![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
Digestive tract
|
1. mouth
2. esophagus 3. stomach 4. small intestines (duodenum, ileum, jejunum) 5. large intestines (ascending colon, transverse colon, descending colon, sigmoid colon) 6. rectum 7. anus |
|
|
Mouth
|
Digestion begins in the mouth with alpha-amylase contained in saliva
breakdown of starch chewed food forms clump called bolus |
|
|
alpha-amylase
|
contained in saliva
begins breakdown of starch (carbohydrates) into polysaccharides |
|
|
esophagus
|
bolus is pushed into esophagus from mouth by swallowing
bolus is moved down esophagus by peristaltic action saliva acts to lubricate esophagus to help food move down no digestion occurs |
|
|
peristaltic action
|
wave motion, similar to squeezing a tube of toothpaste at bottom and sliding fingers toward top to expel toothpaste
movement is performed by smooth muscles |
|
|
stomach
|
bolus moves into stomach through lower esophageal sphincter (cardiac sphincter)
very flexible pouch that mixes and stores food reduces bolus to semifluid mass called chyme contains exocrine glands within its gastric pits begins protein digestion with enzyme pepsin low pH assists by denaturing proteins (pH 2) and kills bacteria no absorption occurs |
|
|
4 major cell types of stomach
|
1. mucous cell
2. chief (peptic) cell 3. parietal (oxyntic cells) 4. G cell |
|
|
G cell
|
secrets gastrin into interstitium (bloodstream), which stimulates parietal cells to secrete HCl
|
|
|
Mucous cell
|
contains rough ER and golgi to make mucus, composed of glycoprotein and electrolytes
secretes mucus to lubricate stomach and protect epithelial lining different types line stomach wall and necks of exocrine glands some secrete small amounts of pepsinogen |
|
|
parietal cell
|
found in exocrine glands of stomach
secrete HCl, which diffuses to lumen. also secrete intrinsic factor, helps ileum absorb B12 used to lower pH of stomach and raise pH of blood Have many mitochondria to produce sufficient energy to establish proton gradient |
|
|
Chief (peptic) cell
|
synthesizes pepsinogen on rough ER, which is later cleaved to active pepsin
deep in exocrine glands secret pepsinogen (zymogen precursor of pepsin) |
|
|
pepsinogen
|
zymogen precursor to pepsin
activated to pepsin by low pH in stomach once activated, pepsin beings protein digestion |
|
|
gastrin
|
secreted by G cells into interstitium
large peptide hormone absorbed into blood stimulates parietal cells to secrete HCl |
|
|
Major hormones affects secretion of stomach juices?
|
1. acetylcholine: increases secretion of all cell types
2. gastrin: increase secretion of HCl 3. histamine: increase secretion of HCl |
|
|
Small intestines
|
90% of digestion and absorption occurs in small intestines
3m in length divided into 3 parts (smallest to largest): 1. duodenum (digestion) 2. jejunum (absorption) 3. ileum (absorption) Pyloric sphincter is between stomach and duodenum |
|
|
villi
|
finger-like projections that covers outermost layer of small intestines
increases surface area, allowing for greater digestion and absorption each contain capillary network and lymph vessel (lacteal) through which absorbed nutrients pass |
|
|
microvilli
|
smaller finger-like projections on apical (lumen side) surface of cells of each villus (cells called enterocytes)
increase surface area appear as fuzzy covering |
|
|
brush border
|
fuzzy covering of microvilli on villus
contains membrane bound digestive enzymes for carbohydrates, proteins, nucleotides |
|
|
goblet cells
|
epithelial cells on the small intestinal lining that secrete mucus to lubricate intestines and help protect brush border from mechanical and chemical damage
|
|
|
Pancreas
|
secretes bicarbonate ion into duodenum to make pH 6
exocrine glands also secretes enzymes: trypsin, chymotrypsin, pancreatic amylase, lipase, ribonuclease and deoxyribonuclease all enzymes are released as zymogens Enterokinase activates trypsin which activates other enzymes |
|
|
trypsin and chymotrypsin
|
degrade proteins into small polypeptides.
Carboxypeptidase (pancreatic enzyme) further cleaves amino acids from the sides of the peptides |
|
|
pancreatic amylase
|
like salivary alpha-amylase, but more powerful
digests starch, carbohydrates hydrolyzes polysaccharides to disaccharides and trisaccharides degrades carbohydrates of chyme to small glucose polymers |
|
|
lipase
|
degrades fats, specifically triglycerides
since intestinal fluid is aqueous solution, fat clumps together, reducing surface area, which makes degradation difficult, problem fixed by addition of bile |
|
|
bile
|
produced by liver and stored in gall bladder
gall bladder releases bile into small intestines needed to increase surface area of fat physically separates fat molecules, but does not chemically break down fat emulsifies fat, doesn't digest fat Bile is reabsorbed by small intestine and transported back to liver |
|
|
emulsification
|
what bile does to fat
breaking up of fat into small particles without changing it chemically increases surface area of fat, allowing lipase to degrade it into fatty acids and monoglycerides |
|
|
large intestines
|
site of water and electrolyte absorption
profuse water loss, diarrhea, results when there is a problem with large intestines mutualistic symbiosis between humans and bacteria (E. coli) in large intestines, bacteria get our leftovers and we get vitamins (K, B12, thiamin and riboflavin) made up of: 1. ascending colon 2. transverse colon 3. descending colon 4. sigmoid colon |
|
|
glycogenesis
|
formation of glycogen from glucose
glycogen is stored occurs when blood glucose levels increase occurs in liver and muscle cells all cells are capable of storing glycogen, liver and muscle cells store most glycogen |
|
|
glycogenolysis
|
occurs when blood glucose levels decrease
glycogen in converted to glucose takes place in the liver and glucose is returned to blood |
|
|
urea
|
ammonia is converted to urea by liver and then excreted in urine by kidney
|
|
|
albumin
|
fatty acids combine with albumin in the blood
single molecule of albumin carried 3 fatty acid molecules, but is capable of carrying up to 30 |
|
|
the liver and the vena cava
|
Vena cava is the location where all blood that has passed through liver is deposited
The liver receives blood from the capillary beds of the intestines, stomach, spleen, and pancreas via the hepatic portal vein. |
|
|
functions of liver
|
1. blood storage
2. blood filtration (kupffer cells phagocytize bacteria) 3. carbohydrate metabolism (regulates blood glucose through gluconeogenesis, glycogenesis, storage of glycogen) 4. fat metabolism (cholesterol -> bile, carbs/protein -> fat, forms lipoproteins) 5. protein metabolism (forms urea from ammonia in blood, synthesizes plasma proteins, deaminates AA's, synthesizes NONessential AA's) 6. detoxification 7. erythrocyte destruction 8. vitamin storage (A, D, B12, ferritin) when the liver mobilizes fat or protein for energy, the liver makes ketone bodies which increases blood acidity (acidosis) |
|
|
Kidney function
|
1. excrete waste products (urea, uric acid, ammonia and phosphate)
2. maintain homeostasis of body fluid volume and solute composition 3. help control plasma pH |
|
|
Kidney
|
2 fist-size organs
made up of: 1. outer cortex 2. inner medulla The kidney creates urine |
|
|
What is the renal pelvis? What is the flow of urine starting from renal pelvis?
|
Renal pelvis is where urine is emptied to from the kidney
Renal pelvis -> ureter -> bladder -> urethra |
|
|
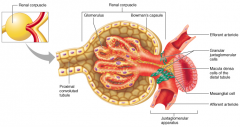
nephron
|
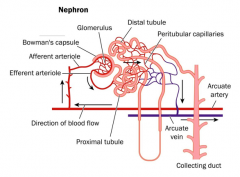
the functional unit of kidney
Made up of: 1. glomerulus 2. bowman's capsule 3. renal corpuscle 4. proximal tubule 5. loop of henle 6. distal tubule 7. collecting duct 8. juxtaglomerular apparatus |
|
|
glomerulus
|
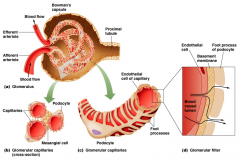
First step: blood flows into the 1st capillary bed of nephron
hydrostatic pressure forces some plasma through fenestrations of the glomerular endothelium and into Bowman's capsule. The glomerulus contains fenestrations which sieve out filtrate (primary urine) and hold back blood cells and large proteins. |
|
|
renal corpuscle
|
made up by bowman's capsule and glomerulus
it is where filtration occurs |
|
|
proximal tubule
|
After filtrate is sieved into bowman's capsule, the filtrate moves to the proximal tubule.
Proximal tubule is where most reabsorption takes place secondary active transport proteins in apical membranes of proximal tubule cells are responsible for reabsorption of glucose, proteins and other solutes water is reabsorbed across relatively permeable tight junctions due to favorable osmotic gradient drugs, toxins and other solutes are secreted into filtrate by cells of proximal tubule also secreted into proximal tubule: uric acid, bile pigments, antibiotics and other drugs Antiport system: secretes H+ ions into the filtrate through Na+, driven by Na+ concentration gradient. similar to transport system of glucose with Na+, except H+ crosses membrane in opposite direction to Na+ net result of proximal tubule: reduce amount of filtrate in nephron, while changing solute composition without changing osmolarity |
|
|
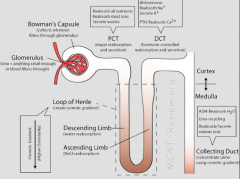
loop of henle
|

filtrate flows to here from proximal tubule
dips into medulla It concentrates solute into the medulla, thus increasing osmotic pressure of medulla. water passively diffuses out and into medulla 2 parts: 1. descending loop of henle 2. ascending loop of henle The vasa recta is a second capillary bed that surrounds the loop of henle and helps to maintain the concentration of the medulla. |
|
|
descending loop of henle
|
As filtrate descends into the medulla, water passively diffuses out of the loop of Henle and into the medulla.
DLOH has low permeability to salt, so filtrate osmolarity goes up. DLOH is permeable to water |
|
|
ascending loop of henle
|
As filtrate rises out of medulla into cortex, salt diffuses out, passively at first and then actively
ALOH is impermeable to water actively transports Na+ into kidney |
|
|
distal tubule
|
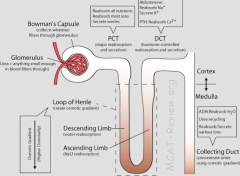
reabsorbs Na+ and Ca+2
secretes K+, H+ and HCO3- ADH acts on distal tubule cells to increase Na+ & K+ membrane transport proteins net effect of distal tubule: lower filtrate osmolarity ADH acts to increase permeability of cells to water presence of ADH, water flow from tubule, concentrating filtrate |
|
|
collecting duct
|

where distal tubules empties
carries filtrate into highly osmotic medulla impermeable to water and sensitive to ADH In the presence of ADH, collecting duct becomes permeable to water allowing it to passively diffuse in medulla, concentrating urine leads to renal pelvis |
|
|
juxtaglomerular apparatus
|
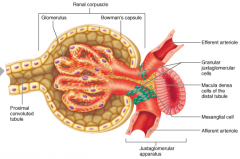
monitors filtrate pressure in distal tubule
granular cells secrete renin enzyme, to initiate regulatory cascade which ultimately stimulates adrenal cortex to secrete aldosterone aldosterone acts on distal tubule, stimulating formation of membrane proteins that absorb Na+ and secrete K+ |
|
|
Aldosterone
|
Acts on the distal tubule. Stimulates the formation of membrane proteins that absorb sodium and secrete potassium. Raises blood pressure.
Renin -> angiotensin -> aldosterone |

