute inflammation, e.g. bed sores |
|
|
What are the 3 patterns of chronic inflammation
|
1. Lymphocytic → infiltration of lymphocytes e.g. auto-immune thyroid disease, chronic hepatitis
2. Granulomatous → formation of granulomas e.g. TB, sarcoidosis, Crohn's disease 3. Mixed acute and chronic inflammation e.g. chronic active gastritis, ulcerative colitis |
|
|
What cells are involved in chronic inflammation?
|

- Mononucleated cells
1. Macrophages = nucleus cigar-shaped, vesicular chromatin, very pale cytoplasma 2. Lymphocytes = dark round nucleus, very little cytoplasm 3. Plasma cells = clock-faced nucleus 4. Eosinophils |
|
|
Describe the features of the innate and adaptive immune systems
|
Innate:
- No previous exposure required - Reacts to bacterial wall and virus proteins - TOL Like receptors (TLRs) = conserved receptors on responsive cells which recognise foreign particles - Phagocytosis by neutrophils and macrophages carrying TLRs - Complement activated = cascade of proteins which disrupt membrane Adaptive - Previous exposure required - Response specific to that organism - Depends on APC processing antigens - Recruitment of unique lymphoid cells |
|
|
What is Nuclear factor Kappa B (NF-κB)?
|
- Rapid acting primary transcription factor
- Found in the signalling pathway of TLRs on neutrophils and macrophages - Five members of the NF-κB family - Present in the cytoplasm and activated by both non-canonical and canonical pathways - Activated NFκB translocates from cytoplasm to nucleus - Transactivation of up to 200 genes in inflammatory response, cell proliferation, and cell survival pathways - Rapid acting = doesn't require transcription itself |
|
|
Describe the features and functions of the macrophage
|

- Derived from blood monocytes
- Different levels of activation - Phagocytosis and destruction of bacteria and debris. - Control of other inflammatory cells by means of cytokines. - Secrete a number of factors involved in tissue destruction and tissue repair. - Processing and presenting antigen to the immune system. |
|
|
What are the various types of macrophage?
|

Reticuloendothelial system = tissue bound macrophages
|
|
|
What are the factors that activate macrophages, and what happens to the macrophage on activation?
|
Macrophage activating factors:
- Cytokines – IFNγ (γ-interferon) from T Cells - Bacterial endotoxins - Chemical mediators of inflammation - ECM proteins Activation means - Epithelioid cell type (known as this when they have developed voluminous cytoplasm) - Increased size = increased cytoplasm - Increased metabolic rate = subcellular apparatus for protein synthesis develops - Increased phagoctyic activity - Often form multinucleated giant cells by fusion of active macrophages |
|
|
Describe the secretions of the activated macrophages
|
1. Tissue damaging agents
- Proteases, Collagenase, and Lipases → dissolution of extracellular material - Neutrophil chemotactic factors - Coagulation factors - Arachidonic acid derivatives = mediators of acute inflammation - Nitric oxide and highly reactive oxygen metabolites → bacterial and cell killing 2. Pro-fibrotic tissue repair factors - Growth factors (PDGF, FGF, TGFb) = stimulate growth of blood vessels, and division and migration of fibroblasts - Fibrogenic cytokines, IL-1, TNFα = stimulate fibroblast proliferation and collagen synthesis, which are important in the reparative response - Angiogenic factors - Remodelling collagenases All factors are secreted in varying amounts depending on the type of stimulation on the cell |
|
|
Describe the process of accumulation of macrophages
|
1. Recruitment from circulation via endothelial receptors and chemotaxis - C5a, IL8 Chemokines (MCP-1), TGF Beta.
2. Immobilization - Macrophage inhibitory factor, oxidised lipids. 3. Proliferation. |
|
|
What are lymphocytes?
|
- Normally present in lymph nodes and other tissues
- T cells release cytokines and have cytotoxic functions = Thymus selects the useful, neglects the useless and destroys the harmful. - B cells responsible for antibody production = Bone marrow - Both types undergo maturation in secondary lymphoid tissue (lymph node spleen and mucosal associated lymphoid tissue) |
|
|
Describe the features of B lymphocytes and Plasma cells
|
- B cells found in the cortex of lymph nodes (follicles)
- Naïve Bcells are non antigen sensitized - Mature in the primary follicle following APC antigen presentation, with T helper cell - Undergo IG gene rearrangement with selection of successful clone - Matures to memory B cell or plasma cell - Plasma cells are immunoglobulin factories - Clonal i.e. produce one unique antibody per cell |
|
|
Describe the features of T cells
|
- TCR is unique to one antigen
- T4 Helper/Inducer need Ag+MHCII • TH1 release IFNγ & IL2. Found in cellular response and granulomatous disease as well as Immunoglobulins • TH2 release IL4 IL5 & IL13 → Facilitates Ab production - T8 Supressor/cytotoxic need Ag+MHC1 |
|
|
Describe the features of eosinophils and mast cells in the chronic immune response
|

Eosinophils
- Have membrane bound IgE, and important in IgE mediated reactions and parasites infections (allergy etc). - Eotaxin is important in recruitment. - Release Major Basic Protein, a cationic protein toxic to many parasites. - Present in some tumours. Mast cells - Tissue bound = also have membrane bound IgE - Important in anaphylaxis reaction - Important in acute and chronic inflammation - Release cytokines |
|
|
Describe 4 possible complications of chronic inflammation
|
- Never get complete resolution back to normal
1. Fibrosis - TB, 'hour glass' stomach = distorts organs → strictures etc 2. Scarring with dysfunction e.g. cirrhosis (chronic hepatitis), intestinal stenosis (Crohn's) 3. Atrophy e.g. gastric mucosa in chronic auto immune → left with simple tubular crypts, thin mucosa and high surface mucous cells 4. Metaplasia e.g. bronchus, oesophagus, and bladder (transitional to squamous) |
|
|
Describe the regulation of inflammation
|
- Elimination of noxious agent leading to reduction of pro-inflammatory mediators -PGs, Leukotrienes, TNF etc.
- Regulatory T cells under control of FoxP3 → TH2, TR1 - Repressing cytokines IL10, TGFβ and receptor fragments for TNF, Annexin A-I (activates leukocytes and sends them to the site of infection directly, inhibiting neutrophil extravasation and down regulates the magnitude of the inflammatory response) - Systemic hormones • Adrenal glucocorticoids, adrenaline and α-melanocyte stimulating hormone (αMSH) • Autonomic nervous system - vagal suppression via nicotinic receptors on macrophages |
|
|
Describe the features of granulomatous inflammation
|
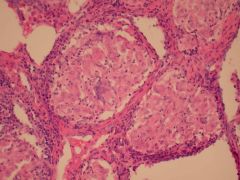
- Chronic inflammation characterised by the presence of granulomas.
- Granulomas are collections of macrophages, often with giant cells. - Granuloma formation • Response to chronic (persistent) low grade antigen stimulation. • Delayed hypersensitivity reaction. • Foreign material • Insoluble antigens - TH1 cells - secrete - IL2 IFNγ = promote macrophage accumulation |
|
|
What are the 3 types of granulomata?
|
1. Necrotizing e.g. TB and Wegner's granulomatosis
2. Naked e.g. Sarcoidosis (no necrosis) 3. Foreign body |
|
|
List 7 granulomatous diseases
|
Infections
1. Mycobacteria e.g. TB 2. Syphilis 3. Cat scratch disease Autoimmune 4. Rheumatoid nodules Idiopathic 5. Crohns disease 6. Sarcoidosis Foreign body (7) |
|
|
Describe the features of giant cells
|

- Several macrophages fuse to form giant cells = nuclei exist in the cytoplasm and many cells contribute to the cell membrane
- Often (but not always) in granulomatous inflammation - Major role in phagocytosis of foreign bodies - Langhans is a characteristic giant cell seen in TB - Distinguished by the arrangement of the nuclei = horse-shoe shaped |
|
|
Describe the features of tuberculosis
|

- Archetypal chronic inflammatory disease
◘ Causes: - Mycobacterium tuberculosis hominis or Mycobacterium tuberculosis bovis (rare) - Various other mycobacterial species can cause infection in the immunocompromised. - Aerobic bacteria with a waxy coat - Requires special stain (Ziehl Neelson) acid alcohol fast (AFB) ◘ Epidemiology: - 8 million people affected worldwide - 2 million die from TB - Particularly prevalent in Sub-Saharan Africa, India, and South East Asia. - Multi-drug resistant strains becoming common especially in Russia. - Associated with poor socioeconomic conditions. - Less common in Britain largely due to public health measures, and vaccination. - TB is a notifiable disease ◘ Primary TB: - Initial infection small granuloma = Gohn focus → casseous necrosis surrounded by fibrous tissue - Involvement of hilar lymph node = Gohn complex - Usually heals with minor scarring - Occasionally progressive primary TB (TB proper) • Massive hilar lymphadenopathy • TB pneumonia • Miliary TB ◘ Latent Period: - Individuals well and disease free. - Small granulomata in lungs, often fibrosed, and barely visible. - Low mTb load often not detectable, sputum negative. - Patients not infective. ◘ Secondary TB: - Apex lungs (aerobic bacteria and need high O2 tension). - Re-activation of primary infection - Variable and unpredictable disease. - Particularly likely to breakout in “run down” patients. - Granulomas with caseation = central necrosis. - TH1 control via cytokines chiefly IFNγ. ◘ Outcomes of Secondary TB = Arrest fibrosis scaring - Cavitation of large granulomas = Tubercle • Erosion into bronchus - infectious patients • Erosion into pulmonary vessels - Consumption • Pleura - tuberculous empyema - Erosion in pulmonary artery or vein - Miliary TB • Distant blood borne spread • Lymph nodes kidneys, adrenal gland (Addison’s disease), fallopian tubes (infertility), epididymis, brain, skin (lupus vulgaris) |
|
|
Describe the features of sarcoidosis
|

- Idiopathic
- Systemic disease with many manifestations - Pulmonary nodules with lymphadenopathy common - Most commonly affects women, especially Afro-Caribbean and Caucasians - Unknown in Asian and Chinese - Small well formed non-caseating granulomas (mortar-wall granulomas) with histiocytic giant cells - Frequently accompanied by fibrosis - Affected patients most commonly present with clinical disease related to lung involvement, or with evidence of bilateral hilar lymph node enlargement - Diagnosis of exclusion: fungi, mycobacterium berylliosis etc. - Treatment: corticosteroids e.g. prednisone, tapered over a 6-month period, or (where steroid-resistance, or side-effects) methotrexate. For patients with advanced sarcoid-induced pulmonary fibrosis, lung transplantation is the only hope for long-term survival |
|
|
Describe the features of Crohn's disease
|

- Gastrointestinal granulomatous disease with systemic manifestations.
- Idiopathic, but polymorphisms in NOD 2 (a co-factor in the NaK3 pathway) have recently been implicated. - Affects any portion of GIT most commonly terminal ileum. - Caucasians and western populations most commonly affected - Transmural chronic inflammation with small granulomata and fissure ulcers → cobblestone appearance - Granulomas not in all cases, and are small where present |
|
|
Describe the features of leprosy
|

- Chronic granulomatous disease involving Mycobacterium leprae
- Infection results in a clinical disease in a minority of patients - Affects skin and peripheral nerves - Can lead to irrepairable nerve damage and disability - 3 types: 1. Lepromatous = multi-bacterial form with strong humoural response but little cell-mediated immunity → wide-spread lesions, disfiguring nodularity of the skin. Lesions contain lymphocytes, plasma cells and macrophages filled with organisms 2. Borderline 3. Tuberculoid = pauci (low)-bacterial form with few skin lesions. Focal areas of skin pallor and anaethesia due to early involvement of nerves. Basic lesion is a follicular granuloma (tubercle) similar to a true tubercle follicle. Cell-mediated immunity is well-developed - Treatment = Dapsone (blocks folic acid synthesis → bacteriostatic) and Rifampin (Inhibits DNA-dependent RNA polymerase → bactericidal) once a month, plus clofazimine (slowly bactericidal, inhibits growth, anti-inflammatory) once a month for a year. Educate patients on nerve damage and properly treat any effects of nerve damage to prevent deformity. Surgical drainage of nerve abscesses can restore function if noted quickly - Significant associations in SNPs in five genes including NOD2, HLA-DR, RIPK2 - Associations stronger in multi-baciliary form compared to the pauci-baciliary form |
|
|
Describe the features of syphilis
|

- Sexually transmitted granulomatous infection caused by T. pallidum
- Primary syphilis = during the first 3 weeks of infection. • Formation of hard chancre characterised by lymphocytes and plasma cells (not polymorphs = not an abscess and healing occurs without scarring) - Secondary syphilis lesions are quite variable in their manifestations. • Widespread mucocutaneous lesions are observed over the entire body. Most often, the lesions are macular, discrete, reddish brown, and 5 mm or smaller in diameter • All such lesions contain treponemes. Of these, wet mucous patches are the most contagious. • Histologically, the inflammatory reaction is similar to but less intense than that of the primary chancre. - Tertiary syphilis • The pathognomonic lesion of tertiary syphilis is the gumma, a granuloma which is characterized by a center of necrotic tissue with a rubbery texture (coagulative necrosis. • Gummas principally form in the liver, bones, and testes. • Histological examination shows palisaded macrophages and fibroblasts, as well as plasma cells surrounding the margins. • Treponemes are rarely visualized or recovered from these lesions. - Treat with antibiotics e.g. penicillin |

