![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
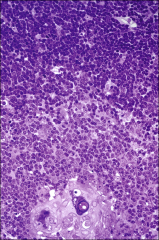
lymphoid tissues have two principal components:
|
framework of reticular fibers
(type III collagen) Free cells- Lymphocytes (chiefly), macrophages, plasma cells |
A framework of reticular fibers (type III collagen) secreted by reticular cells which are indistinguishable from fibroblasts. The epithelial reticular cells of the thymus are an exception to this generalization.
Free cells- Lymphocytes (chiefly), macrophages, and plasma cells occupy spaces between the reticular cells and fibers. Each lymphoid organ or tissue has its own special organizational features. |
|
|
Lymphatic Tissue
three categories depending upon the connective tissue covering -Unencapsulated 1 *Diffused lymphatic tissue 1 >Partially encapsulated 1 ~Encapsulated 3 |
Unencapsulated
-Free cells Diffused lymphatic tissue >Lymph nodule Partially encapsulated *Tonsils Encapsulated ~Thymus ~Lymph nodes ~Spleen |
|
|
|
Unencapsulated lymphoid tissue
|
-Free cells-
-Diffused lymphatic tissues -(MALT) mucosa assoc lymphatic tissue -Lymphocytes, -IgA = secreting plasma cells, APCs, T cells, CD4+ helper cells predominate. These cells are strategically located to intercept antigens and initiate an immune response -Lymph nodules Primary Nodule Secondary Nodule rapid proliferation contains lymphoblasts and plasmablasts) Peyer’s patches in the small intestine, or as large aggregations in lymphatic organs. |
|
|
|
Luminal antigens are captured by dome-shaped cells called =
|
M cells
present in the covering of Peyer's patches and transported to the subjacent region. |
|
|
|
M cells =
|
mucosal immunity in the intestine.
Luminal antigens are captured by dome-shaped M cells present in the covering of Peyer's patches and transported to the subjacent region. |
|
|
|
Partially encapsulated lymphoid tissue
= 4ct |
Tonsils
1-Palatine tonsils: 2. Lingual tonsils 3. Pharyngeal tonsils 4. Tubal tonsils |
|
|
|
Encapsulated lymphoid organs
|
Thymus
|
|
|
|
decribe the Thymus =
|
-bilobed
-lymphoepithelial -superior mediastinum -The thymus develops early -well developed before birth -involute -atrophy -After puberty replaced by fatty and fibrous tissues |
|
|
|
Thymus
Produces the = |
T-lymphocytes
THymus Monitors T-cell production |
It destroys the T-cells capable of attacking self
|
|
|
T/F
THymus has no Afferent lymph vessels only Efferent |
T
|
|
|
|
T-cells are released by the thymus to complete their maturation in the =
2ct |
spleen
or lymph nodes. |
|
|
|
Thymus
Each lobule is divided into two zones: |
-peripheral zone rich in lymphocytes called cortex
-central zone relatively rich in epithelial cells called the medulla. Info |
Structure
Capsule - The thymus is surrounded by a connective tissue capsule. Trabecular septa extend from the capsule to divide the gland into lobules The capsule and trabeculae contain blood vessels, efferent (but not afferent) lymphatic vessels and nerves. Each lobule is divided into two zones: |
|
|
Hormones acting on the thymus
promote the formation of T cells = 5ct |
Thymosin
thymopoietin thymulin thymic humoral factor Thyroxin Thyroxin encourages _________ causes production of ______________ _____ |
Thyroxin encourages thymulin production by epithelialreticular cells.
|
|
|
depress T cell formation in the thymus.
|
Adrenocorticosteroids
|
|
|
|
Epithelioreticular cells
do what |
provide a framework for the developing T cells.
|
|
|
|
Thymic cortical cells (besides lymphocytes):
Epithelioreticular cells of six type |
Type I
separate the thymus parenchyma from connective tissue Type II: (thymic nurse cells) Type III: form functional barrier between cortex and medulla. Like type II cells, type III cells express MHC I and MHC II molecules. |
|
|
Medulla stains less intensely than the cortex.
Three types of epithelioreticular cells are present in medulla: Type IV: are located between cortex and medulla close to type Thymic medulla |
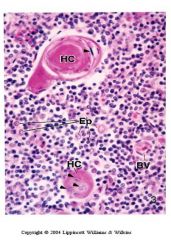
Type IV:
between cortex and medulla close to type III cells. located throughout the medulla. Type VI: thymic or Hassall’s corpuscle. have flattened nuclei. They produce thymic hormones (e.g. thymosin, thymopoietin). |

|
|
|
blood – thymic barrier.
|
present in cortex only
|
|
|
|
present in cortex only
|
blood – thymic barrier.
|
|
|
|
Lymphocytes reaching the thymic cortex are prevented from contact with antigens by a physical barrier called
|
blood – thymic barrier.
It is present in cortex only |
|
|
|
During the process of differentiation T-cells will develop subsets markers that distinguish various types of
T- cells such as = 6ct |
helper T-cells
cytotoxic T-cells gamma-delta T cells and regulatory suppresser T cells Thy-1, |
|
|
|
Thy-1, identify =
|
all subtypes of T-cells in the
thymus and in the recirculating lymphocyte pool. |
|
|
|
Most T cell development takes place in the Medulla or cortex =
|
cortex
|
|
|
|
Deep in the cortex, maturing T cells are double-positive
|
CD4+ and CD8+
and become receptive to peptide-MHC complexes. |
|
|
|
Degeorge Syndrome =
|
affects the production of functional T cells. The development of_________ is not affected in DiGeorge syndrome.
|
B cells
|
|
|
MHC class II molecules are required for the development of =
|
CD4+ T cells
|
|
|
|
MHC class I molecules are necessary for the development of
|
CD8+ T cells
|
|
|
|
T cells that recognize both
self-MHC and self-antigens -produced by thymic medullary epithelial cells under the regulation of the AIRE gene. What happens to them = |
eliminated by negative selection
|
|
|
|
T/F
Those lymphocytes that fail to meet appropriate antigens do not survive in the spleen. |
T
|
|
|
|
If the thymus of a newborn is removed, the following effects occur:
|
no formation of T-lymphocytes
decrease of lymphocytes in blood and lymph depletion thymus dependent areas of lymphoid tissues and organs. no delayed hypersensitivity reaction no graft rejection. |
|
|
|
the transcription factor Foxn1 necessary for the differentiation of thymic epithelial cells and epidermal cells
info |
.
|
|
|
|
The human autosomal disorder called autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy
(APECED) Does what = |
-autoimmune destruction of endocrine organs
-the inability to eliminate Candida yeast infection, -development of ectodermal dystrophic tissue. |
|

