![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
what are the four categories involved in the organization of the respiratory system?
|
1) lungs and muscle pump, 2) gas exchange unit, 3) circulatory system and blood and 4) regulation of ventilation and perfusion.
|
|
|
what are the three forms of control that regulate ventilation and perfusion?
|
neuronal, hormonal and local control
|
|
|
what is internal respiration?
|
mitochondria = glucose + O2 --> CO2 + H20 + H + heat + ATP
|
|
|
what is external respiration?
|
O2 travels from the atmosphere to the lungs to the heart and vasculature to the tissues and then CO2 flows in the opposite direction depositing in the atmosphere.
|
|
|
what are the two physiological importances of gas exchange?
|
maintain O2 delivery to tissues (prevent hypoxia) and elimination of CO2 (prevent hypercapnia/acidosis)
|
|
|
What type of pattern is exhibited in the movement of gas in the body?
|
convection (brain) --> diffusion (pulmonary) --> convection (internal) --> diffusion (tissue)
ie: bulk flow, diffusion, bulk flow, diffusion. |
|
|
The primary symbols used in respiratory physiology are F, P, Q, Q(dot), R, S, V, and V(dot). what does each one stand for?
|
F- fractional concentration in dry gas
P- pressure or partial pressure Q- volume of blood Q(dot)- volume of blood per unit time R- respiratory exchange ratio S- saturation of Hb with O2 V- volume of gas V(dot)- volume of gas per unit time. |
|
|
what are the secondary symbols used for the gas phase? (IDEAL TB)
|
A- Alveolar
B-Barometric D- dead space E- expired I- inspired L- lung T- tidal |
|
|
what are the secondary symbols used for the blood phase? (CCAVVI)
|
a- arterial
c- capillary c'- end-capillary i- ideal v- venous v(line)- mixed venous |
|
|
what are static mechanics?
|
when volume is not changing, no air flow.
|
|
|
the lung consists of 6 structures, what are they?
|
airways, lung parenchyma, interstitial matrix, alveolar surfaces and pulmonary circulation
|
|
|
the chest wall consists of 4 structures, what are they?
|
structures outside of the lung that move the rib cage, diaphragm, abdominal cavity and anterior abdominal muscles.
|
|
|
what ultimately determines lung volume?
|
interaction of lung and chest wall
|
|
|
what is the static tendency of lungs?
|
to collapse due to an inward elastic recoil (for any lung volume).
|
|
|
what is the static tendency of the chest wall?
|
to expand due to an outward elastic recoil.
|
|
|
why is Ppl negative?
|
because the two membranes (visceral and parietal pleura) are pulling away from each other.
|
|
|
What is the formula for calculating alveolar pressure?
|
elastic recoil pressure + pleural pressure. ie (Pel + Ppl)
|
|
|
what is Pressure across the lung called? how is it calculated?
|
transpulmonary pressure (Pl)
alveolar pressure (Pa) - pleural pressure (Ppl) |
|
|
how do you calculate the pressure across the chest wall?
|
Pw= Ppl - Pb
|
|
|
how do you calculate the pressure for respiratory system?
|
Prs= PL + Pw
|
|
|
ultimately, based on the formulas used to determined various pressures, what is PL equivalent to?
|
Pel
|
|
|
PL is lung ______ pressure; Pel is lung _______ pressure.
|
distending; collapsing
|
|
|
what are the two ways to correct a pneumothroax?
|
1) add positive pressure in airway and 2) remove air from pleural space to re-create the negative intrapleural pressure
|
|
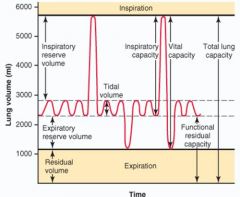
what are the two ways that Vital capacity can be calculated?
|
VC= IRV + Vt + ERV or
VC= IC + ERV |
|
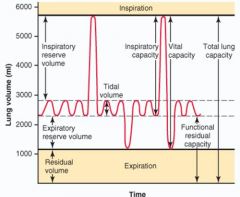
what are the two ways that Total lung capacity can be calculated?
|
TLC= VC + RV or
TLC= IC + FRC |
|
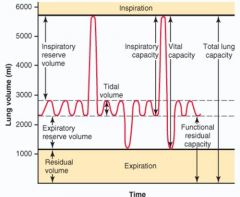
how do you calculate Functional residual capacity?
|
FRC+ ERV + RV
|
|
|
define vital capacity.
|
maximum volume of gas that can be exchanged in a single breath
|
|
|
define total lung capacity.
|
maximum volume of gas that the lungs (and airways) can contain
|
|
|
define functional residual capacity.
|
volume of gas remaining in the lings (and airways) at the end of a normal exhalation
|
|
|
define inspiratory capacity.
|
is the volume between the end of exhalation of a tidal breath and the total lung capacity
|
|
|
In and obstructive disease like emphysema, what is increased?
|
Residual volume.
|
|
|
In a restrictive disease like pulmonary fibrosis, what is decreased?
|
Total lung capacity
|

