![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
136 Cards in this Set
- Front
- Back

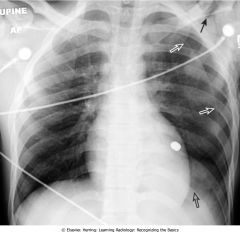
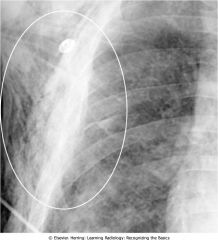
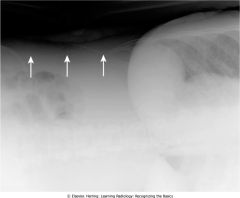
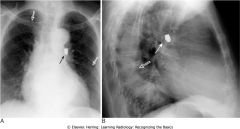
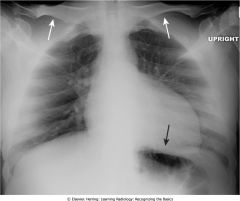
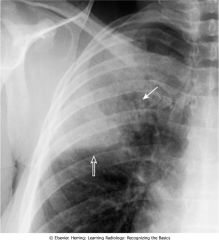
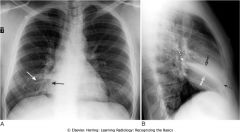
What is this?
|

Lingular Pneumonia
|
|

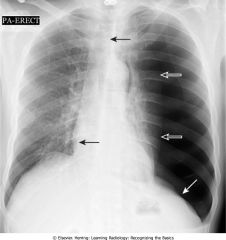
What is this?
|

Left lower lobe pneumococcal pneumonia
|
|

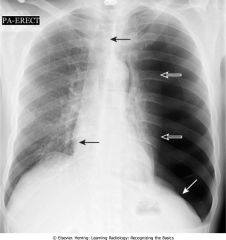
What is this?
|

Right upper lobe pneumococcal pneumonia
|
|

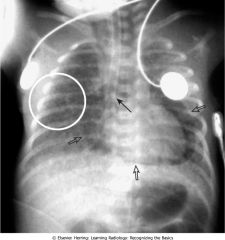
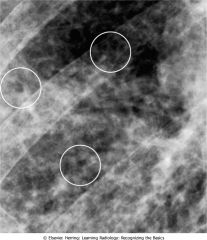
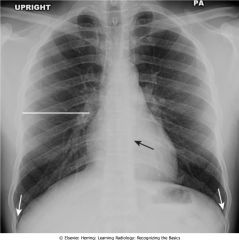
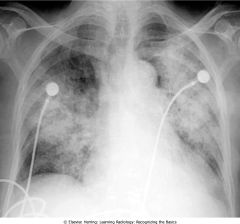
What is this?
|

Staphylococcal bronchopneumonia
|
|

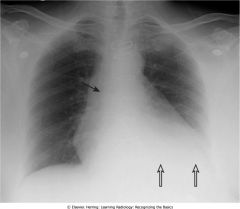
What is this?
|

Pneumocystis carinii (jiroveci) pneumonia (PCP)
|
|

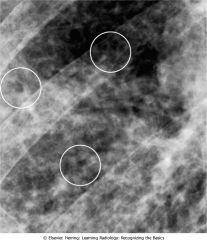
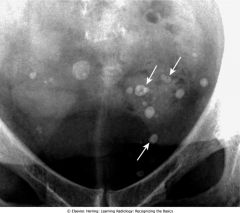
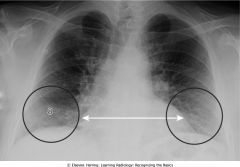
What is this?
|

Round pneumonia, seen most often in Children.
|
|

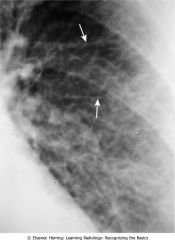
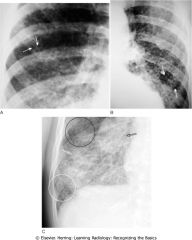
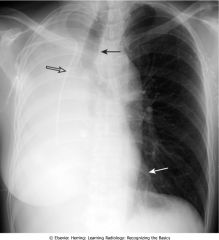
What is this?
|

Primary tuberculosis. Prominence of the left hilum is caused by left hilar adenopathy (closed white arrows). Unilateral hilar adenopathy may be the only manifestation of primary infection with Mycobacterium tuberculosis, especially in children.
|
|

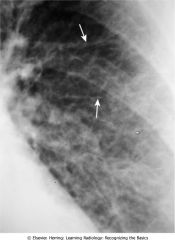
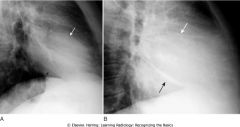
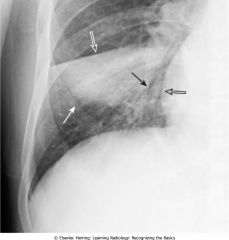
What is this?
|

Postprimary tuberculosis (reactivation tuberculosis). A cavitary pneumonia is in the right upper lobe (open black arrow). Numerous thin-walled cystic lesions (cavities) are seen throughout the airspace disease (closed white arrows). A cavitary upper lobe pneumonia is presumptively TB, until proved otherwise.
|
|

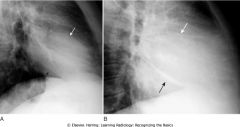
What is this?
|

Postprimary tuberculosis
|
|

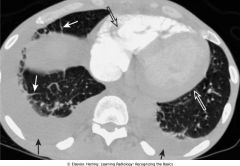
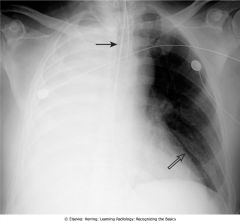
What is this?
|

Miliary tuberculosis
|
|
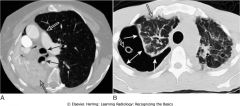
What is this?
|
Aspirate Pneumonia both lobes
|
|

What does this show?
|

Spine Sign in lateral view, a pneumonia/airway disease
|
|
What does this show?
|
Left is pneumonia, right is pneumonia after having been treated for seven days.
|
|

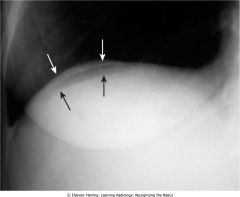
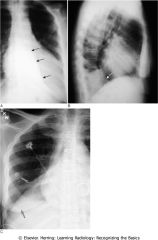
What is this?
|

Visceral pleural line in a pneumothorax
|
|

What is this?
|

Pneumothorax seen on CT
|
|

What is this?
|

Deep sulcus sign, tension pneumothorax
|
|

What is this?
|

Bullous disease, right upper lobe.Often seen in Emphysema.
|
|

What is this?
|

Bullous disease on right; pneumothorax on left.
|
|

What is on the left, and what is on the right?
|

Skin fold mimicking a pneumothorax on the left, actual pneumothorax on the right. skin fold has more of a black line compared to the white visceral line of the pneumothorax.
|
|

What is this?
|

Scapular edge mimicking a pneumothorax
|
|

What is this?
|
Pneumothorax with no shift
|
|
What is this?
|
Large left-sided tension pneumothorax. Progressive loss of air into pleural space through a one-way check-valve mechanism may cause a shift of the heart and mediastinal structures away from side of pneumothorax
|
|

What is this?
|

Bilateral pneumothoraces
|
|

What is this?
|

Pneumomediastinum seen on CT.
|
|

What is this?
|

Continuous diaphragm sign of pneumomediastinum. With pneumomediastinum, air can outline the central portion of the diaphragm beneath the heart producing an unbroken diaphragmatic contour that extends from one lateral chest wall to the other
|
|
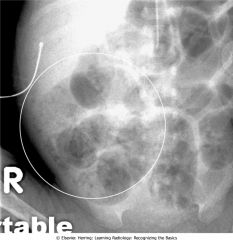
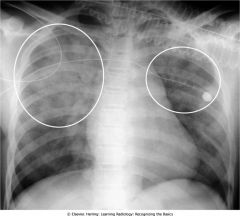
What is this?
|
Pneumopericardium, pulmonary interstitial emphysema. This is a premature infant with underlying hyaline membrane disease (respiratory distress syndrome) who is on a ventilator. A lucency surrounds the heart (open black arrows), representing air in the pericardial space. Notice how the air does not extend above the reflection of the aorta and main pulmonary artery. Pneumopericardium usually occurs from direct violation of the pericardium by trauma. In infants, it can occur from air that dissects along the bronchovascular bundles of the lungs (pulmonary interstitial emphysema). The lungs have a "bubbly" appearance (white circle) suggesting small pockets of air, a finding of pulmonary interstitial emphysema. The tip of the endotracheal tube extends too far and is in the right main bronchus (closed black arrow).
|
|
What is this?
|
Subcutaneous emphysema. Air can extend into the subcutaneous tissues of the neck, chest, and abdominal walls from the mediastinum, or it can dissect in the soft tissues from a thoracotomy drainage tube or a penetrating injury to the chest wall. Air dissecting along muscle bundles produces a characteristic comblike, striated appearance that overlies the lung (white oval). Although dramatic radiographically, subcutaneous emphysema usually produces no serious clinical effects by itself.
|
|

What is this?
|

Kerley B Lines
|
|
What is this?
|
Kerley A lines
|
|
What is this?
|
Peribronchial cuffing
|
|
What is seen on the left and on the right?
|
Left is normal fissures, right is when there is fluid in the fissures secondary to CHF.
|
|
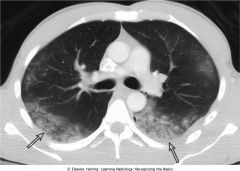
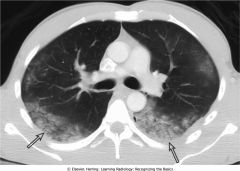
What is this?
|
Bilateral pleural effusions and Kerley B lines on CT. Axial CT scan of the chest following intravenous injection of contrast material. Note that the right side of the heart is opacified (open black arrow) but the contrast agent has not yet passed through the lungs a sufficient number of times to fully opacify the left side of the heart (open white arrow). There are bilateral pleural effusions present and they layer posteriorly because the patient is being scanned supine (closed black arrows). The thickened interlobular septa (closed white arrows) are Kerley B lines.
|
|

What is this?
|

Bat-wing pattern of pulmonary edema
|
|

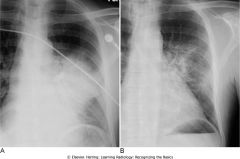
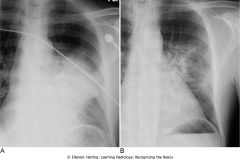
What is this showing?
|

Rapid clearing of pulmonary edema. Pt has pulmonary edema on left, and four days later is recovering on right.
|
|

What is the image on the left, and what is the image on the right?
|

Pulmonary interstitial (left) versus pulmonary alveolar edema (right)
|
|

What is this?
|
Unilateral airspace disease affects the entire right lung. In addition, a chest tube (closed black arrow) is seen on the same side. The chest tube was inserted for a large, right-sided, tension pneumothorax that was rapidly re-expanded. Re-expansion pulmonary edema results from the overly rapid expansion of a lung that has typically been chronically collapsed by pneumothorax or a large pleural effusion. Its exact cause is not known. In general, unilateral pulmonary edema can occur either because of an abnormality on the same side as the pulmonary edema (e.g., prolonged positioning with the affected side dependent) or an abnormality on the opposite side (e.g., large pulmonary embolus occluding flow to the opposite lung).
|
|

What is this?
|

Noncardiogenic pulmonary edema. Bilateral airspace disease primarily affects the upper lobes in this patient (closed black arrows). There is no evidence of pleural fluid (white circles). In general, noncardiogenic pulmonary edema is less likely to demonstrate pleural effusions and Kerley B lines, more likely to demonstrate a normal pulmonary capillary wedge pressure (PCWP) of less than 12 mm Hg, and more likely to be associated with a normal-sized heart than cardiogenic pulmonary edema. This patient had taken an overdose of heroin.
|
|

What does this show?
|

Normal Supine Abdomen
|
|

What is this showing?
|

Normal Prone Abdomen
|
|

What is this showing?
|

Normal colonic distension with barium and gas enema.
|
|

What does this show the appearance of?
|

Stool
|
|

What does this image show?
|

aerophagia - swallowing excessive amounts of air.
|
|

What does this show?
|
Normal upright abdomen. There are two things to look for on an upright view of the abdomen: air-fluid levels and free intraperitoneal air. Normally, there is an air-fluid level in the stomach (closed black arrow). There may be short, air-fluid levels in two or three nondilated loops of small bowel (open black arrow). There are usually very few or no air-fluid levels in the colon (closed white arrow). Free air, if present, should be visible just below the hemidiaphragm (dotted black arrow) and would be easier to recognize on the right than the left, because the stomach bubble is usually present on the left.
|
|

What does this show?
|

Large bowel
|
|
What does this show?
|
Normal left lateral decubitus view of the abdomen. For a left lateral decubitus view, the patient lies on his or her left side on the examining table and an exposure is made with a horizontal x-ray beam (parallel to the floor). This is done so that any "free air" will distribute itself at the highest part of the abdominal cavity, which will be the patient's right side. If present, free air should be easily visible as a black crescent over the outside edge of the liver (closed white arrows), a location in which there is normally no bowel gas present. There is no free air in this patient.
|
|
What does this show?
|

Phleboliths
|
|

What does this show?
|

Calcification of the rib cartilages (white circle) occurs with advancing age and, although not a true abdominal calcification, can sometimes be confused for calculi when it overlays the kidney or region of the gallbladder
|
|

What does this show?
|
Riedel's lobe of the liver. Occasionally, a tongue-like projection of the right lobe of the liver may extend to the iliac crest, especially in females. This is called a Riedel's lobe (closed black arrows) and is normal.
|
|

What is this?
|
Hepatomegaly. Sometimes, the liver can become so enlarged it will be obvious even on conventional radiographs. An enlarged liver might be suggested from conventional radiographs if there is displacement of all bowel loops from the right upper quadrant down to the iliac crest and across the midline (closed white arrows), such as in this patient with cirrhosis.
|
|

What is this showing?
|
Splenomegaly. The spleen is normally about 12 cm in length and usually does not project below the 12th posterior rib. If the spleen (closed white arrows) projects well below the 12th posterior rib (closed black arrow) or displaces the stomach bubble toward or across the midline, the spleen is probably enlarged, as it is in this patient with leukemia.
|
|

What does this show?
|
Position of the kidneys. This image is from an intravenous urogram (aka intravenous pyelogram [IVP]) in which the patient receives an intravenous injection of iodinated contrast material that is excreted by the kidneys. Both kidney outlines (closed white arrows), ureters (closed black arrows), and urinary bladder (open black arrow) can be seen. Other images of the kidneys, including oblique views, were often obtained to visualize the entire contour of the kidney. IVPs have largely been replaced by CT scans and CT urograms. The liver (open white arrow) depresses the right kidney more inferiorly than the left kidney.
|
|

What does this show?
|

Enlarged kidneys. Soft tissue masses or organomegaly can be diagnosed from a conventional radiograph either by visualizing the edge of the mass if there is fat or air surrounding it or by displacement of bowel, as in this case. Note that even though you don't see the outline of the right kidney, there is no bowel gas on the right side of the abdomen (closed white arrow),
|
|
What does this show?
|
Normal Urinary Bladder
|
|

What does each image show?
|

distended bladder (left), large uterus (right)
|
|
|
The following means what?
Air in Rectum or Sigmoid - Yes Air in Small Bowel - Yes, 1-2 loops Air in Large Bowel - Rectum and/or sigmoid |
Normal Bowel
|
|
|
The following means what?
Air in Rectum or Sigmoid - Yes Air in Small Bowel - 2-3 dilated loops Air in Large Bowel - Rectum and/or sigmoid |
Localized ileus
|
|
|
The following means what?
Air in Rectum or Sigmoid - Yes Air in Small Bowel - Multiple dilated loops Air in Large Bowel - Yes, dilated |
Generalized ileus
|
|
|
The following means what?
Air in Rectum or Sigmoid - No Air in Small Bowel - Multiple dilated loops Air in Large Bowel - No |
Small bowel obstruction
|
|
|
The following means what?
Air in Rectum or Sigmoid - No Air in Small Bowel - None unless ileocecal valve incompetent Air in Large Bowel - Yes, dilated |
Large bowel obstruction
|
|
|
Site of dilated loops
Right upper quadrant |
Cholecystitis
|
|
|
Site of dilated loops
Left upper quadrant |
Pancreatitis
|
|
|
Site of dilated loops
Right lower quadrant |
Appendicitis
|
|
|
Site of dilated loops
Left lower quadrant |
Diverticulitis
|
|
|
Site of dilated loops
Mid-abdomen |
Ulcer or kidney/ureteral calculus
|
|

What does this show?
|

sentinal loops from pancreatitis
|
|
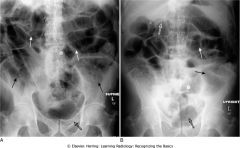
What is this?
|
Generalized adynamic ileus, supine (A) and erect (B) abdomen. Dilated loops of large (closed black arrows) and small bowel (closed white arrows) are seen down to and including the rectum (open black arrows). The upright image (B) shows surgical clips (open white arrow) just to the right of the upper lumbar spine. The patient had undergone abdominal surgery the day before.
|
|

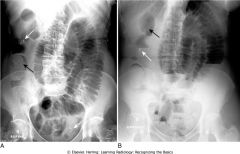
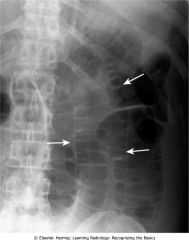
What is this?
|
Step-ladder appearance of obstructed small bowel. As they begin to dilate, small bowel loops stack up, forming a step-ladder appearance usually beginning in the left upper quadrant and proceeding, depending on how distal the small bowel obstruction is, to the right lower quadrant (closed white arrows). The more proximal the small bowel obstruction (e.g., proximal jejunum), the fewer dilated loops there will be; the more distal the obstruction (e.g., at the ileocecal valve), the greater the number of dilated small bowel loops. This was a distal small bowel obstruction caused by a carcinoma of the colon, which obstructed the ileocecal valve.
|
|

What is this?
|

Mechanical small bowel obstruction
|
|
What does this show?
|
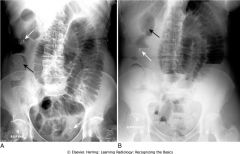
Partial small bowel obstruction, supine (A) and upright (B) views
|
|

What is this?
|
Mechanical large bowel obstruction. The entire colon is dilated to a cut-off point in the distal descending colon (closed white arrow), the site of this patient's obstructing carcinoma of the colon. Some gas has passed backward through an incompetent ileocecal valve and outlines a dilated ileum (closed black arrow). Notice that the large bowel is disproportionately dilated compared to the small bowel, a finding of large bowel obstruction. This patient had an obstructing carcinoma at the sigmocolic junction.
|
|

What does this show?
|
Dilated cecum in large bowel obstruction of the descending colon. Although the point of this patient's large bowel obstruction is the mid-descending colon (open white arrow), notice that the cecum is the most dilated loop of colon (closed white arrow). With a mechanical obstruction, the loop(s) that will become the most dilated will be either the loop of bowel with the largest resting diameter before the onset of the obstruction (e.g., the cecum in the large bowel) or the loop(s) of bowel just proximal to the obstruction. This patient had an obstructing carcinoma of the mid-descending colon.
|
|

What is this showing?
|
Large bowel obstruction masquerading as a small bowel obstruction. There are air-filled and dilated loops of small bowel (closed white arrows) in this patient who actually had a mechanical large bowel obstruction from a carcinoma of the mid-descending colon. The pressure in the colon was sufficient to open the ileocecal valve, which then allowed much of the gas in the colon to decompress backward into the small bowel. The cecum still contains air (open white arrow) and is dilated, a clue that this is really a large bowel obstruction. Abdominal CT or a contrast enema can resolve the question of whether the large or small bowel is obstructed.
|
|
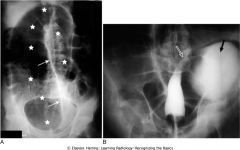
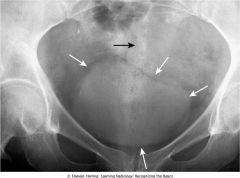
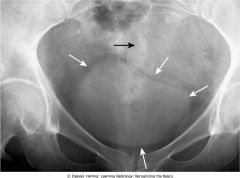
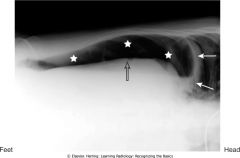
What is this?
|
Sigmoid volvulus. Supine abdominal film (A) shows a massively dilated sigmoid (white stars) with the wall between the twisted loops (closed white arrows) forming a line that points toward the right upper quadrant, findings characteristic of a sigmoid volvulus. B, One image from a barium enema shows a smoothly tapered segment of sigmoid colon likened to a bird's beak, a finding characteristic of a sigmoid volvulus (open white arrow). Some barium has entered the dilated volvulated sigmoid (closed black arrow).
|
|

What is this?
|
Ogilvie's syndrome. Ogilvie's syndrome (acute intestinal pseudo-obstruction) may occur in elderly individuals who are usually already hospitalized or at chronic bedrest. Drugs with anticholinergic effects may cause or exacerbate the condition. The syndrome is characterized by a loss of peristalsis, resulting in sometimes massive dilatation of the entire colon, resembling a large bowel obstruction, as in this patient. Treatment is pharmacologic stimulation of the bowel.
|
|
What is this showing?
|
Free air beneath right hemidiaphragm. Close-up of the right upper quadrant from an upright chest radiograph shows a thin crescent of air between the hemidiaphragm (closed white arrows) and the dome of the liver (closed black arrows) representing free intraperitoneal air. The patient had undergone abdominal surgery 5 days earlier. Free air can remain for up to 7 days after surgery in an adult, but serial studies should demonstrate a progressively decreasing amount of air.
|
|

What does this show?
|
Large amount of free air. Upright view of the chest demonstrates a large amount of free air (white stars) beneath each hemidiaphragm (closed white arrows). The top of the liver (closed black arrow) is made visible by the air above it. The patient had a perforated gastric ulcer.
|
|

What does the left show, what does the right show?
|
Normal left hemidiaphragm (A) and free air under hemidiaphragm (B). A, Close-up of the left upper quadrant demonstrates the difficulty in recognizing free air beneath the normal left hemidiaphragm (closed white arrows) because of the normal location of gas-containing structures such as the stomach (black star) and splenic flexure (white stars) in that location. B, A crescentic lucency beneath the left hemidiaphragm represents free air in another patient. It is easier to recognize free air beneath the right hemidiaphragm because there is usually no air interposed between the liver and the right hemidiaphragm.
|
|
What is this showing?
|
Left lateral decubitus view showing free air. Close-up of the right upper quadrant in a patient lying on their left side in the left lateral decubitus position shows a crescent of air (white stars) above the outer edge of the liver (open black arrow), beneath the right hemidiaphragm (closed white arrows). If the patient is unable to stand or sit for an upright view of the abdomen, a left lateral decubitus view can substitute. The x-ray beam must be directed horizontally.
|
|

What does this show?
|
Chilaiditi's syndrome. Close-up of the right hemidiaphragm on a conventional chest radiograph (A) and an axial CT scan at the level of the diaphragm (B) both demonstrate air beneath the diaphragm that could be mistaken for free air (open black arrows). Careful evaluation of this air demonstrates several haustral folds (closed white arrows) that traverse the air, indicating this is a loop of colon interposed between the liver and the diaphragm (Chilaiditi's syndrome) rather than free air. Most patients with this syndrome are completely asymptomatic, and it is only important as a potential diagnostic pitfall.
|
|

What does this show?
|
Rigler's sign. When air fills the peritoneal cavity, both sides of the bowel wall will be outlined by air, making the wall of the bowel visible as a discrete line (closed white arrows). This is known as Rigler's sign and indicates the presence of a pneumoperitoneum.
|
|
What does this show?
|
Overlapping loops mimicking free air. Don't let overlapping loops of dilated small bowel (closed white arrows) fool you into thinking you are seeing both sides of the bowel wall because of free air. If there is doubt about the presence of free air, confirmation may be obtained through an upright or left lateral decubitus view of the abdomen or a CT scan of the abdomen.
|
|

What is this?
|
Falciform ligament sign. Free intraperitoneal air may surround the normally invisible falciform ligament on the anterior edge of the liver causing that thin soft tissue structure to become visible (closed black arrows) just to the right of the upper lumbar spine. Notice also that both sides of the stomach wall are visible (Rigler's sign) (open white arrows) in this patient with a large pneumoperitoneum from a perforated gastric ulcer. The thick white bands (closed white arrows) represent folds of skin on the patient's back.
|
|

What is this?
|
Extraperitoneal air seen on CT. Air is seen in the retroperitoneum (open white arrow) on this axial CT scan of the upper abdomen. Air outlines the inferior vena cava (closed black arrow) and the aorta (closed white arrow). Unlike free air, extraperitoneal air is streaky, relatively fixed in position, and outlines extraperitoneal structures such as the vena cava, aorta, psoas muscles, and kidneys.
|
|

What is this?
|
Pneumatosis seen in profile. Close-up of the right lower quadrant in an infant demonstrates a thin curvilinear lucency that parallels the lumen of the adjacent bowel (closed black arrows), an appearance characteristic of gas in the bowel wall seen in profile. In infants, the most common cause for this finding is necrotizing enterocolitis, a disease found mostly in premature infants in which the terminal ileum is most affected. Pneumatosis intestinalis is pathognomonic for necrotizing enterocolitis in infants.
|
|
What is this?
|
Pneumatosis seen en face. Supine abdominal study of another infant shows multiple faint, mottled lucencies in the right lower quadrant (white circle), which is the appearance of pneumatosis intestinales when seen en face. The density has the same appearance as air mixed with stool, but can be distinguished from stool because it occurs in areas stool might not be expected and it does not change over time. This infant also had necrotizing enterocolitis.
|
|

What is this?
|
Pneumatosis cystoides intestinalis. Axial CT scan of the upper abdomen windowed for lung technique shows a cluster of air-containing cysts (closed white arrows) associated with the left colon, characteristic of pneumatosis cystoides intestinales, a rare but benign condition in which air-containing cysts form in the submucosa or serosa of the bowel.
|
|

What is this?
|
Necrosis of bowel from mesenteric ischemia. Axial CT image of the pelvis demonstrates multiple loops of bowel with punctate collections of air throughout their walls consistent with pneumatosis (closed white arrows). The patient had widespread ischemia of bowel from mesenteric vascular disease. Pneumatosis which results from bowel necrosis is an ominous sign.
|
|

What does this show?
|
Portal venous gas. Numerous small black branching structures are visible over the periphery of the liver (white circle). This is air in the portal venous system, a finding most often associated with necrotizing enterocolitis in infants. Once thought to be an ominous prognostic sign, it now is considered less grave. Unlike air in the biliary system, this air is peripheral rather than central and has numerous branching structures rather than the few tubular structures seen with pneumobilia.
|
|

What is this?
|
Air in the biliary tree. Frontal view of the upper abdomen from an upper gastrointestinal series demonstrates several air-containing tubular structures over the central portion of the liver consistent with air in the biliary system (white circle). There is also barium in the gallbladder (closed white arrow). This patient had a history of a prior sphincterotomy for gallstones so that reflux of air and barium into the biliary system would be expected.
|
|

What does this show?
|
Gallstone ileus. The three key findings of gallstone ileus are present on this study. A, Axial CT scan of the upper abdomen shows air in the lumen of the gallbladder (closed black arrow) and dilated small bowel (open white arrows) consistent with a mechanical small bowel obstruction. At a lower level, another axial CT scan of the abdomen (B) shows a large calcified gallstone inside the small bowel (closed white arrow). The gallstone had eroded through the wall of the gallbladder into the duodenum and then began a journey down the small bowel before becoming impacted and producing obstruction.
|
|
What is this?
|
Bullet in the chest. The dense (white) metallic foreign body in the region of the aortopulmonary window resembles a bullet because it is a bullet (black and white closed arrows). It is much denser (whiter) than the bones, represented by the ribs, clavicles, and spine (open white arrows). Two views at 90° angles to each other, such as these frontal (A) and lateral (B) chest radiographs, are called orthogonal views (see Chapter 2). With only one view, it would be impossible to know the location of the bullet. Orthogonal views are used throughout conventional radiography to localize structures in all parts of the body.
|
|

What is this?
|
Gallstones. Multiple laminar, calcific densities (whiter than surrounding soft tissue) are seen in the right upper quadrant (closed white arrow) with flattened edges where they rub against each other in the lumen of the gallbladder (perhaps to stay warm). These are called faceted gallstones. The numerous small opacities (open white arrow) represent radiopaque metallic sutures from prior surgery.
|
|

What is this?
|
Right lower lobe bronchogenic carcinoma. There is a nearly spherical mass in the right middle lobe of the lung (white closed arrows) seen on the frontal (A) and lateral (B) radiographs of this patient. Because the mass is nearly spherical, it has relatively the same shape when viewed en face and in profile.
|
|

What is this?
|
Coin in the esophagus. Both the frontal (A) and the lateral (B) images of this child's upper thorax demonstrate a radiopaque (white) metallic density in the region of the upper esophagus (white closed arrows). The child swallowed a quarter, which is temporarily lodged in the esophagus just above the aortic arch. Notice how different the coin looks when viewed en face in (A) where it is seen as a circle and in profile (B) where it is seen on end.
|
|
What does this show?
|
Well-exposed frontal view of a normal chest. Notice how the spine (closed black arrow) is just visible through the heart shadow. Both the right and left lateral costophrenic angles are sharply and acutely angled (closed white arrows). The white line demarcates the approximate level of the minor or horizontal fissure. There is no minor fissure on the left side. The major or oblique fissures are oriented in a diagonal plane such that they are generally not visible on the frontal radiograph.
|
|
What does this show?
|
Underpenetrated frontal chest radiograph. The spine (closed black arrow) is not visible through the cardiac shadow. The left hemidiaphragm is also not visible (open black arrows) and the degree of underpenetration makes it impossible to differentiate between actual disease at the left base versus nonvisualization of the left hemidiaphragm from underpenetration. A lateral radiograph of the chest would help to differentiate between artifact of technique and true disease.
|
|

What does this show?
|
Overpenetrated frontal chest radiograph. The overpenetration makes lung markings difficult to see, mimicking some of the findings in emphysema or possibly suggesting a pneumothorax. How lucent (dark) the lungs appear on a radiograph is a poor way of evaluating for the presence of emphysema because of artifacts introduced by technique. In emphysema, the lungs are frequently hyperinflated and the diaphragm flattened (see Chapter 14). In order to diagnose a pneumothorax, you should see the pleural white line
|
|
Secondary syphilis
|
disseminated disease:
maculopapular rash (palms, soles) lymphadenopathy condylomata lata |
|

What do these three show?
|
How to evaluate for rotation. A, Close-up view of the heads of the clavicles demonstrates that each (white arrows) is about equidistant from the spinous process of the vertebral body between them (black arrow). This indicates the patient is not rotated. B, Close-up view of the heads of the clavicles in a patient rotated toward his own right (remember that you are viewing the study as if the patient were facing you). The spinous process (black arrow) is much closer to the left clavicular head (open white arrow) than it is to the right clavicular head (closed white arrow). C, Close-up view of the heads of the clavicles in a patient rotated toward his own left. The spinous process (black arrow) is much closer to the right clavicular head (closed white arrow) than it is to the left (open white arrow).
|
|

What does this show?
|
Distorted appearance due to severe rotation. Frontal chest radiograph of a patient markedly rotated toward her own right. Notice how the left hemidiaphragm, being farther from the cassette than the right hemidiaphragm because of the rotation, appears higher than it normally would (closed white arrow). The heart and the trachea (closed black arrow) appear displaced into the right hemithorax because of the rotation.
|
|
What kind of radiograph is this?
|
Apical lordotic chest radiograph. An apical lordotic view of the chest is now most frequently obtained inadvertently in patients who are semirecumbent at the time of the study. Notice how the clavicles are projected above the first ribs and their usual "S" shape is now straight (closed white arrows). The lordotic view also distorts the shape of the heart and produces spurious obscuration of the left hemidiaphragm (closed black arrow). Unless the artifacts of technique are understood, these findings could be mistaken for disease that doesn't exist.
|
|

What is this?
|
Anterior mediastinal adenopathy. Left lateral view of the chest demonstrates soft tissue filling in the normal clear space behind the sternum (closed black arrows). This represents anterior mediastinal lymphadenopathy in a patient with lymphoma. Adenopathy is probably the most frequent reason the retrosternal clear space is obscured. Thymoma, teratoma, and substernal thyroid enlargement also can produce anterior mediastinal masses but do not usually produce exactly this appearance.
|
|

What is this?
|
Arms obscure retrosternal clear space. In this example, the patient was not able to hold her arms over her head for the lateral chest examination, as patients are instructed to do in order to eliminate the shadows of the arms from overlapping the lateral chest. The humeri are clearly visible (closed white arrows) so even though the soft tissue of the patient's arms appears to fill in the retrosternal clear space (closed black arrows), this should not be mistaken for an abnormality such as anterior mediastinal adenopathy
|
|

What is this?
|
Hilar mass on lateral radiograph. Left lateral view of the chest shows a discrete mass in the region of the hila (closed black arrows). Normally, the hila do not cast a shadow that is easily detectable on the lateral projection. This patient had bilateral hilar adenopathy from sarcoidosis but any cause of hilar adenopathy or a mass in the hilum would have a similar appearance.
|
|

What is this?
|
Fluid in the major fissures. Left lateral view of the chest shows thickening of both the right and left major fissures (closed white arrows). This patient was in congestive heart failure and this thickening represents fluid in the fissures. Normally, the fissures are either invisible or, if visible, they are fine, white lines of uniform thickness no larger than a line made with the point of a sharpened pencil. The major or oblique fissure runs from the level of the fifth thoracic vertebral body to a point on the anterior diaphragm about 2 cm behind the sternum. Notice the increased interstitial markings that are visible throughout the lungs and are due to fluid in the interstitial tissues of the lung.
|
|

What is this?
|
Osteoporotic compression fracture and degenerative disk disease. Don't forget to look at the thoracic spine when studying the lateral chest radiograph for valuable information about a host of systemic diseases (see Chapter 24). In this study, there is loss of stature of the eighth thoracic vertebral body due to osteoporosis (open white arrow). Compression fractures frequently involve the superior end plate first. There are small osteophytes present at multiple levels from degenerative disk disease (closed white arrows).
|
|

What is this?
|
Blunting of the posterior costophrenic sulcus by a small pleural effusion. Left lateral view of the chest shows fluid blunting the posterior costophrenic sulcus (closed white arrow). The other posterior costophrenic angle (closed black arrow) is sharp. The pleural effusion is on the right side because the hemidiaphragm involved can be traced anteriorly farther forward (open black arrow) than the other hemidiaphragm (the left), which is normally silhouetted by the heart and not visible anteriorly.
|
|
What is this?
|
Diffuse airspace disease of pulmonary alveolar edema. There are opacities throughout both lungs, primarily involving the upper lobes (white circles), that can be described as fluffy, hazy, or cloudlike and are confluent and poorly marginated, all pointing to airspace disease. This is an typical example of pulmonary alveolar edema (due to a heroin overdose in this patient).
|
|
What is this?
|
Right middle lobe pneumonia. There is an area of increased opacification in the right lower lung field that has indistinct inferior margins (closed white arrow) and several black branching structures that represent air bronchograms (closed black arrow). These findings are consistent with airspace disease. Notice the sharp superior border of the disease (open white arrow), a sign that the airspace disease is abutting the minor fissure and establishing its location in the right middle lobe. The right heart border (open black arrow) is still visible because the disease involves a segment that is not in anatomic contact with the right heart border.
|
|

What is this?
|
Air bronchograms demonstrated on CT scan. There are numerous black, branching structures (closed black arrows) representing air that is now visible inside the bronchi because the surrounding airspaces are filled with inflammatory exudate in this patient with an obstructive pneumonia from a bronchogenic carcinoma. Normally, on conventional radiographs, air inside bronchi is not visible because the bronchial walls are very thin, they contain air, and they are surrounded by air.
|
|
What is this?
|
Silhouette sign, right middle lobe pneumonia. Fluffy, indistinctly marginated airspace disease is seen (A) to the right of the heart (open white arrow), which partially obscures a small margin of the right heart border (closed black arrow). This is called the silhouette sign and establishes that the disease (1) is in contact with the right heart border (which lies anteriorly in the chest) and (2) that the disease is the same radiographic density as the heart (fluid or soft tissue). Pneumonia fills the airspaces with an inflammatory exudate of fluid density. B, The area of the consolidation is indeed anterior, located in the right middle lobe, which is bound by the major fissure below (closed white arrow) and the minor fissure above (open black arrow).
|
|
What is this?
|
Right upper lobe pneumococcal pneumonia. Close-up view of the right upper lobe demonstrates confluent airspace disease with several air bronchograms (closed white arrow). The inferior margin of the pneumonia is more sharply demarcated because it is in contact with the minor fissure (open white arrow). This patient had Streptococcus pneumoniae cultured from the sputum.
|
|
What is this?
|
Acute pulmonary alveolar edema. Fluffy, bilateral, perihilar airspace disease with indistinct margins sometimes described as a bat-wing or angel-wing configuration. No air bronchograms are present. The heart is enlarged. This represents pulmonary alveolar edema secondary to congestive heart failure.
|
|

H. ducreyi
|
painful chancre
("do cry" = ducreyi) |
|
What is this?
|
A, Interstitial lung disease, predominantly reticular. Close-up view of the right upper lung field shows a prominence of the markings that, on close inspection, represents a diffuse network of interwoven lines. Between the well-demarcated lines are numerous small areas of normal lung (closed white arrows). This pattern is characteristic of reticular interstitial disease. The patient had sarcoidosis. B, Interstitial lung disease, predominantly nodular. Close-up view of the left upper lung field demonstrates a prominence of the lung markings that has a small, nodular (dot-like) appearance. Interspersed between the sharply demarcated nodules are multiple zones of normal-appearing lung (closed white arrows). This pattern is typical for nodular interstitial lung disease, sometimes referred to as micronodular lung disease because of the small size of the nodules. The patient was known to have thyroid carcinoma, and these nodules represent innumerable small metastatic foci in the lungs. C, Interstitial disease of the lung, reticulonodular. Most interstitial diseases of the lung have a mixture of both a reticular (lines) and nodular (dots) pattern, as does this case, which is a close-up view of the right lower lobe in a patient with sarcoidosis. The disease in the white circle consists predominantly of an intersecting, lacy network of lines. There are also a few small nodules seen (black circle). The inferior margin of markedly enlarged hilar lymph nodes is seen (open black arrow). Notice how a portion of this disease appears confluent, like airspace disease (open white arrow). Always look at the peripheral margins of parenchymal lung disease to best determine the nature of the "packets" of abnormality and to help in differentiating airspace disease from interstitial disease.
|
|

What is this?
|
Silicosis. The patient was a sandblaster with a long-term exposure to silica particles. Innumerable, small nodular densities are seen on the frontal radiograph most prominent in the upper lobes (white circle). The appearance and distribution are characteristic of silicosis. More confluent disease in this patient's right upper lobe includes cavity formation (closed black arrow). On further study, the disease in the right upper lobe was proved to represent tuberculosis. Silicosis is a predisposing factor in tuberculosis.
|
|

What is this?
|
Blood vessels on-end versus nodules. Blood vessels seen on-end (A) may mimic small pulmonary nodules (B). To differentiate the two, always look for a "line" (open white arrows) leading up to the "dot" (closed white arrows). If one is present, the chances are good that you are looking at a vessel on-end. The "line" is the feeding vessel. Also, blood vessels seen on-end in one projection will "disappear" (they will no longer be on-end) on the orthogonal view. Nodules will appear the same on both orthogonal views. Finally, nodules (B) may be disproportionately large compared to the size of other blood vessels in the region (closed black arrows). These nodules are residual calcifications from a previous episode of varicella pneumonia.
|
|

What is this?
|
Pulmonary interstitial edema secondary to congestive heart failure. A diffuse accentuation of the pulmonary interstitial markings is evident in the frontal radiograph (A). A close-up view of another patient with the same disease (B) demonstrates multiple Kerley B lines (black circle) representing fluid in thickened interlobular septa. There is a network of crossing lines in the lung (white circle) that represent Kerley A lines. Peribronchial cuffing is present (closed white arrow) representing bronchial walls that are now visible because they are fluid-filled and dilated.
|
|

What is this?
|
Idiopathic pulmonary fibrosis. Idiopathic pulmonary fibrosis probably represents a spectrum of disease that may begin as desquamative interstitial pneumonia and lead to the findings here of usual interstitial pneumonia (UIP). A, Coarse reticular interstitial markings represent fibrosis, predominantly at the lung bases (closed black arrows). A high-resolution CT scan of the chest (B) shows abnormalities at the lung bases, peripherally in a subpleural location, the typical distribution for UIP. There are small cystic spaces called honeycombing (white circles) with hazy densities called ground-glass opacities (closed white arrows).
|
|

What is this?
|
Rheumatoid lung. Prominent markings at both lung bases have a predominantly reticular appearance (closed white arrows). Bibasilar interstitial disease can be found in numerous diseases including bronchiectasis, asbestosis, desquamative interstitial pneumonia (DIP), scleroderma, and sickle cell disease. This patient was known to have rheumatoid arthritis. Pleural effusion is the most common manifestation of rheumatoid lung disease. Pulmonary fibrosis, usually diffuse but more prominent at the bases, is seen second most commonly.
|
|

What is this?
|
Adenocarcinoma, right upper lobe. A mass is evident in the right upper lobe (closed white arrow). Its margin is slightly lobulated and is indistinct along the superolateral border (closed black arrow). Also, prominence of the soft tissues in the right paratracheal region (open white arrow) suggests associated adenopathy. CT scan of the chest confirmed the presence of the mass and demonstrated paratracheal and right hilar adenopathy. The mass was biopsied and was an adenocarcinoma, primary to the lung. Adenocarcinoma of the lung most commonly presents as a peripheral nodule.
|
|

What does this show?
|
Metastases to the lung. Frontal radiograph of the chest (A) demonstrates multiple nodules of varying size throughout both lungs (closed black arrows). The diagnosis of exclusion, whenever multiple nodules are found in the lungs, is metastatic disease. On a chest CT scan in another patient (B), there are multiple nodules of varying sizes with irregular margins seen in both lungs (closed white arrows). The patient in A had a breast carcinoma, and the patient in B had colorectal carcinoma. These nodules are sometimes called cannon-ball metastases seen with hematogenous spread of malignancy to the lungs.
|
|

What does this show?
|
Sarcoidosis. A frontal radiograph of the chest reveals bilateral hilar and right paratracheal adenopathy (closed white arrows), a classical distribution for the adenopathy in sarcoidosis. In addition, the patient has diffuse, bilateral interstitial lung disease that is reticulonodular in nature (see close-up view of this same patient in Fig. 4-8C). In some patients with this stage of disease, the adenopathy regresses while the interstitial disease remains. In the overwhelming majority of patients with sarcoid, the disease completely resolves.
|
|
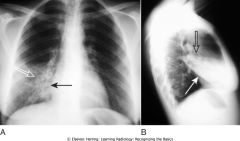
What do these two show?
|
Obstructive atelectasis versus a pneumothorax. Two different causes of lung collapse and the difference in their radiologic appearance. A, There is atelectasis of the entire right lung (open black arrow) from an obstructing endobronchial lesion. The visceral and parietal pleurae remain in contact with each other and other mobile structures in the mediastinum, such as the right and left main bronchi (closed black arrows), shift toward the atlectasis. The left lung overexpands and crosses the midline (open white arrow). B, This patient has a large right-sided pneumothorax. Air (double white arrow) interposes between the visceral (closed white arrows) and parietal pleurae, causing the lung to undergo passive atelectasis (open black arrow). There is a chest tube in the right hemithorax (open white arrow) that had been removed from suction.
|
|
What does this show?
|
Right middle lobe atelectasis. Frontal (A) and lateral (B) views of the chest show an area of increased density (closed white arrow), which is silhouetting the normal right heart border (closed black arrow) indicating its anterior location in the right middle lobe. On the lateral view (B), the minor fissure is displaced downward (open black arrow) and the major fissure is displaced upward (open white arrow). Note the anterior location of the middle lobe and the fan-shaped appearance of the atelectatic lobe with its apex at the hilum (dotted white arrow) and its base adherent to the chest wall (dotted black arrow).
|
|

What is this?
|
Right upper lobe atelectasis. A fan-shaped area of increased density is seen on the frontal projection (A) representing the airless right upper lobe (open black arrow). The minor fissure is displaced upward (closed white arrow). The trachea is shifted to the right (closed black arrow). The lateral (B) demonstrates a similar wedge-shaped density near the apex of the lung. The minor fissure (closed white arrow) is pulled upward and the major fissure is pulled forward (closed black arrow). This is a child who had asthma leading to formation of a mucus plug, which obstructed the right upper lobe bronchus.
|
|

What is this?
|
Atelectasis of the left lung. There is complete opacification of the left hemithorax with shift of the trachea (closed black arrow) and the esophagus (marked here by a nasogastric tube) (open black arrow) toward the side of the atelectasis. The right heart border, which should project about a centimeter to the right of the spine, has been pulled to the left side and is no longer visible. The patient had an obstructing bronchogenic carcinoma in the left main bronchus.
|
|
What is this?
|
Atelectasis of the right lung. There is complete opacification of the right hemithorax with shift of the trachea (closed black arrow) toward the side of the atelectasis. The left heart border is displaced far to the right and now almost overlaps the spine (closed white arrow). This patient had an endobronchial metastasis in the right main bronchus from her left-sided breast cancer (did you notice the left breast was surgically absent?) and was already receiving chemotherapy through an indwelling central venous catheter (open black arrow).
|
|

What is this?
|
Left upper lobe atelectasis. On the frontal projection (A), there is a hazy density surrounding the left hilum (open black arrow) and there is a soft tissue mass in the left hilum (closed black arrow). Notice how the left hemidiaphragm has been pulled up to the same level as the right. The lateral projection (B) shows a bandlike zone of increased density (closed white arrows) representing the atelectatic left upper lobe sharply demarcated by the major fissure, which has been pulled anteriorly. The patient had a squamous cell carcinoma of the left upper lobe bronchus that was producing complete obstruction of that bronchus.
|
|

What is this?
|
Subsegmental atelectasis. Close-up view of the lung bases demonstrates several linear densities extending across all segments of the lower lobes, paralleling the diaphragm (open black arrows). This is a characteristic picture of subsegmental atelectasis, sometimes also called discoid atelectasis or plate-like atelectasis. The patient was postoperative from abdominal surgery and was unable to take a deep breath. The atelectasis disappeared within a few days after surgery.
|
|

What is this?
|
Compressive (passive) atelectasis. Passive compression of the lung can occur either from a poor inspiratory effort (A), which is manifest as increased density at the lung bases (open white arrow) or secondary to a large pleural effusion or pneumothorax (B). Axial CT scan of the chest showing only the left hemithorax (B) demonstrates a large left pleural effusion (open black arrow). The left lower lobe (closed black arrows) is atelectatic, having been compressed by the pleural fluid surrounding it.
|
|
What is this?
|
Atelectasis and effusion in balance, an ominous combination. There is complete opacification of the right hemithorax. There are neither air bronchograms to suggest pneumonia nor any shift of the trachea (closed black arrow) or heart (open black arrow). The absence of any shift suggests the possibility of atelectasis and pleural effusion in balance, a combination that should raise suspicion for a central bronchogenic carcinoma (producing obstructive atelectasis) with metastases (producing a large pleural effusion).
|
|

What is this?
|
Round atelectasis, left lower lobe. There is a masslike density in the left lower lobe (open black arrow). The patient has underlying pleural disease in the form of pleural plaques from asbestos exposure (closed black arrows). There are comet-tail-shaped bronchovascular markings that emanate from the "mass" and extend back to the hilum (closed white arrows). This combination of findings is characteristic of round atelectasis and should not be mistaken for a tumor.
|
|

What is this?
|
Right upper lobe atelectasis and hilar mass: S sign of Golden. There is a soft tissue mass in the right hilum (open white arrow). There is opacification of the right upper lobe from atelectasis. The minor fissure is displaced upward toward the area of increased density (closed white arrows) indicating right upper lobe volume loss. The curved edge formed by the mass and the elevated minor fissure is called the S sign of Golden. The patient had a large squamous cell carcinoma obstructing the right upper lobe bronchus.
|
|
What do these show?
|
Left lower lobe and right lower lobe atelectasis. A, A fan-shaped area of increased density behind the heart is sharply demarcated by the displaced major fissure (closed black arrows) representing the characteristic appearance of left lower lobe atelectasis. On the lateral view (B), the major fissure (closed white arrow) is displaced posteriorly. The small triangular density in the posterior costophrenic sulcus is in the characteristic location for left lower lobe atelectasis as seen on the lateral projection. C, In a different patient there is a fan-shaped triangular density in the right lower lobe bounded superiorly by the major fissure (open white arrow). Notice how the unaerated lower lobe silhouettes the right hemidiaphragm (open black arrow).
|
|

What does this show?
|
Right upper lobe and left lung atelectasis from an endotracheal tube. The tip of the endotracheal tube extends beyond the carina into the bronchus intermedius (open black arrow), which aerates only the right middle and lower lobes (A). The right upper lobe and entire left lung are opaque from atelectasis. The minor fissure is elevated (closed white arrow) and the trachea (as marked by the endotracheal tube) is displaced to the left (open white arrow). B, One hour later, the tip of the endotracheal tube has been retracted (closed black arrow) and the right upper lobe and a portion of the left lower lobe are again aerated (white circles).
|

