![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
____ /____/_____ 3ct are devoid of capillaries.
|
epidermis
cornea of the eye cartilage |
|
|
|
Capillaries
is regulated by vessels with |
smooth muscle in their wa
|
|
|
|
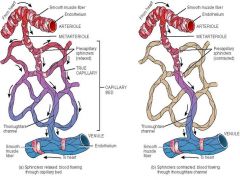
A metarteriole is a vessel that emerges from an arteriole, traverses the capillary network, and empties into a
|
venule
|
|
|
|
The proximal portion of metarterioles are surrounded by
|
scattered smooth muscle
|
|
|
|
The distal portion of a metarteriole has no smooth muscle cells and is called a
|
oughfare channel.
|
|
|
|
True capillaries emerge from arterioles or metarterioles and are not on direct flow route from a
|
arteriole to venule.
|
|
|
|
At their sites of origin, there is a ring of smooth muscle called a
|

precapillary sphincter that controls the flow of blood entering a true capillary
Pic info |
|
|
|
Capillaries
are composed of a single layer of |
endothelial cells
|
|
|
|
Capillaries
a few mitochondria rough endoplasmic reticulam Junctions of the zonula occludens type are present |
.
|
|
|
|
Capillaries
________ proximity to that of the endothelial cell. The pericytes have a great potential for transformation into other cells and thus are undifferentiated cells. |
pericytes
info |
At various locations along capillaries and small venules, there are mesenchymal cells with long cytoplasmic processes that partially surround the endothelial cells. These are called pericytes or perivascular cells.
|
|
Capillaries
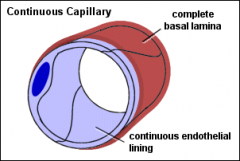
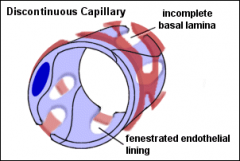
can be grouped into 3 types depending on the structure of the endothelial cell and the presence or absence of a basal lamina. |
continuous
fenestrated sinusoidal |
|
|
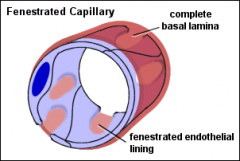
***Nm the type of structure
|
Nm the type of structure
|
Nm the type of structure
fenestrated continuous sinusoidal |
|
|
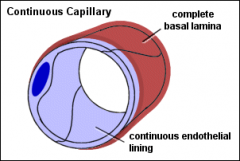
Few or no vesicles
. in the central nervous system |
Continuous capillaries
|
Continuous capillaries
In most regions there is a narrow gap between opposed cell membranes, which contains some electron dense material, but in some regions, the opposed cell membranes fuse to form tight junctions (e.g. in the central nervous system). Few or no vesicles are encountered in the continuous capillaries of the central nervous system. This feature accounts for the existence of the blood-brain barrier. |
|
|
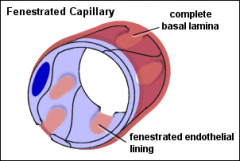
A continuous basal lamina is present.
What type of vessel |
2. Fenestrated (Type II or Visceral) Capillaries
|
|
|
|
Fenestrated capillaries are found in tissues where =
|
rapid interchange of substances
|
|
|
|
rapid interchange of substances is required
What vessel type |

Fenestrated Capillaries
|
|
|
|
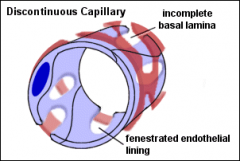
These have
1 tortuous path and a greatly enlarged diameter (30-40µm), which slows the circulation of blood. 2 endothelial cells form a discontinuous layer and are separated from one another by wide spaces. 3 multiple fenestrations (no diaphragm) in the endothelial cell wall 4 the presence around the wall of the cells with phagocytic activity (macrophages) 5 absence of a continuous basal lamina. |
3. Sinusoidal Capillaries
|
|
|
|
Sinusoidal Capillaries
have 5ct points |
1 tortuous path and a greatly enlarged diameter (30-40µm), which slows the circulation of blood.
2 endothelial cells form a discontinuous layer and are separated from one another by wide spaces. 3 multiple fenestrations (no diaphragm) in the endothelial cell wall 4 the presence around the wall of the cells with phagocytic activity (macrophages) 5 absence of a continuous basal lamina. |
|
|
|
The sinusoidal capillaries are found mainly in
|
liver
hematopoietic organs bone marrow spleen found in the adrenal cortex adenohypophysis endocrine glands |
|
|
|
Have these types of capillaries? =
liver hematopoietic organs bone marrow spleen found in the adrenal cortex adenohypophysis endocrine glands |
The sinusoidal capillaries
|
|
|
|
Functions of Capillaries
Capillaries perform at least 3ct important functions. They serve as = |
a selective permeability barrier
a synthetic and metabolic system a nonthrombogenic container for the blood. |
|
|
|
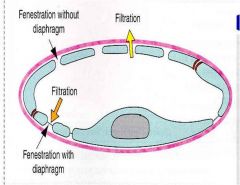
Info
Permeability of capillary walls varies with the size and charge of the permeating molecules and with the structure of the endothelial cell. |
Interpreting results of physiologic experiments, researcher have postulated the existence of two sizes of pores in the capillary walls. The smaller pores are thought to have a diameter of 9-11 nm and the larger pores a diameter of 50—70 nm.
|
Selective permeability:
Capillaries (and postcapillary venules) are often referred to as exchange vessels. These allows selective movements of small and large molecules from blood to tissues and from tissues to blood. Small hydrophilic and hydrophobic molecules e.g. oxygen, carbon dioxide, glucose, amino acids and electrolytes can diffuse or are actively transported across the plasma membrane. |
|
|
Functions of Capillaries
Three possible morphologic equivalent to these ‘physiologic pores’ are |
intercellular junctions and clefts between neighboring endothelial cells
fenestral diaphragms in fenestrated capillaries large number of pinocytotic vesicles thought to cross the endothelial cells of most capillaries. |
|
|

Functions of Capillaries
|
The intercellular junctions are now believed to be the morphologic counterpart of the small pores postulated by physiologic studies.
The large pores of the physiologist is almost certainly represented by the fenestrae or pinocytotic vesicles of endothelial cells. Small molecules, water and soluble proteins are transported by pinocytotic vesicles. Large molecules are transported through fenestrations Some specific molecules e.g. low-density lipoproteins, cholesterol, transferrins are transported via receptor mediated endocytosis which uses endothelial specific surface receptors. |
|
|
|
Clinical Note: In abnormal state such as inflammation or injection of snake or bee venom, capillary and postcapillary venular permeability is
|
greatly increased.
|
|
|
|
diapedesis
|
Leukocytes may leave the bloodstream by passing between endothelial cells and entering the tissue spaces
|
|
|
|
Opening of these junctions seems to be mediated by locally liberated pharmacologically active substances, such as =
2ct |
histamine
bradykinin |
|
|
|
Functions of Capillaries
. Metabolic Functions: Capillary endothelium 6ct |
1 Synthesizes substances that modulate blood flow and vascular resistance by secretion of vasoconstrictors (endothelin, angiotensin-converting enzyme) and vasodilators (Endothelial derived relaxation factor and nitric oxide).
2 Regulates immune response by controlling interaction of lymphocytes with endothelial surface by expression of adhesion molecules and their receptors and by the secretion of interleukin IL-1, IL-6 & IL-8. Leukocyte migration from blood to tissue is also regulated by adhesion molecules formed by endothelial cells (Selectins, integrins, CD marker molecules). 3 Synthesizes basal lamina as well as glycocalyx. 4 Converts angiotensin-I to angiotensin-II 5 Inactivates by conversion of bradykinin, serotinin, prostaglandins, norepinephrines, thrombin, etc, to biologically inert compound. 6 Modifies lipoproteins by oxidation. |
|
|
|
Functions of Capillaries
3. Nonthrombogenic Function: 4ct |
-Platelets do not normally adhere to intact endothelium.
- due, in part, to the ability of endothelial cells to release prostacyclin (prostaglandin I2) a powerful inhibitor of platelet aggregation -endothelial lining is disrupted, underlying collagen of basal lamina is stimulus for clot formation. -Anticoagulants (thrombomodulins & others) synthesized by endothelial cells. |
-Platelets do not normally adhere to an intact endothelium.
-This is due, in part, to the ability of endothelial cells to release prostacyclin (prostaglandin I2) which is a powerful inhibitor of platelet aggregation and thus thrombus (clot) formation. -If the endothelial lining is disrupted, the underlying collagen of the basal lamina is an important stimulus for clot formation. -Anticoagulants (thrombomodulins & others) are also synthesized by endothelial cells. |

