![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
What do mammary glands develop from |
Ventrolateral ectoderm in wall of embryo which forms the mammary ridge |
|
|
What are the mammary glands |
Modified sweat glands Lovules of glanular tissue surrounding ducts In fibrofatty connective tissue |
|
|
What are ducts lined with |
Bilayer of cuboidal epithelium |
|
|
What are myoepithelial cells |
Present around alveoli and ducts Control milk flow Contract under influence of oxytocin |
|
|
What does the amount of secretory tissue |
Age Pregnancy Lactaitonal status |
|
|
How many teat canals do ruminants have |
1 |
|
|
How many teat canals do pigs and horses have |
2 |
|
|
How many teat canals do cats have |
3-7 |
|
|
How many teat canals do dogs have |
8-14 |
|
|
What is the teat canal lined buy |
Stratified squamous epithelium and waxy material (debris and milk solids) |
|
|
What is the basic function of the mamary gland |
Transfer of passive immunity Nutrient source for neonates |
|
|
What occurs at pubery |
Increase in glandular tissue and duct branching Caused by prolactin and growth factors etc
|
|
|
What occurs at oestrus |
Glandular development and vascular congestion which regresses post oestrus |
|
|
What occurs at lactation |
Accumulation in secretory epithelium Tall and columnar cells before discharge |
|
|
What occurs post lactation |
Involuaiton of the gland |
|
|
What occurs due to damage during lactation |
Ductal epithelial hyperplasia Acinar necrosis and degradation |
|
|
What are the congenital conditions of the mammary glands |
Galactorrhoea - neonatal secretion due to action of maternal hormones (self resolving) Mammary gland or nipple aplasia Inversion or non patency Supenumary teats |
|
|
What does the consequence of congenital conditions depend on? |
Whether the animal is used for breeding or milk production |
|
|
What is bovine hepres mammilitis |
Caused by bovine herpes 2 Ulcerative mammilitis - inflammation of the teat and udder Teat swelling and plain Plaques with centra necrosis Ulceration Regional lymphadenopathy Syncitia of epithelium Eosinophillic inclusion bodies |
|
|
What does bovine herpes 4 cause |
Mammary pustular dermatitis |
|
|
Mastitis |
Inflammation of the mammary gland |
|
|
Routes of infection for mastitis |
Haematogenous Percutaneous Invasion of the teat canal |
|
|
Ranges of clinical involvement |
Acute, subacute, chronic, systemic |
|
|
Microbes involved in mastitis |
Strep Staph Coliforms
|
|
|
What factors contrubute to disease development |
Innate and acquired resistance Teat damage
|
|
|
Pathogenesis of mastitis |
Trauma and cell damage Invasion of udder and prolifection of bacteria Tissue penetration and inflammation Clinical mastitis and sequalae |
|
|
Two categories of mastitis in cattle |
Contageous mastitis - cow to cow transmission Environmental mastitis |
|
|
What is contageous mastitisq |
Bacteria on the skin of the cow that can be passed from one cow to another
|
|
|
What is environmental mastitis |
Contamination of environment Entry via teat canal |
|
|
Contageous masitis and Environmental mastitis bacteria |
Strep uberis Strep dysgalactiae |
|
|
Environmental mastitis pathogen |
E.coli |
|
|
Contageous mastitis pathogens |
Staph aureus |
|
|
Clinical signs of mastitis |
May not show anything - subclinical Marked abnormalitis of the udder Decreased milk production Systemic involvement |
|
|
Acut catharral mastitis |
Hyperaemia, interstitial oedema, lymphatic dialtion, migration of neutrophils, interlobular tissue and alveoli May be sublcinicaal |
|
|
Acute suppurative mastitis |
Organism survives in the ducts and penetrates the connective tussue with the production of purulat material May become chronic e.g. staph |
|
|
Necrotising mastitis |
Organism or toxin penetrates and causes acute necrosis Toxaemia can cause death e.g. Tueperella, arcanobacterium pyogenes |
|
|
Chronic mastitis |
Suppurative or granulomatous Deep invasion Chronic or granulomatous infection Staph, Trueperella,actinobacillus
|
|
|
Endotoxic shock syndrome |
Necrotising vascular damage Endotoxic injury serous inflammation |
|
|
Summer mastitis |
Trueperella pyogenes - sporadic cases of mastitis Necrotising and suppurative inflammation |
|
|
Mycoplasma mastitis |
Sudden agalactia with a firm, swollen and painless gland - arthritis -/+ Emigration of neutrophils Alveolar and duct hyperplasia (chronic cases) |
|
|
Tuberculous masititis |
M. Bovis and usually due to haematogenous infection |
|
|
Predisposing factors for sheep and goat mastitis |
Teat injury Udder chilling and high stocking densities
|
|
|
Common isolates of mastitis in sheep |
Mannheimia Haemolytica Staph aureus |
|
|
Pathology associated with mastitis in sheep |
One gland affected - bluish, watery milk expressed Peracute cases - toxaemia Acute necrotising/gangrenous necrosis results in death (sudden/unexpected) |
|
|
Sequalae to mastitis in sheep |
Sloughing of necrotic tissue or re-established and fibrosis / chronic abscessation |
|
|
Contagious agalactiae |
Mycoplasma agalactiae seen in goats Septicameia Keratoconjunctivitis, arthritis, mastitis Pregnant females may abort or deliver live infected foetuses |
|
|
Maedi visna |
Lentivirus Lungs - pneumonia Bilateral matitisis Lymphoplasmacytic Interstitial and periductal CT |
|
|
Causes of mastitis in goats |
Contageous agalactia Maedi visna Caprine arthritis encephalitis |
|
|
Sow mastitis |
Intensive breeding units Usually husbandry related Coliforms, e.coli and staph
|
|
|
Mastitis - metritis - agalactia syndrom |
occurs 12-48h post partum Lethargy pyrexia, swollen firm mammary glands Colifroms Agalactia also seen |
|
|
bacteria are a commonly used bacterial indicator of sanitary quality of foods and water |
Coliforms |
|
|
Causes of mastitis in dogs and cats |
Strep and staph |
|
|
Mammary masses that are non neoplastic |
Mammary ductular and lobular hyperplasia (bitches and queens) Mammary fibroepithelial hyperplasia - feline mammary hypertrophy Feline mammary fibroadenomatosis, feline firoadenoma or fibroadenomatous hyperplasia
|
|
|
Mammary fibroepithelial hyperplasia |
Seen in young cycling or pregnant queens Treat with syntheic progestagens Regress or require ovariohysterectomy Swelling and erythema, Ulceration and necrosis Proliferation of ductular epitheliu non neoplastic |
|
|
Mammary gland neoplasia |
Usually occurs in older unspayed or late spayed bitches 50% malignant with mets common in lungs and regional LN |
|
|
Mammary neoplasia in the cat |
- malignant in 80-90% Mets to ln,lung,liver
|
|
|
Types of malignant tumours |
Ductular carcinoma In situ carcinoma Simple/complex caricinoma - mixed cell types Mammary sarcoma |
|

|
BHV Mammilitis |
|
|
clots in the milk increased somatic cell count neutrophil macrophages |
|

|
Staph aureus causing gangrenous mastitis Necrosis and eventual sloughing - if animal does not die of systemic disease |
|

|
Mycobacterium Arcanobacterium Staph aureus Actinobacillus |
|
|
Gram negative pathogens cause |
endotoxaemia |
|
|
gram positive pathogens cause |
acute suppurative and chronic purulent mastits |
|

|
Peracute necrotising mastitis |
|

|
Mammary cyst |
|
|
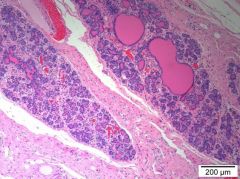
Hyperplasia Duct - pre-neoplastic? |
|

|
Mammary mixed tumour |
|
|
Complex adenoma - myoepithelial cells and tubuloepithelial cells |
|

|
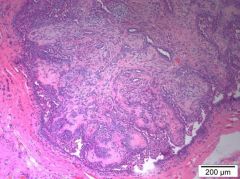
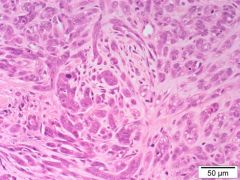
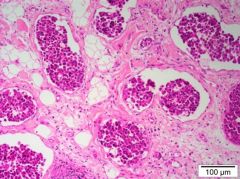
Primary mammary adenocarcinoma |
|
|
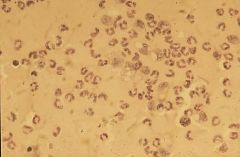
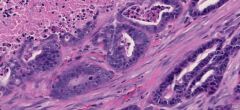
Histology of adenocarcinoma - bizarre mitotic figures |
|
|
Inflammatory mammary carcinoma Involvement of the dermal lymphatics |
|
|
mammary carcinoma note mitotic figs |

