![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
How common is ICH? |
15% to 20% of all new strokes annually; twice as common as subarachnoid hemorrhage and just as deadly, with a 30 day mortality of 30% to 50%
|
|
|
What are the most common causes of ICH? (4) |
1. Hypertension (50%) 2. Amyloid angiopathy ([CAA] about 20% of cases) 3. Anticoagulant use accounts for 15% to 17% 4. Other |
|
|
Hypertensive ICH usually occurs where? |
Deep areas of the brain, such as the basal ganglia, pons, and cerebellum |
|
|
Underlying mechanism of hypertensive ICH? |
Accelerated age-related degeneration of cerebral arterioles at their branch points |
|
|
Deposits in CAA? |
Amyloid protein deposits occurs in the media and adventitia of arteries and arterioles, usually in the cerebral cortex |
|
|
Clinical presentation of ICH? |
1. Sudden-onset, focal neurologic deficit 2. Impaired consciousness 3. Headache 4. Elevated blood pressure, nausea, and emesis are more common in ICH than in ischemic stroke |
|
|
Timeframe for expansion in ICH? |
1. Noncoagulopathic ICH - in the initial 6 hours 2. Coagulopathic ICH - in the initial 24 hours |
|
|
Perihematomal edema and increased intracranial pressure reach maximum levels when? |
Around 72 hours after the ictus |
|
|
Onset of symptoms during coitus or physical activity might suggest what mechanism underlying the ICH? |
Rupture of a vascular structure such as an aneurysm or an AVM |
|
|
Medical history in ICH should focus on? |
1. Time of symptom onset or time of awareness 2. Recent head trauma? 3. Vascular risk factors? 4. Medications 5. History of previous stroke? 6. History of coagulopathies or systemic conditions that predispose to bleeding |
|

|
Hypertensive ICH in the left putamen and globus pallidus with extension superiorly |
|
|
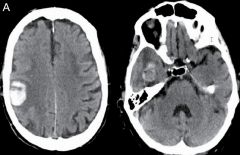
CT of ICH secondary to CAA shows right posterior frontal hematoma (image on the left) and right temporal lobar ICH ( image on the right) |
|
|
What might suggest a coagulopathy when evaluating CT scans of ICH? |
Fluid level within the hematoma or blood in different stages |
|
|
Role of CT angio in patients with confirmed blood on noncontrast CT? |
CTA and contrast-enhanced CT may be considered to help identify patients at risk for hematoma expansion |
|
|
What is "spot" sign due to? |
Vascular leak at the point of enhancement and may predict hematoma enlargement |
|
|
Role of MRI in ICH? |
Rule out underlying structural abnormalities, such as tumors or AVM |
|
|
What are microbleeds? |
Small areas (<10mm) of ferritin and hemosiderin deposition appearing as signal dropout (profoundly hypointense) on T2 gradient-echo images and are considered the radiologic footprint of CAA when diffuse and predominantly in a cortical or subcortical location |
|
|
Differential diagnosis of microbleeds? |
1. CAA 2. Hypertensive microbleeds 3. Multiple cavernous malformations 4. Calcium 5. Mechanical heart valve emboli |
|
|
General recommendations regarding blood pressure in ICH? |
sBP <160 and AP 70-110 |
|
|
Corticosteroids in ICH?? |
No evidence of being beneficial |
|
|
Prophylactic anticonvulsants in ICH? |
No evidence of being beneficial |
|
|
Management of noncoagulant ICH? |
No indication to treat with blood products or with recombinant factor VIIa; for warfarin-related ICH, treat with vitamin K (10 mg as a slow iv infusion over 30 minutes), FFP, and 3- or 4-factor PCC |
|
|
Treatment recommendations for ICH related to newer anticoagulants? |
1. Activated charcoal 2. IV hydration 3. 4-factor PCC 4. Hemodialysis 5. Praxbind is an antidote to dabigatran (Pradaxa) |
|
|
Which ICH patients may benefit from surgery? (3) |
1. Cerebellar hemorrhage and a deteriorating neurologic status 2. Brainstem compression or hydrocephalus (or both) from ventricular obstruction 3. Lobar hemorrhages >30cm^3 and within 1 cm of the surface, evacuation of the supratentorial hemorrhage by standard craniotomy may be considered |
|
|
T1 and T2 signals characteristic of ICH in the hyperacute phase? |
T1 - isodense central and peripheral part of the hemorrhage T2 - increased signal both peripherally and centrally |
|
|
What is considered the hyperacute phase of ICH? |
<12 hrs |
|
|
T1 and T2 signals characteristic of ICH in the acute phase? |
T1 - isodense centrally and peripherally T2 - Decreased signal centrally, increased peripherally |
|
|
What is considered the acute phase of ICH? |
12-72 hrs |
|
|
T1 and T2 signals characteristic of ICH in the early subacute phase of ICH? |
T1 - isodense central, increased signal peripherally T2 - decreased central, markedly decreased peripherally |
|
|
What is considered the early subacute phase of ICH? |
4-7 days |
|
|
T1 and T2 signals characteristic of ICH in the late subacute phase? |
T1 - Markedly increased centrally and peripherally T2 - Markedly increased centrally and peripherally |
|
|
What is considered the late subacute phase of ICH? |
1-4 weeks |
|
|
T1 and T2 signals characteristic of ICH in the chronic phase? |
T1 - Increased centrally, decreased peripherally T2 - Increased centrally, decreased peripherally |
|
|
What is considered chronic phase of ICH? |
Months |
|
|
T1 and T2 signals characteristic of ICH in the late chronic phase? |
T1 - markedly decreased centrally and peripherally T2 - increased centrally, markedly decreased peripherally |
|
|
PCC? |
Prothrombin Complex Concentrate |
|
|
A reasonable approach to ICH? |
1. Aggressive, full care early after ICH onset 2. Postpone new DNR orders until at least the second full day of hospitalization 3. LMWH may be considered for prevention of venous thromboembolism in patients with lack of mobility, 3 to 4 days after ictus |
|
|
ICH score is based on five variables, what are they? |
1. GCS score (3-4 = 2 points, 5-12 1 point) 2. ICH volume (>30cm^3 = 1 point) 3. IVH present (yes = 1 point) 4. Infratentorial origin (yes = 1 point) 5. Age, y (>80 = 1 point) |
|
|
30-day mortality based on the ICH score? |
0 point = 0% 1 point = 13% 2 points = 26% 3 points = 72% 4 points = 97% 5-6 points = 100% |
|
|
Best predictor of outcome in ICH? |
Hematoma volume at presentation |
|
|
How is hematoma volume calculated? |
(A x B x C)/2, where A is the maximum ICH diameter, B is the maximum diameter perpendicular to A, and C is the maximum vertical diameter; values in cm |

