![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
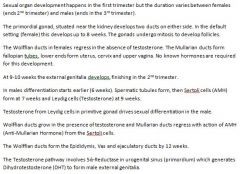
Describe the different processes involved in the differentiation of male and female sexual organs (internal) and the hormones controlling this differentiation.
|
|
|
|
What is cryptorchidism and what causes it?
|
Cryptorchidism is the most common defect in male childbirth (3%)
It describes a condition where the testes fail to descend from the abdomen to the scrotum - a process normally driven by DHT (DiHydroTestosterone) As a result, cryptorchidism can result from a number of causes: 1. Hypothalamic failure to secrete GnRH 2. Testes failure to secrete androgens 3. 5-alpha reductase deficiency (so no conversion of testosterone to DHT) 4. Androgen receptor failure (insensitivity) |
|
|
What is Klinefelters?
|
Typically 47XXY (or 46XX) are boys born with boobs, hips, fat, and small balls. They have a low level of testosterone secretion, and high levels of oestrogen.
|
|
|
What is Turner's syndrome?
|
45XO. Girls born short, with webbed necks, left sided heart abnormailities, renal and GI complications. Ovaries replaced by streak gonads, infertile.
|
|
|
Describe the key genetic and hormonal features determining sexual differentiation.
|

|
|
|
Describe the secretion of GnRH and its effects on FSH and LH and how this changes at puberty
|
Secretion of GnRH is pulsatile so secretion of LH and FSH are also pulsatile.
GnRH is inhibited until puberty, in lactation and when dieting. |
|
|
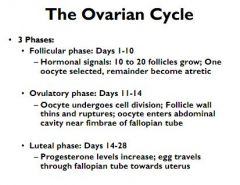
Describe the development of oocytes in the foetus.
|

Primordial germ cells divide into oogonia my mitosis
Oogonia undergo meiosis to form primary follicles (flat granulosa) Primary follicles are arrested in prophase of meiosis 1 Primordial follicles develop into secondary follicles with a thick stratified epithelial outer which sits on a basement membrane outer – Membrana granulosa and has a thinner Zona Pellucida inside Secondary follicle granulosa cells secrete fluid which collects to form a crescent shaped antrum. This swells. Granulosa around oocyte form cumulus oophorus - Graafian follicle |
|
|
Describe the changes in hormones in the menstrual cycle
|
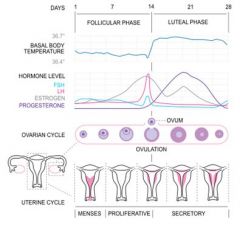
FSH up at the end of the cycle, stimulates development of around 20 primary follicles
Granulosa secretes oestrogens, FSH and LH are inhibited Oestrogen drives the LH surge at day 14 Secondary oocyte and first polar body results Meiosis 2 begins but arrests, only continues if egg is fertilised LH causes ovarian contractions, enzymes digest collagen around the follicle Corpus luteum formed granulosa and thecal cells. Oestrogens and progesterone act on endometrium. Progesterone lowers GnRH, affecting FSH and LH |
|
|
Summarise the ovarian cycle
|
|
|
|
Summarise all the hormones involved in the female reproductive cycle, where they come from, and what they do
|

|
|
|
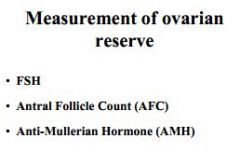
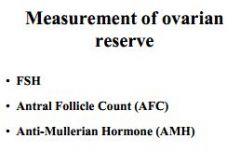
How do you measure ovarian reserve?
|
|
|
|
How do you measure ovarian reserve?
|
|
|
|
|
|

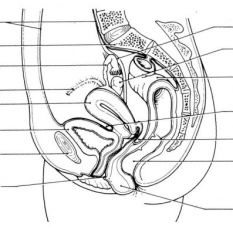
What is shown in this picture, and what are they?
|
The bottom label refers to 'Gartner's Ducts'
These are remnants of the embryological 'mesonephric ducts', which form the epididymis and vas in the male. These lie between the uterus and the wall of the vagina. |
|
|
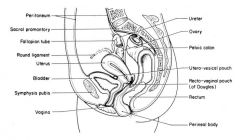
What are the typical diameters of the pelvic inlet and outlet
|

Inlet (13cms wide, 11cms deep 11)
Outlet (11cms wide by 13cms deep) |
|

|
|
|

|
|
|
|
|
|
|
Describe the blood supply and lymphatic drainage of the female reproductive organs?
|
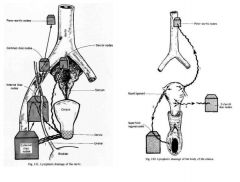
Blood supply
Ovarian artery - From Aorta - Ovary and Fallopian tube Uterine artery - Internal Iliac - Uterus and Fallopian tube |
|
|
Describe changes to the mucus in the cervix.
|
At ovulation
Clear and stringy due to glycoproteins, supports and nourishes sperm on journey through cervix and uterus After ovulation Progesterone causes cross-linking, no sperm gets through During pregnancy Forms a thick leucocyte rich plug to block infection |
|
|
List factors affecting male fertility
|
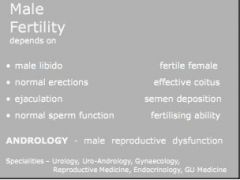
|
|
|
What commonly causes male subfertility?
|
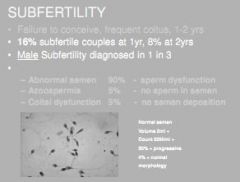
90% Abnormal sperm
5% Azoospermia 5% Coital dysfunction |
|
|
What are the 3 sections of the male urethra?
|
A. Prostatic
B. Membranous C. Spongiosus |
|
|
Describe how the position of a lesion of the spinal cord could affect the way ejaculation can be stimulated
|
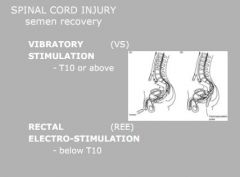
|
|
|
Describe the nervous control and physiology associated with orgasm in men
|

Orgasm occurs in right pre-frontal cortex, Septal Nucleus of the hypothalamus, and the pituitary.
Hypothalamus produces dopamine to stimulate. 5-HT inhibits. Posterior pituitary produces Oxytocin. Ejaculation is essentially emmission plus ejection. Emmission is a sympathetic response involving the ejactulatory centre in the spinal cord (T10-L2), this also closes the bladder nack to prevent retrograde ejactulation. Ejection is a somatic reflex, involving Sacral nerves 2-4 |
|
|
Describe the nervous control and physiology associated with orgasm in men
|

Orgasm occurs in right pre-frontal cortex, Septal Nucleus of the hypothalamus, and the pituitary.
Hypothalamus produces dopamine to stimulate. 5-HT inhibits. Posterior pituitary produces Oxytocin. Ejaculation is essentially emmission plus ejection. Emmission is a sympathetic response involving the ejactulatory centre in the spinal cord (T10-L2), this also closes the bladder nack to prevent retrograde ejactulation. Ejection is a somatic reflex, involving Sacral nerves 2-4 |
|
|
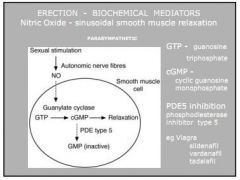
Describe the anatomy and physiology behind the male erection.
|
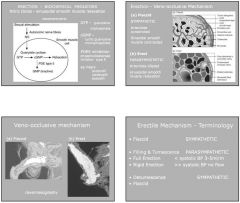
The male penis has three glans, 2x corpus canvernosum and 1xspongiuosum. The urethra lies in the spongiosum.
There are two cavernosal arteries, and only one dorsal vein. Erection involves stimualtion of higher centres, and parasympathetic nerves (S2-4). This deliver NO to the smooth muscle cells of the arteries to the penis, causing dilation via guanylate cycles, conversion of GTP to cGMP. The swelling of the corpus cavernosa, occludes the dorsal vein, trapping blood in the penis. Sympathetic nerves (T11-L2) constrict the arteries, causing the loss of blood to the cavernosa, subsequent relaxation and loss of blood through the vein (flaccidity) |
|
|
Explain the mechanism of action of viagra
|
|
|
|
Describe the prostate, give its blood supply and venous drainage. Explain the sites for Benign Prostatic Hypertrophy and malignancy.
|
Prostate is walnut sized. Has several lobes, anterior, posterior, medial and lateral.
It also has two distinct zones - transitional (BPH) and peripheral (malignancy) Blood is from the internal iliac via the inferior vesicle, middle pudendal and internal pudendal Venous drainage is pampiniform. |
|
|
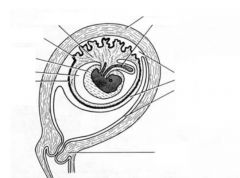
Describe the scrotums 8 layers, give its blood and nerve supply and venous drainage.
|
1. Skin
2. Dartos muscle 3. External spermatic fascia 4. Cremaster 5. Internal spermatic fascia 6. Tunica vaginalis (parietal) 7. Tunica vaginalis (visceral) 8. Testes (Tunica Albuginea) Blood supply - External pudendal Venous drainage - Meme Lymphatics - Superficial inguinal Nerves: Genitofemoral, Ilioinguinal, lateral cutaneous femoral, posterior perineal, T10-11 spermatic cord. |
|
|
Describe the fascia, blood and nerve supply to the spermatic cord.
|
3 Fascia:
External Spermatic, Cremasteric, and Internal Spermatic 3 Arteries: Testicular (aorta), Ductus Deferens (Inferior vesicle), Cremasteric (Inferior Epigastric) 3 Nerves: Genito-femoral, Ilioinguinal, and sympathetics |
|
|
Describe the blood supply and venous drainage to the testes
|

Right - IVC
Left - Renal |
|
|
Describe the various glands of the male reproductive tract and their secretions
|
Seminal vesicles - Sacular, join Vas at it's ampulla. Mucus secreting goblet cells, semen has Semeniligen for coagulation
Prostate - Produces milky, alkaline secretion Cowper's - Alkali, base of penis Littre's - In penis. Lube. |
|
|
Describe the anatomy of the male reproductive organs
|

Each testes is made up of seminiferous tubules, 60cms in length, contained in 250 compartments each containing 2-4 tubules (total 750 tubules)
They collect in the Rete Testis, at the mediastinum of the testes, with 20 collecting ducts, going into the Epididymis (6m long) - which has a head, a body and a tail. Head absorbs fluid for the sperm. Cuboidal, ciliated. Tail - pseudostratified columnar with microvilli - metabolic exchange with sperms. Epididymis empties into the Vas Deferens (30cms), has thick, smooth muscle walls, goes up the back of the spermatic cord, through the inguinal canal, around the inferior epigastric, runs along the bladder - thickens to form the ampulla. Joins seminal vesicle - forms ejactulatory ducts. Pierces prostate gland. |
|
|
Describe the makeup of sperm.
|

|
|
|
Describe changes to cervical mucus in the menstrual cycle under the influence of hormones.
|
Cervical mucus properties change under action of oestrogen:
Increase in hydration and alignment of glycoproteins alter stretchiness Mid cycle mucus promotes penetration of sperm Swimming character changed by alignment of muco-proteins Progesterone environment causes cross-linking and mucus plug |
|
|
Outline the steps involved in the fertilisation of the egg once the sperm is in the fallopian tube
|
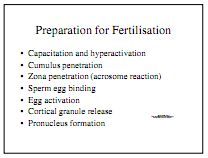
Sperm immotile in isthmus of fallopian tube
Hyperactivation - Ovulation increases Ca2+, cAMP and Adenylate Cyclase Capacitation - Changes in the ionic charge cause sperm activation, loss of glycoprotein coat Acrosome reaction - Capacitated sperm bind the ZP3 receptor on Zona Pellucida of the egg. Ca2+ causes depolarisation and egg becomes impermeable to extra sperm. ZP2 holds sperm in egg. ZP3 also causes Cortical granulation which hardens the Zona Pellucida Pronuclei form, swell, spindles, DNA synthesis... first meiotic division begins Pronuclei breakdown, chromosomes mix, first mitotic division occurs = Diploid progeny Division continues - Morula is 16 cells 32-64 cell blastocyst is next (1 week), this enters the uterus Outer cells are trophoblasts, inccer cell mass forms pluripotent stem cells. |
|
|
Give causes and treatments for anovulation
|
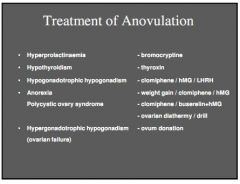
|
|
|
Give common causes of tubal damage
|
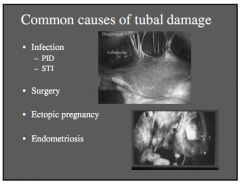
|
|
|
Define male subfertility
|
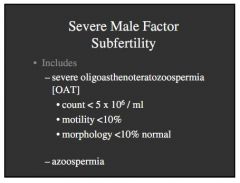
|
|
|
Define gestational age and embryonic age.
|
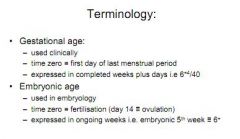
|
|
|
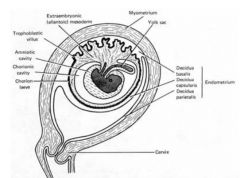
Describe the events associated with the implantation phase, and give rough timings in days for each stage.
|
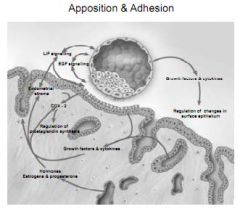
Process of implantation begins around day 7 and lasts till day 10
Apposition - Secretion of mediators by both the embryo and uterus including Leukaemia Inhibiting Factors, cytokines and Prostaglandins Attachment - Ligands on the blastocyst bind receptors on uterine lining Penetration - Embryo surface molecules change to promote invasion, proteases digest decidual cells |
|
|
Describe the differentiation of trophoblastic cells
|

|
|
|
Describe the development of the placenta from D10 to 12
|
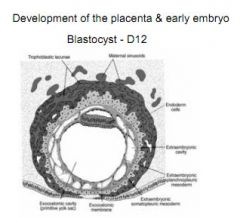
Endometrium forms decidua around the embryo. Sprial uterine arteries appear
|
|
|
Describe the development of placental villi between D13 and D28.
|
D14 - 28
Appearance of chorionic villi • Primary villous stems have a central core of cells derived by the proliferation of the cytotrophoblast. • The primary villi gradually develop mesenchymal cores, which convert them into the secondary villi. • The mesenchymal cells within the villi differentiate into blood capillaries, thus forming the tertiary villi. • The vessels from the villi soon become connected with the embryonic heart via vessels that differentiate in the mesenchyme of the chorion and in the connecting stalk |
|
|
What forms the chorion leavae and chorion frondosum and why is this significant?
|
Villi on the decidual side for chorion leavae. Villi by decidual plate form chorion frondosum
Placenta = Chorion Frondosum + Decidual Plate |
|
|
Describe placental features at the end of the fourth gestational month
|
By the end of the fourth month of the pregnancy,
the placenta has attained its definitive form and undergoes no further anatomical modifications. Two components: the maternal portion formed by Development of the placenta • Two components: the maternal portion, formed by the decidual plate, and a fetal portion, made by the chorion frondosum. • On the maternal side decidual septa extend into the intervillous spaces, dividing placenta into 10- 38 cotyledons |
|
|
There are three types of monozygotic twins, what are they and how do they arise?
|
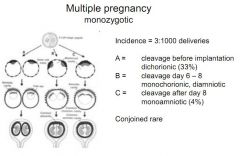
|
|
|
What are the three layers of gastrulation?
|
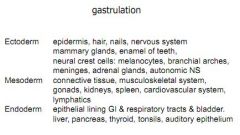
|
|
|
Describe the changes seen from week 4 to week 10. Give examples of conditions which can be found at that stage of development.
|
4th week - Spina bifida
6th week - Heart forms as paired tubes 7th week - Limb buds, vitelline ducts, caudal spine 8th week - Brain development, forebrain, midbrain and hindbrain can be seen 9th week - Eyes, movements 10th week - Heart forms chambers |
|
|
What does the abortion act say?
|
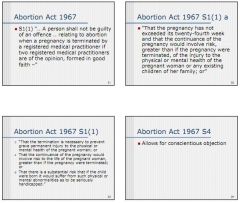
|
|
|
What are the main differences in female and male reproduction?
|
1. Blood testes barrier
2. Mitosis 3. Non-cyclic release of GnRH |
|
|
List some factors affecting male fertility and spermatogenesis
|
Heat >34degrees
Pollution Radiation Stress/smoking/drugs - causing oxidative stress which affects DNA synthesis, protein synthesis Klinefelters Kallmans (hypogonadism due to lack of GnRH) Hyperprolactinaemia |
|
|
Explain control of male reproductive function by the brain
|
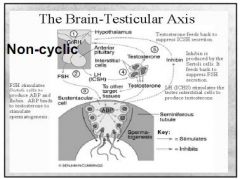
Non-cyclic release of GnRH, stimulates FSH and :LH
FSH acts on Sertoli cells, they secrete nutrients for sperm, as well as inhibins as a negative feedback LH acts on Leydig cells, they secrete androgens like testosterone, which further stimulates sertoli cells (and allows them to make oestrogens) and also feeds back directly on the hypothalamus |
|
|
Describe spermiogenesis
|

A spermatogonia from stem cells under 4 lots of mitosis
B spermatogonia form at the next to last mitosis Primary spermatogonia exist after final mitotic division Secondary spermatogonia after the first meiotic division Haploid spermatids after second meiotic division Maturation - funny shape changes etc |
|
|
What forms the blood testes barrier and why is it important?
|
Sertoli cells form tight junctions protecting the spermatids, this is vital as otherwise immune system would fuck them up
|
|
Label the diagram
|
|
|
|
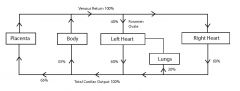
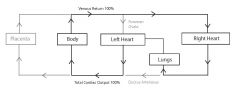
Describe blood flow in the materno-foetal exchange
|
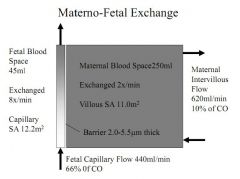
|
|
|
Describe the transfer of O2, CO2, glucose, amino acids, IgG and bilirubin across the placenta
|
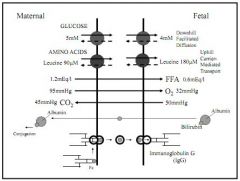
O2 - foetal Hb (y) has higher affinity for O2, so curve is to the left. PO2 in foetus is low (4.2kPa, to 3.2kPa)
CO2 - normal 6.6 - 6.1 kPa, diffuses along conc gradient Glucose - GLUT1 facilitated diffusion along conc gradient, insulin independent Amino acids, up conc gradient so requires energy IgG - always higher in foetus than mother Bilirubin - diffuses in free form, cannot cross placenta bound to protein |
|
|
Describe changes in the GI system in pregnancy and consequences.
|
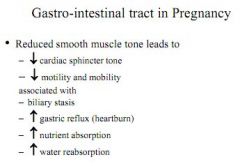
|
|
|
Describe changes in lung function and what stimulates these changes. Explain changes to PO2, PCO2 and why pH does not alter.
|
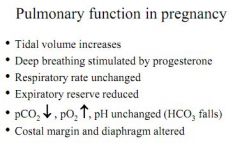
|
|
|
Explain changes in renal function and explain why normal markers for renal function might be unreliable in pregnancy
|
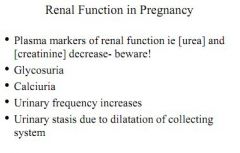
|
|
|
Explain changes in perfusion generally, and explain the consequences of changes in skin blood flow
|

Blood flow increases in all departments, skin, kidneys, uterus, gut.
|
|
|
Blood flow increases in pregnancy, explain the CVS changes seen and give reasons for these changes
|
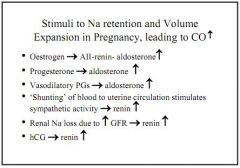
CO rises because blood volume rises. Blood volumes rises because of multiple stimulations of the Renin-Angio-Aldo system
Oestrogen raises Renin Progesterone raises Aldosterone Prostaglandins raise Aldosterone Loss of Na+ due to raised GFR raises Renin HcG also raises renin Despite all this TPR actually falls for three reasons: Increased NO causes relaxation by cGMP, prostacyclins cause relaxation by increased cAMP and blood volume increases shear forces which relax vessels by Ca2+ |
|
|
Explain where progesterone comes from in pregnancy and the role it plays
|
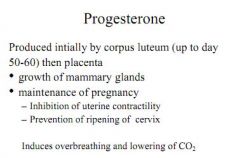
Comes from corpus luteum up to 60 days, then from the placenta itself. Delays labour by preventing the ripening of the cervix.
Also lowers CO2 by stimulating deeper breathing Grows boobs |
|
|
Explain the role of oestrogens in pregnancy
|
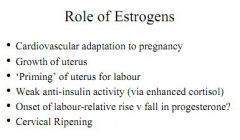
|
|
|
Explain how hormones are synthesised by the foetus and placenta in pregnancy
|

|
|
|
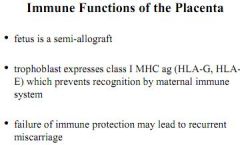
Give the immune functions of the placenta, how this appears to occur, and it's role in miscarriage
|
|
|
|
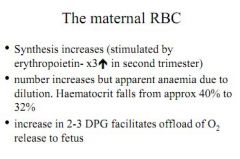
What happens to the maternal RBC count in pregnancy?
|
|
|
|
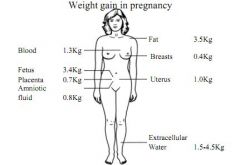
Describe weight gain in pregnancy.
|
|
|
|
Describe the foetal circulation giving reference to the three shunts.
|
|
|
|
Describe the foetal response to hypoxia
|
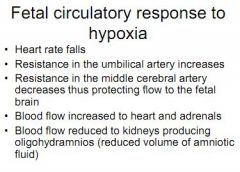
|
|
|
Describe changes to foetus at delivery
|
Cord occulsion decreases right atrial pressure, closing foramen ovale (in 60% of babies)
Inspiration of first breath causes vasodilation of pulmonary atery and lower resistance in plumonary circulation reduces flow through ductus arteriosus Increased PO2 closes ductus arteriosus This can be delayed by prostaglandins of accelerated by NSAIDs |
|
|
Describe changes in foetal lungs, and explain surfactant and the role of glucocorticoids
|
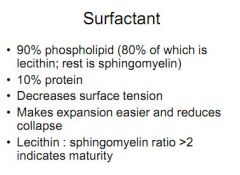
Secretory organ in foetus producing liquids and surfactant. Alveoli develop at week 24 - can see breathing movements in third trimester
Surfactant is 90% phopholipids, 10% protein, reduces lung surface tension Glucocorticoids can speed up lung development and surfactant synthesis, but can also cause diabetes in later life if administered to foetus |
|
|
Describe the importance of foetal Hb in foetal development
|
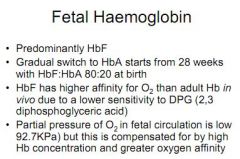
|
|
|
What stimulates the first breath?
|
|
|
|
Describe the stimulation and mechanism for the ejection of milk during feeding
|
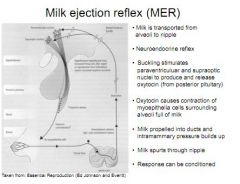
Suckling stimulates the release of oxytocin via supraoptic and paraventricular nuclei in hypothalamus
Oxytocin causes contractions of myoepithelium surrounding breast alveoli |
|
|
The various components of breast milk are secreted in different ways, explain this
|
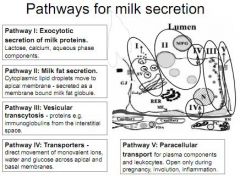
Proteins secreted by exocytosis after manufacture in Golgi
Milk fats from cytoplasm form droplets which pass out separately bound in a membrane Proteins from interstitium diffuse out, and ions, H2O and glucose move directly. Finally, leucocytes pass out paracellularly. |
|
|
Explain how suckling producing milk secretion (not ejection).
|
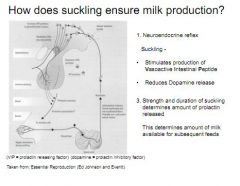
Suckling stimulates Vasoactive Intestinal Peptide, which inhibits dopamine, which inhibits Prolactin
|
|
|
Prolactin is secreted by the mother from 16 weeks, why does this not allow her to produce breast milk until term?
|
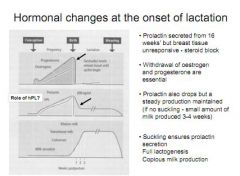
|
|
|
Describe the important mechanisms thought to be involved in parturition
|

|
|
|
Explain factors thought to be involved in the preparation of the myometrium for labour and what might cause this
|
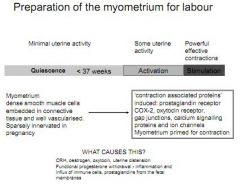
|
|
|
Describe factors which cause the cervix to ripen and what is thought to cause this
|
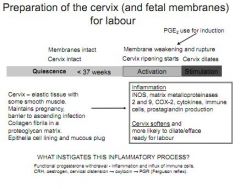
|
|
|
What are the three stages of labour?
|

|

