![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
Pharmacologic modulation of extracellular fluid volume
|
1. To increase or decrease body fluid volume, the kidneys must increase or
decrease renal Na+ reabsorption from the volume of glomerular filtrate. 2. This is accomplished by integrated action of apical and basolateral ion channels and transporters. 3. Pharmacologic modulators of extracellular fluid volume include agents that modify neurohormonal volume regulators (e.g., ACEIs and ARBs) and those that act directly on the nephron segments to alter renal Na+ handling. The latter category, the diuretics, will be the focus of this presentation. 4. The diuretics directly target renal ion transporter or channel function or expression to increase renal Na+ excretion and thereby decrease extracellular fluid volume. |
|
|
Proximal tubule
|
About 67% of sodium reabsorption occurs here
b. Solute absorption is iso-osmotic—water accompanies reabsorbed ions to maintain ionic balance c. The proximal tubule is the principle site of action for the carbonic anhydrase inhibitors (CAIs) (Acetazolamide and dorzolamide) and the osmotic diuretics (mannitol). |
|
|
Loop of Henle
|
a. The tubular fluid emerging from the thin ascending limb is hypertonic
and has an elevated NaCl concentration. b. The thick ascending limb (TAL) reabsorbs NaCl without accompanying water, diluting the tubular fluid. c. The TAL reabsorbs between 25% and 35% of the filtered Na+ load. d. The TAL of the loop of Henry is the principle site of action for the loop diuretics (ethacrynic acid and furosemide). |
|
|
Distal convoluted tubule
|
a. This continuation of the diluting segment reabsorbs between 2% and
10% of the filtered Na+ load, while remaining impermeable to water. b. The distal tubule is the principle site of action for the thiazide diuretics (hydrochlorothiazide and indapamide). |
|
|
Collecting duct
|
a. The principal cells of the proximal portions of the collecting duct
reabsorb between 1% and 5% of the filtered Na+ load. b. The reabsorption of Na+ is dependent upon plasma aldosterone levels (aldosterone increases Na+ reabsorption and water retention). c. The collecting duct is the principle site of action for the potassiumsparing diuretics (Amiloride, spironolactone, and triamterene). |
|
|
Loop diuretics
|
are the most potent
i. The thick ascending limb of the loop of Henle determines the final magnitude of natriuresis. ii. Loop diuretics which inhibit reabsorption in the TAL induce a very large Na+ and water loss. The distal tubule and collecting duct for Na+ reabsorption are not able to recapture the increased Na+ reaching these sites due to their relatively limited capacity for sodium reabsorption. iii. The loop diuretics retain their function in patient’s with very low creatinine clearance. |
|
|
Thiazide diuretics
|
The modest diuresis caused by the thiazides is due to the fact that 90%
of sodium reabsorption occurs before reaching the distal tubule. |
|
|
Osmotic diuretics
|
Not shown in the table, the osmotic diuretics are about equally effective
with the thiazide diuretics. |
|
|
Carbonic anhydrase inhibitors
|
These drugs which act proximal to the TAL have their natriuretic
response reduced by the ability of the TAL to augment its rate of Na+ reabsorption in the presence of increased tubular Na+ load (see below). |
|
|
Potassium-sparing diuretics
|
i. The collecting duct has a limited capacity to reabsorb solutes, thus
blockade of sodium channels by amiloride and triamterene only mildly increases the excretion rate of Na+. ii. Unlike the sodium channel inhibitors, the effects of spironolactone are a function of the endogenous levels of aldosterone. The higher the levels of aldosterone, the greater the effects of spironolactone |
|
|
Carbonic anhydrase inhibitors (Acetazolamide and dorzolamide)
1. Mechanism of action |
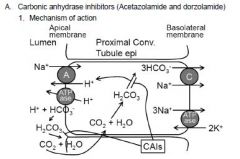
a. Na+ reabsorption in the proximal convoluted tubule
i. H+ is extruded into the tubular lumen by Na+/H+ antiporter and vacuolar ATPase. ii. The extruded H+ is coupled to HCO3 - reabsorption by apical membrane carbonic anhydrase (CAIV) which catalyzes cleavage of HCO3 - into OH- and CO2. The OH- combines with H+ to form water and the CO2 diffuses into the cell. iii. The cytoplasmic carbonic anhydrase (CAII) catalyzes formation of HCO3 - from CO2 and OH-. The bicarbonate is then transported to the interstitium together with sodium by a basolateral cotransporter |
|
|
Effects of carbonic anhydrase inhibitors
|
i. CAIs inhibit Na+ reabsorption by noncompetitively and reversibly
inhibiting proximal tubule cytoplasmic carbonic anhydrase II and luminal carbonic anhydrase IV. ii. This leads to an increase delivery of sodium and biocarbonate to more distal segments of the nephron. iii. Much of the sodium bicarbonate is initially excreted causing an acute decrease in plasma volume (diuresis). Over the course of several days, however, the diuretic effect is diminished by compensatory mechanisms resulting in up-regulation of sodium bicarbonate reaborption and by NaCl reabsorption across more distal nephron segments. |
|
|
Carbonic anhydrase inhibitors
Administration and elimination |
a. Acetazolamide administered orally and IV; dorzolamide as eye drops
b. Excreted largely unchanged in the urine—avoid use in severe renal impairment (drug is ineffective |
|
|
Carbonic anhydrase inhibitors
Adverse effects |
a. Metabolic acidosis
i. Inhibition of H+ secretion ii. Inhibition of CA acid secreting-intercalated cells of the collecting duct b. These drugs are sulfonamide derivatives thus they may cause allergic reactions in patients hypersensitive to sulfonamides |
|
|
Carbonic anhydrase inhibitors
Drug interactions |
Increased urinary pH increases excretion of organic acid anions and
decreases excretion of weak organic bases |
|
|
Carbonic anhydrase inhibitors
Contraindications |
COPD (increased risk of metabolic acidosis)
|
|
|
Carbonic anhydrase inhibitors
Clinical uses |
a. Dorzolamide reduces formation of aqueous humor and thus lowers
intraocular pressure in treating open angle glaucoma b. Acetazolamide i. Acute mountain sickness ii. Restore acid-base balance in heart failure patients with metabolic alkalosis caused by loop diuretics |
|
|
Osmotic diuretics (Mannitol)
1. Mechanism of action |
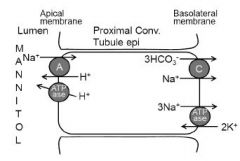
a. Osmotic diuretics such as mannitol are small molecules that are filtered
at the glomerulus but not subsequently reabsorbed in the nephron. b. They constitute an intraluminal osmotic force limiting reabsorption of water across water-permeable nephron segments. c. This effect is most pronounced in the loop of Henle and the proximal tubule where most iso-osmotic water reabsorption takes place |
|
|
Osmotic diuretics (Mannitol)
Administration and elimination |
a. Administered IV
b. Eliminated unchanged in the urine |
|
|
Osmotic diuretics (Mannitol)
Adverse effects |
Effects on Na+
i. Hypernatremia and dehydration due to water loss in excess of sodium excretion ii. Mannitol increases plasma osmolality leading to hyponatremia (manifested as headache, nausea and vomiting) due to the movement of fluid into the extracellular compartments |
|
|
Osmotic diuretics (Mannitol)
Contraindications |
a. Pulmonary congestion (INCR extracellular volume can cause pulmonary
edema) b. Heart failure (INCR extracellular volume can cause pulmonary edema) c. Severe renal disease (reduced GFR cannot dissipate the initial increase in extracellular volume expansion |
|
|
Osmotic diuretics (Mannitol)
Clinical uses |
Reduce intracranial pressure in neurological conditions
i. The decrease in systemic vascular volume induced by mannitol causes a reduction in cerebral intravascular volume ii. In addition, the increase in plasma osmolality contributes to the movement of fluid from the brain |
|
|
Loop diuretics (Ethacrynic acid and furosemide)
1. Mechanism of action |
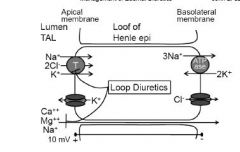
a. Na+ reabsorption in the thick ascending limb of the loop of Henle
i. Na+ is reabsorbed through an apical Na+/K+/2Cl- cotransporter. ii. The Na+/K+ ATPase pumps sodium into the interstitium. iii. Basolateral Cl- channel tranports Cl- into the interstitium iv. K+ is recycled into the urinary space by a luminal K+ channel. v. The combined activities of the K+ and Cl- channels is a lumenpositive transepithelial potential difference (about 10 mV) which drives paracellular absorption of cations |
|
|
Effects of loop diuretics
|
i. These drugs reversibly and competitively inhibit the Na+/K+/2Clcotransporter
thus inhibiting Na+ reabsorption. ii. This abolishes the transepithelial potential resulting in increased excretion of cations, particularly Mg++ and Ca++. iii. The increase in tubular flow increases K+ secretion by washing the K+ downstream thus minimizing the rise in tubular [K+]. The rise in tubular flow also increases the amount of sodium entering the distal tubule and collecting duct, which in turn enhances Na+ reabsorption and the lumen negative potential favoring K+ secretion. Finally, the increase in Na+ reabsorption stimulates K+ uptake across the basolateral membrane by increasing the activity of the Na+/K+ ATPase which promotes K+ secretion. iv. Inasmuch as 20% of the filtered Na+ load is reabsorbed by the loop of Henle, these drugs are the most effective diuretics |
|
|
Loop diuretics (Ethacrynic acid and furosemide)
Administration and elimination |
a. Administered orally and IV
b. The drugs are actively secreted into the tubular lumen c. Eliminated in the feces and urine as unchanged drug—in cases of severe renal impairment large doses (grams) may be necessary to initiate diuresis |
|
|
Loop diuretics (Ethacrynic acid and furosemide)
Adverse effects |
a. Effects on electrolytes
i. Hypocalcemia ii. Hypomagnesemia iii. Hypokalemia (predisposes patient to cardiac arrythmias) iv. Metabolic alkalosis b. Ototoxicity manifested as hearing impairment, tinnitus, deafness, and vertigo (reversible with furosemide; irreversible with ethacrynic acid)—occurs with rapid IV infusion (maintain infusion rate < 4 mg/min) c. Furosemide is a sulfonamide derivative and thus it may cause allergic reactions in patients hypersensitive to sulfonamides (Ethacrynic acid is NOT) d. Decreased glucose tolerance (may be due to impairment of insulin secretion or decreased peripheral insulin sensitivity; insulin secretion is increased by potassium, thus hypokalemia caused by loop diuretics may contribute to the decrease in insulin secretion) |
|
|
Loop diuretics (Ethacrynic acid and furosemide)
Drug interactions |
a. Aminoglycosides (synergism of ototoxicity)
b. NSAIDs can decrease effectiveness of loop diuretics (loop diuretics increase prostaglandin production which contribute to vascular effects of loop diuretics [vasodilation]) c. Oral hypoglycemics (Loop diuretics decrease glucose tolerance, may need to increase dose of oral hypoglycemic agents) |
|
|
Loop diuretics (Ethacrynic acid and furosemide)
Contraindications |
a. Patients with hypersensitivity to sulfonamide derivatives (Ethacrynic acid
would be an alternative) |
|
|
Loop diuretics (Ethacrynic acid and furosemide)
Clinical uses |
a. Relief of pulmonary and peripheral edema
b. Relief of edema associated with hypoalbuminemia (caused by liver disease or nephrotic proteinuria) c. Increased calcium diuresis is used to provide relief for hypercalcemia caused by hyperparathyroidism or malignancy-associated hypercalcemia; saline is administered concurrently to prevent volume depletion. d. Counteract hyperkalemia caused by potassium-retaining drugs or renal insufficiency with impaired K+ excretion e. Treatment of hyponatremia; Loop diuretics interfere with the kidney’s ability to produce a concentrated urine. Loop diuretics (to cause diuresis) in combination with hypertonic saline (to replace sodium) are useful for the treatment of life-threatening hyponatremia. |
|
|
Thiazide diuretics (Hydrochlorothiazide and indapamide)
1. Mechanism of action |
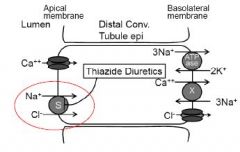
a. Na+ reabsorption in the distal convoluted tubule
i. Na+ enters the epithelial cells via the Na+/Cl- cotransporter. ii. Basolateral exit of sodium is mediated by Na+/K+ ATPase iii. Basolateral exit of Cl- occurs via Cl- channels. iv. Ca++ and Mg++ reabsorption occurs through channels in the apical membrane (only Ca++ channel shown). The ions cross the basolateral membrane via specific exchangers (only Ca++/Na+ exchanger shown) and by ATPases. |
|
|
Effects of thiazide diuretics
|
i. These drugs are competitive antagonists of the Na+/Clcotransporter.
ii. Thiazides promote transcellular reabsorption of calcium (may be due to increased expression of Ca++ channels and the Ca++/Na+ exchanger) |
|
|
Thiazide diuretics (Hydrochlorothiazide and indapamide)
Administration and elimination |
a. Orally administered
b. The drugs are actively secreted into the tubular lumen c. Hydrochlorothiazide excreted in urine—avoid use in severe renal impairment; indapamide is extensively metabolized by the liver |
|
|
Thiazide diuretics (Hydrochlorothiazide and indapamide)
Adverse effects |
a. Hypokalemia (due to increased delivery of Na+ to the collecting duct)
b. Impaired glucose tolerance (may be due to impairment of insulin secretion or decreased peripheral insulin sensitivity; insulin secretion is increased by potassium, thus hypokalemia caused by thiazide diuretics may contribute to the decrease in insulin secretion) c. Hyperuricemia (The thiazides compete with uric acid for active secretory sites in the proximal tubule thus inhibiting active secretion of uric acid; patients with gout may be particularly susceptible to the increase levels of uric acid) d. Thiazides are sulfonamide derivatives and thus they may cause allergic reactions in patients hypersensitive to sulfonamides |
|
|
Thiazide diuretics (Hydrochlorothiazide and indapamide)
Drug interactions |
a. Oral hypoglycemics (decreased effect of oral hyoglycemics)
b. NSAIDs (decrease the efficacy of thiazides) c. Loop diuretics (synergistic effect when combined with a thiazide diuretic) |
|
|
Thiazide diuretics (Hydrochlorothiazide and indapamide)
Contraindications |
a. Patients with hypersensitivity to sulfonamide derivatives (Ethacrynic acid
would be an alternative) b. Anuria |
|
|
Thiazide diuretics (Hydrochlorothiazide and indapamide)
Clinical uses |
a. Diminish hypercalciuria in patients at risk for nephrolithiasis
b. Hypertension (first-line drugs) c. Thiazide and loop diuretics used in combination in heart failure d. Nephrogenic diabetes insipidus (These kidneys of these patients do not respond to ADH and thiazides can produce a modest decrease in urine flow. This seemingly paradoxical effect is likely mediated through the extracellular volume contraction which promotes proximal tubular reabsorption of Na+ and water. Therefore a reduced volume is delivered to the distal tubule.) |
|
|
Potassium-Sparing Diuretics (Amiloride, spironolactone, triamterene)
1. Mechanism of action |
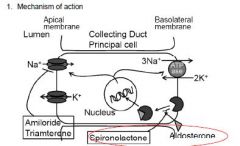
a. Na+ reabsorption in the collecting duct
i. Luminal Na+ enters the principal cell via a Na+ channel. ii. The Na+ exits the basolateral membrane via a Na+/K+ ATPase iii. The collecting duct cells express apical K+ channels that allow K+ to exit into the lumen iv. Expression of Na+ channels and Na+/K+ ATPase is modulated by aldosterone. |
|
|
Actions of potassium-sparing diuretics
|
i. Spironolactone inhibits synthesis of new Na+ channels (and new
Na+/K+ ATPase) in the principal cells by binding to and preventing nuclear translocation of the mineralcorticoid (aldosterone) receptor. ii. Amiloride and triamterene are competitive inhibitors of the apical membrane Na+ channel. iii. These drugs decrease K+ excretion by decreasing the lumen negative potential and thus decreasing the driving force for K+. iv. Proton secretion also is diminished by the decrease in Na+ uptake. |
|
|
Potassium-Sparing Diuretics (Amiloride, spironolactone, triamterene)
Administration and elimination |
a. Administered orally
b. Metabolized in the liver and excreted in the urine and feces. Avoid use in severe renal impairment |
|
|
Potassium-Sparing Diuretics (Amiloride, spironolactone, triamterene)
Adverse effects |
a. Hyperkalemia
b. Metabolic acidosis c. Impotence and gynecomastia caused by the antiandrogenic effects of spironolactone (not with amiloride or triamterene) |
|
|
Potassium-Sparing Diuretics (Amiloride, spironolactone, triamterene)
Drug interactions |
a. Concurrent use of these drugs with other potassium-sparing diuretics,
potassium supplements, ARBs, or ACEIs can increase the risk of hyperkalemia b. NSAIDs can decrease effectiveness |
|
|
Potassium-Sparing Diuretics (Amiloride, spironolactone, triamterene)
Contraindications |
a. Anuria
b. Hyperkalemia c. Concurrent use of potassium-sparing drugs, potassium supplements, ARBs, or ACEIs |
|
|
Potassium-Sparing Diuretics (Amiloride, spironolactone, triamterene)
Clinical uses |
a. Potentiate the action of more proximally acting diuretics
b. Counteract the potassium wasting of thiazide and loop diuretics c. Sprionolactone i. Heart failure (decrease mortality) ii. Treatment of ascites and edema associated with impaired plasma protein biosynthesis secondary to hepatic failure iii. Hypokalemic alkalosis secondary to mineralcorticoid excess that accompany heart failure, hepatic failure, and other diseases associated with diminished aldosterone metabolism d. Amiloride is used in treating lithium-induced nephrogenic diabetes insipidus (Lithium may inhibit the action of vasopressin on renal adenyly cyclase causing a lack of responsiveness to vasopressin and polyuria. Amiloride blocks the uptake of lithium by the Na+ channel in the collecting duct |
|
|
1. Heart failure
|
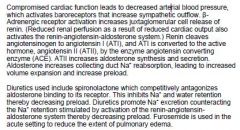
|
|
|
Cirrhosis
|
Cirrhosis is caused by hepatic parenchymal fibrosis resulting from chronic
inflammation or hepatotoxic insult. The fibrotic changes obstruct venous outflow from the liver and increase hydrostatic pressure in the portal vein. Hepatocellular injury disrupts the synthetic and metabolic functions of the liver leading to decreased production of albumin and other contributors to plasma oncotic pressure. Serous fluid accumulates in the abdominal cavity (ascites) which decreases intravascular volume leading to decreased cardiac output leading to increased Na+ retention by a mechanism similar to that described above for heart failure. Diuretics include Spironolactone, loop diuretics and thiazides |
|
|
Nephrotic syndrome
|
Nephrotic syndrome is characterized by massive proteinuria, edema, and
hypoalbuminemia. The primary cause is glomerular dysfunction. The proteinuria leads to decreased plasma oncotic pressure leading to fluid transudation into the interstitium. This transudation decreases intravascular volume ultimately enhancing renal Na+ retention. Diuretics include Spironolactone, loop diuretics and thiazides |
|
|
Carbonic anhydrase inhibitors
|
a. Acute mountain sickness - acetazolamide
b. Glaucoma - dorzolamide c. Restore acid-base balance in heart failure patients with metabolic alkalosis caused by loop diuretics - acetazolamide |
|
|
Osmotic diuretics
|
Reduce intracranial pressure in neurological conditions
|
|
|
Loop diuretics
|
a. Hypercalcemia
b. Hyponatremia (administered with hypertonic saline) c. Counteract hyperkalemia caused by potassium-retaining drugs or renal insufficiency with impaired K+ excretion |
|
|
Thiazides
|
a. Hypertension
b. Nephrolithiasis c. Nephrogenic diabetes insipidus d. Counteract hyperkalemia caused by potassium-retaining drugs or renal insufficiency with impaired K+ excretion |
|
|
Potassium sparing diuretics
|
a. Lithium-induced nephrogenic diabetes insipidus - amiloride
b. Counteract the potassium wasting of thiazide and loop diuretics |

