![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
what is hypospadias
|
congenital anomalie where urethral opening on ventral surface of penis
|
|
|
what is epispadias
|
abnormal urethral opening on dorsal surface of penis
|
|
|
what are male genital tract congenital anomalies associated with?
|
failure of normal descent of testes
malformation of urinary tract |
|
|
what can male genital tract congenital abnormalities result in
|
obstruction or sterility
increased risk of ascending urnary tract infection |
|
|
what is phimosis?
|
prepuce(foreskin) too small to permit normal retraction
|
|
|
what causes phimosis
|
secondary to repeated infection that leads to scarring
|
|
|
what is paraphimosis
|
during phimosis, prepuce forcibly retracted leading to marked constriction and swelling of the penis
extremely painful and urethral constiction. |
|
|
what is balanoposthitis
|
infection of the glans and prepuce
usually associated with phimosis chronic accumulation of smegma can be caused by a variety of oranisms: canida anerobes, garnerella, pygenic bacteria |
|
|
what is smegma
|
stuff that is trapped under the foreskin dead skin cells, urine, bacteria, etc
causes inflammation and can lead to cancer. |
|
|
discribe condyloma acuminatum
|
benign epithlial tumor caused by HPV
STD lesions occur around coronal sulcus and inner surface of prepuce sesslie or peduculated red papillary excrescences |
|
|
what types of HPV most commonly cause condyloma acuminatum
|
6, 11
|
|
|
what is the microscopic presentation of condyloma acuminatum
|
branchign, villous, papillary connective tussue stroma caused by hyperplastic epithelium with hyperkeratosis and acanthosis
koilocytes present |
|
|
what are koilocytes
|
clear vacuolization of epithelial cells
halo around affected cells |
|
|
what is carcinoma in situ
|
cancer that has not broken the basement membrane yet
full thickness dysplasia |
|
|
what is characteristic of bowen disease?
|
skin of shaft, usually solitary lesion
thickend gray white or red shiy plaques erythroplasia of queyrat 10% progress to malignancy |
|
|
what is erythroplasia of queyrat
|
seen in bowens disease.
lesions on the glans or prepuce |
|
|
waht is bowenoid papulosis
|
young sexually active adults
multiple reddish brown papular verucoid lesions virtually never develops into cancer |
|
|
what type of HPV are commonly associated with CIS
|
16
|
|
|
discribe squamous cell carcinoma of the penis
|
uncommon
correlated with lack of circumcision HPV type 16 smoking slow growing lesion near coronal sulcus papillary or flat eventually ulcerates and erodes local tissue prognosis related to stage and LN invovlment |
|
|
What is the prognosis for squamous cell carcinoma of the penis if there is LN involvment? if not?
|
27% 5year survival
66% 5 year survival |
|
|
What type of SCC of the penis rarely metasatasizes
|
verrucous carcinoma
has papillary surface growth pattern and a pushing broad border with the dermis underneath, locally invasive |
|
what are these structures?
|
1. leydig cell
2. sertoli cell 3. spermatogonia 4. primary spermatocyte 5. spermatids |
|
|
what is cryptorchidism
|
undescended testes: complete or incompelte failure of the intraabdominal testes to descend into teh scrotal sac by the first year.
1% of mailes may be associated with GU tract malformation asymptomatic often descend later or surgically corrected |
|
|
what are some complications of cryptorchidism
|
increased risk of cancer
death of germ cells increased risk of hernia |
|
|
what is seen on histology of cryptochid tesis
|
thickened basement membrane
leydig cell hyperplasia. atrophy of germ cells |
|
|
which is more common epiddymal or testicualr inflammation?
|
epiddiymal
|
|
|
what is an important cause of orchitis
|
mumps
|
|
|
where in male GU does gonorrhea/TB arise
|
epididymis first then spread to testis
|
|
|
where in male GU does syphilis arise
|
in testis first and then spread to epididymis
|
|
|
what are the nonspecific infections of the testis and epididymis?
|
bacterial UTI
gram neg chlamydia trachomatis neiseria gonorrheoea E. coli and psuedomonas chronic can lead to scarring and infertility |
|
|
what cause granulomatous orchitis
|
autoimmune
unilateral testicaular enlargment in middle aged sudden onset of tender testiscular mass fever confined to region of teh seminiferous tubules |
|
|
discribe testicular torsion
|
vascular distubance secondary to twisting of the spermatic cord and venous obstruction
can occur in absence of injury sudden onsent surgical treatment can lead to gangrene |
|
|
what are the two major groups of testicular tumors
|
germ cell
non germinal |
|
|
what are the types of germ cell tumors?
|
seminoma :seminoma, speratiocytic seminoma
non seminoma: embryonal carcinoma, yolk sac tumor, choriocarcinoma, teratoma |
|
|
what are the types of nongerminal tumors
|
leydig cell tumors
sertoli cell tumor |
|
|
what is the most common testicular tumors
|
germ cell tumors
cause 10% of cancer deaths most common tumor in ages 15-34 males |
|
|
what are the predisposing factors of germ cell tumors
|
cryptorchidism, genetic, (ischoromosome 12;12p) testicular dysgenesis(feminizatrion and klinefelters)
|
|
|
what is the genetic predisposition for germ cell tumors
|
isochromosome 12; 12p)
|
|
|
what is the pathogenisis of germ cell tumors?
|
malignant transformation of germ cells results in intratubular CIS. if these cells cross basement membrane invasive neoplasm develops
tumor can retain features of preimitive gonadocytes in which case it is characterized as seminoma or transfrom into totipotential cell population in which case it is a nonseminomatous tumor |
|
|
which type of germ cell tumor has a worse prognosis?
|
nonseminomatous
|
|
|
what is the microscopic findings for germ cell neoplasia
|
lots of germcells but no maturation all same size
thickened basement membrane |
|
|
what is the presentation of germ cell tumors
|
present with painless enlargment of the testes
|
|
|
what should not be done if germ cell tumor is suspected
|
do not take biopsy could cause tumor spillage so standard management is orchioectomy
|
|
|
what is the first site of lymphatic spread for germ cell tumors
|
para aortic nodes
|
|
|
how does germ cell tumors spread to other organs and in what order?
|
hematogenous spread to lungs most common followed by liver, brain, bones
|
|
|
what is AFP a marker for
|
yolk sac tumor(endodermal sinsu)
|
|
|
what is HCG a marker for
|
choriocarcinoma
|
|
|
what is often elevated in germ cell tumors
|
lactate dehydrogenase
not a specific marker for the testis |
|
|
what is the morphology of the seminoma
|
gross-homogenous gray/whit mass lobulated cut surface replaces entire testicle, tunica albuginea intact
mircoscopic- sheets of uniferm larg polyhedral cells, distinct cells membranes, large central nulceus, one or two prominent nucleoli, abunden clear cytoplasm containing glycogen, background of lymphocytes. contain syncitial giant cells that resemble syncytiotrophoblasts- produce HCG fibrous strands septa infiltrated by lymphocytes granulomas |
|
|
what is the characteristic immunohistochemical finding in seminoma
|
PLAP positive
Cytokarytin negative |
|
|
what are some characteristic of spermatocytic seminoma
|
older patients
indolent never metastasize larger than normal seminoma mixed population of cells PLAP negative. |
|
|
discribe embyronal carcinoma
|
nonseminoma testicular cancer
often compenent of mixed tumor found in 20-30 yo more aggressive than seminoma |
|
|
what is the gross representation of embryonal carcinoma?
|
poorly demarcated gray white mass with hemmorhage and necrosis. may extend through tunica albuginea into epididymis/spermatic cord
|
|
|
what is the micrscopic presentation of embryonal carcinoma
|
glandular, alveolar, tubular, solid, papilary patterns
primitive epithelial cells, considerable size variation, anaplastic, hyperchromatic nuclei, prominent nucleoli, indistince cell borders, mitotic figures |
|
|
what is the immunohistochemistry associated with embryonal carcinoma?
|
CD30
cytokeratin, PLAP |
|
|
discribe the yolk sac endodermal sinus tumor
|
most common testicular tumor in infants and young children
prognosis is good for children under 3 in adults usually a component of mixed tumor grossly appears with homogenous, and yellow/white, with mucinous with areas of hemmorrhage |
|
|
what is the microscopic presentation of yolk sac tumor
|
lacelike network of medium sized cuboidal enlarged cells
structures resembling primitive glomeruli=schiller duval bodies eosinophillic hyaline globules containing AFP and alpha 1 antitrypsin KEY FEATURE |
|
|
what is schiller duval bodies
|
endodermal sinuses which resemble primitive glomeruli
often found in yolk sac (endodermal sinus) tumors |
|
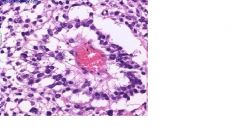
what is this image
|
schiller duval bodies found in yolk sac tumors asscociated with AFP
|
|
|
discribe choriocarcinoma
|
highly malgnant most aggressive type
composed of both cytrophoblast and syncytiotrophoblasts rare less than one percent of germ cell tumors more commonly as part of a mixed germcell tumor can be seen in ovary or placenta as well |
|
|
what is the morpholgy of choriocarcinoma?
|
gross usually small rarely larger than 5cm hemorrhage and necrosis common
|
|
|
what two cell types are most predominant in the microscopic presentation ofchoriocarcinoma?
|
syncytiotrophoblast-large, many irregular or lobular hyperchromatic nuclei and abundant eosinophilic cytoplasm(contains HCG)
cytotrophoblasts- regular polygonal distinct cell membranes, clear cytoplasm, grow in cords or sheets. |
|
|
what is the tumor marke seen in choriocarcinoma
|
HCG
|
|
|
discribe teratoma
|
neoplasm exhibiting evidenc of differentiation into all there germ lines endoderm, mesoderm, ectoderm. therefore tissue from any organ could be seen
can occur at any age pure -children mixed tumor- adults -when found post puperty assumed maligantn with capability to metastasize |
|
|
what is the gross morphology of teratom
|
large, heterogenous with solid, somtimes cartilaginous and cystic areas
|
|
|
what are the three morphological types of teratoma
|
mature- differentiated tisue
immature- elements are incompletely differenctiated, mostly immature neural compenents teratoma with malignant transformatino, shows malignancy in derivatives of nongerm cell types such as presenting with squamous cell carcinoma, adencarcinomae, etc... |
|
|
what is the most common germ cell tumor
|
mixed germ cell tumors
|
|
|
discribe the mixed germ cell tumors?
|
there are variable patterns
-mix of teratoma, embyronal ca, yolk sac, chorionic, metastases can contain any all or new compentents |
|
|
what is a teratocarcinoma
|
a mixed germ cell tumor containing teratoma and embryonoal ca
|
|
|
Discribe the leydig cell tumor
|
approximately 2% of all testicular tumors, usually benign, hormonally active producing androgens and sometimes steroids
males between 20-60 yo |
|
|
how does leydig cell tumor present
|
testicular mass and hormonal changes (gynecomastia, sexual precocity in children)
|
|
|
what is the gross morphology of leydig cell tumor
|
usually less than 5cm in diameter, golden brown homogenous cut surface
|
|
|
what is the microscopic picture of leydig cell tumor
|
large round or polygonal cells with abundant granular eosinophilic cyoplasm and central round nucleus. cytoplasm contians lipid granules and lipofuscin
Crystalloids of reinke in 25% of tumors |
|
|
are leydig cell tumors usually malignant or benign
|
approximatiely 10% are invasive and produce metastasis but most are benign
|
|
|
what does a golden brown cut surface usually indicate on gross tissue examination
|
steroid producing
|
|
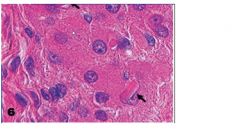
what is this a picture of and what is assocaited with
|
reinke crystals are found in 25% of leydig cell tumors
|
|
|
what are some characteristics of sertoli cell tumor (androblastoma)
|
rare testicular tumors, usually benign, hormonally active, but rarely in suffiencet quantity to produce feminization or precocious masculinizatino
often in middle aged men |
|
|
what is the gross morphology of sertoli cell tumors
|
less than 3cm in diabmeter,
well cricumscribed solid , gray white cut surface |
|
|
what is the microscopic presenation of sertoli cell tumors
|
tumors cells arragned in distinctive trabeculae with a tendency to form cordlike structures resembling immature seminiferous tubuels
tall columnoar cells |
|
|
what ist he clinical manifestion of sertoli cell tumors
|
most are benign
varent with annular tubuels associated with Peutz Jghers syndrome |
|
|
what are the characteristics of testicular lymphoma
|
leuikemia can spread to testes but its rare for primary lymphoma of testes to arise
more common in men older than 60 usually has already spread at time of discovery usually diffuse large B cell lymphoma poor prognosis |
|
|
what are 5 acute conditions of the tunica baginalis
|
hydrocele-serous fluid
hematocele- blood chylocele- lymph speratocele- semen varicocele- dilated vein filled with blood |
|
|
what is the size of a normal prostate
|
20gms
|
|
|
what are the 4 biologically and anatomically distinct lobes
|
peripheral
central transitional periurthral different lesions arise in each area |
|
|
which lobe of the prostate do most cancers arise? what about hyperplasias?
|
cancer=peripheral
hyperplasia=transitional |
|
|
what is the cause of acute prostatitis
|
ecoli, enterococci, staphlococci,
UTI , catheterization |
|
|
what is the presentation of acue prstatitis
|
fever, chills, dysuria, tender boggy prostate
|
|
|
what is the cause for chronic prostatitis
|
associated with recuurent UTI
|
|
|
what is the presentation and testing in chronic prostatitis
|
asymptomatic or low back pain, perineal discomfort dysuria.
leukocytes in prostatic secretion with postiive cultires. |
|
|
what is the presentation of chronic abacterial prostatitis
|
negative bacterial cultures
sexually active male similar presnetion of chronic bacterial prostatis but no hx of recurrent UTI greater than 10 leukocytes per HPF of prostaic secretion |
|
|
what is granulomatous prostatis associated with?
|
in US related to bladder Rx with BCG(attenuated tuberculous strain) for superficial cancer
|
|
|
what is nodular hyperlasi
|
benign prostatic hyperplasia
extermely common in men over 50 periurethral in location(transitional zone) may cause partial to complete urethral obsturciton |
|
|
how is nodular hyperplasi caused
|
hormone dihydrotesterone causes release of growthfactor
|
|
|
what is the gross morphology of nodular hyperplasia(BFH)
|
orginates almost exclusively in the inner aspec of the prostate gland transurethral and periurethral zone(transitiona lobe)
nodules are yllow /pink gray |
|
|
what is the microscopic presentation of BGH
|
glandular epithelial and fibromuscular stromal proliferation
epithelila include papillary bud and infoldings glands lined by 2 cell layer cysts, squamous metaplasia, infarcts not premalignant lesion |
|
|
what is the clinical presentation of nodular hyperplasia
|
increased urinary frequency, nocturiam difficulty startinga and stoping
acute urinary retention |
|
|
what is a hint that there could be cancer in prostate biopsy?
|
large nuclie in the glandular tissue
|
|
|
what is the most common cancer in men
|
prostat adenocarcinoma
also second leading cause of cancer death |
|
|
what are the risk factors for prostate adenocaarcinoma?
|
men over 50
blacks more than whites rare in asians genetics/familiy history hormaone levels envrionmental influences |
|
|
what is the gross presentation of prostate adenocarcinoma
|
occurs in the peripheral zone, usually posterior region.
can often be palpated on rectal exam cut surface gritty/firm, yellowish poorly demarcated lesion |
|
|
what is the microscopic presentation of prostate adenocrcinoma
|
NO BASAL MYOEPITHELIAL CELL LAYER
nuclei large, irregular vacuolated malignant acini arranged back to back capsular and perineural invasion -INDICATE MALIGNANCY may have adjacent precurso lesion prostatic intraepithelial neoplasi myoepithelial layer is retained buy patchy |
|
|
how is prostate adenocarcinoma graded
|
gleason grading
graded by how well differentiated the glandular pattern is. the more differentiated the lower the grade. 1-glands tight together 2-glands starting to loosen 3- 4-cryptaforming 5-sheets most tumors have more than one pattern so you take the primary and secondary patterns seen and combine their score 1 being the most differntiated and 5 being the least. 2-4-well differentiated 5-6 intermediate grade 7 - moderate to poorly differentiated 8-10 high grade. |
|
|
what is the clinical presentation of prostat adenocarcinoma
|
often asymptomatic detected on rectal exam or elevated PSA
in advanced diease there will be urinary obstuction back pain- because of osteoblastic bony metastases via hematogenous spread |
|
|
where does prostate adenocancer tend to spread first
|
obturator nodes
|
|
|
how is prostatic adenocarcinoma treated
|
surgical removal, radiotherapy and hormonal manipulation.
|
|
|
what is the marker for prostat cancer
|
PSA
also elevated in nodular hyperplasia!!!! but levels tend to be lower than in cancer LEVEL ABOVE 4ng/mL |

