![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
ANTI-COAGULATION DRUGS
OVERVIEW - list the 3 categories of Anti-coagulation Drugs |
(THC)
- Thrombolytics (direct-acting) - Heparin + heparin derivatives - Coumarins (i.e. - Warfarin) |
|
|
WARFARIN
- Warfarin is what kind of derivative? |
- Coumarin derivative
|
|
|
WARFARIN
- Interferes with the _____ process of the ______ dependent clotting factors at the _______ location. |
- Synthesis
- Vitamin K - Liver |
|
|
WARFARIN
- Liver synthesizes what Vitamin K dependent Coagulation factors. x4 - Liver synthesizes what Vitamin K dependent ANTI-coagulation proteins? x3 |
- Factor II (2)
- Factor VII (7) - Factor IX (9) - Factor X (10) - Factor C - Factor S - Factor Z |
|
|
WARFARIN
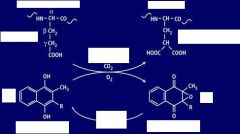
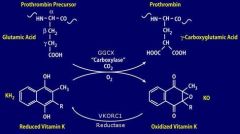
- Vit. K dependent clotting factors undergo what reaction TYPE at the liver? - what Enzyme does this? |
- Glutamate Carboxylation
- GGCX (Gamma Glutamyl CarboXylase) |
|
|
WARFARIN
- What are the Reactants (x2) in the Vit. K dependent clotting factor reaction? - What are the Products? (x2) |
- Prothrombin Precursor
- Reduced Vit. K - Prothromin - Oxidized Vit. K |
|
|
WARFARIN
- For the Vit. K dependent clotting factor reaction, what is the other essential LINKING reaction? - what TYPE of reaction is this? - Enzyme responsible? |
- "REcycling" or REducing of Oxidized Vitamin K
- Reduction - VKORC1 (Vit. K epOxide Reductase Complex 1) |
|
|
WARFARIN
- For "REcycling" Vit. K, what is the reactant? - Product? - Enzyme? - Describe the molecular change |
- Oxidized Vit. K
- Reduced Vit. K - VKORC1 - KO (oxid. VK) --> KH2 (red. VK) |
|
|
WARFARIN
- in the Vit. K dependent clotting factor reaction, describe the chemical change seen for both both products. |
1.) Glutamic acid (precursor)
--> gamma-Carboxyglutamic acid (Prothrombin) 2.) KH2 (red. Vit. K) --> KO (oxid. vit. K) |
|
|
WARFARIN
- What is Factor II? - What is Factor IIa? - What is Factor I? - What is Factor Ia? - Warfarin causes the reduced levels of what Factor? |
- Prothrombin (activated by V, becomes)
- Thrombin (will activate -->) - Fibrinogen (which becomes) - Fibrin - Prothrombin |
|
|
WARFARIN
- Warfarin inhibits which enzyme? - so direct accumulation of? - and reduced levels of? |
- VKORC1
(Vit. K epOxide Reductase Complex 1) - Oxidized Vitamin K - Reduced Vitamin K |
|
|
WARFARIN
- why is Vitamin K in its Reduced form so important? |
- Vit. K is the CoFactor of GGCX
and the reduced form is the only form accepted by GGCX |
|
|
|
|
|
WARFARIN
- Administration? - Absorption? |
- PO
- Rapid & Complete |
|
|
WARFARIN
- Distribution? - Vd value? |
- Plasma protein binding = 99%
- small |
|
|
WARFARIN
- Metabolism by? - Half life? |
- Hepatic CYP2 C9
- 40 hours |
|
|
WARFARIN
- Onset? - Duration? |
- 2 to 3 days
- 2 to 5 days |
|
|
WARFARIN
- what are the major side effects? |
(WAR is broadcast by the BBC)
- Bleeding - Birth Defects - Cutaneous necrosis |
|
|
WARFARIN
- out of the Major side effect, which is the MAIN concern? - what can be given to combat this Major Side Effect? x3 |
- Bleeding
- Vitamin K - Clotting Factors - Fresh Frozen Plasma |
|
|
WARFARIN
- why is Warfarin contraindicated in pregnant women? - Warfarin is teratogenic during what weeks of pregnancy? |
- Crosses the Placenta
- weeks 6 to 12 |
|
|
WARFARIN
- if given to pregnant chick, compare the drug concentrations in mom vs. fetus. |
- [maternal] = [fetus]
|
|
|
WARFARIN
T/F : Warfarin is found breast milk T/F : Other Coumadins are found in breast milk. |
- False
(Warfarin is NOT found in breast milk) - True (other Coumadins are found in breast milk) |
|
|
WARFARIN
- list some non-major side effects x7 |
(DA FAUNA)
- Dermatitis - Abdominal cramps - Fever - Alopecia - Urticaria - N/V/D - Anorexia |
|
|
DRUG INTERACTIONS
- when administering another drug with Warfarin, what type of monitoring is necessary? |
- Prothrombin time (PT)
|
|
|
DRUG INTERACTIONS
With Warfarin, an INCREASED Anti-Coagulation would occur when mixing with drugs that: - Displace......... - Increase........ - Decrease......... - Inhibit........... x2 |
- Displace Plasma Protein bound Warfarin
- Increase the Affinity of the Warfarin "receptor site" - Decrease the Bioavailability of Vitamin K - Inhibit the Liver Microsomal Enzyme System - Inhibit the Platelet Function |
|
|
DRUG INTERACTIONS
With Warfarin, a DECREASED Anti-Coagulation would occur when mixing with drugs that: - Stimulate........... x2 - Inhibit........... |
- Stimulate the Liver Microsomal Enzyme System
- Stimulate the Clotting Factor synthesis - Inhibition of Absorption |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Displace Plasma Protein bound Warfarin, will have what effect on Anti-coagulation? - why? - drug example that does this |
- Increase Anti-coagulation
- b/c of the high degree of Warfarin bound to proteins, even a small decrease in the amount bound can lead to significant increase in free active drug levels - Salicylates such as ASA |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Inhibit Liver Microsomal Enzyme System will have what effect on Anti-coagulation? - why? - drug example that does this |
- Increase Anti-Coagulation
- Decreased metabolism will lead to increased Bioavailabiity of Warfarin - Quinidine |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Increase the Warfarin "Receptor site" affinity, will have what effect on Anti-coagulation? - why? - drug example that does this |
- Increase Anti-Coagulation
- Increased Efficacy of Warfarin at given plasma levels - d-Thyroxine |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Stimulate the Liver Microsomal Enzyme System, will have what effect on Anti-coagulation? - why? - drug example that does this |
- Decreases Anti-coagulation
- Decreases plasma half-life of Warfarin - Barbiturates |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Stimulate Clotting Factor synthesis, will have what effect on Anti-coagulation? - why? - drug example that does this? x2 |
- Decrease Anti-Coagulation
- Antagonizes Warfarin activity - Vitamin K - Estrogens |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Reduce the Availability of Vitamin K, will have what effect on Anti-coagulation? - drug example that does this? x2 |
- Increase Anti-Coagulation
- Broad Spectrum Antibiotics - Laxatives |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Inhibit platelet functioning, will have what effect on Anti-coagulation? - drug example that does this |
- Increase Anti-Coagulation
- ASA |
|
|
DRUG INTERACTIONS
- Mixing Warfarin with drugs that Inhibit Absorption, will have what effect on Anti-coagulation? - drug example that does this |
- Decrease Anti-Coagulation
- Cholestyramine |
|
|
DRUG INTERACTIONS
Warfarin + d-Thyroxine = ? why? |
- Increases Anti-coagulation
- D-thyroxine increases the Affinity of warfarin receptor sites, thus increasing efficacy at a given plasma level |
|
|
DRUG INTERACTIONS
Warfarin + ASA = ? why? |
- Increase Anti-Coagulation
- Displaces Plasma Protein bound Warfarin - Inhibits Platelet functioning |
|
|
DRUG INTERACTIONS
Warfarin + Quinidine = ? why? |
- Increases Anti-Coagulation
- Quinidine Inhibits Liver Microsomal Enzyme system |
|
|
DRUG INTERACTIONS
Warfarin + Broad Spectrum Ab = ? why? |
- Increased Anti-Coagulation
- Decreases the Vitamin K bioavailability |
|
|
DRUG INTERACTIONS
Warfarin + Laxatives = ? why? |
- Increases the Anti-coagulation
- Reduces the Vitamin K bioavailability |
|
|
DRUG INTERACTIONS
Warfarin + Barbiturates = ? why? |
- Decreases the Anti-coagulation
- Barbiturates Stimulate the Liver Microsomal Enzyme system. Thus decreasing warfarin half life. |
|
|
DRUG INTERACTIONS
Warfarin + Vitamin K= ? why? |
- Decreases the Anti-coagulation
- antagonizes warfarin activity |
|
|
DRUG INTERACTIONS
Warfarin + Estrogens = ? why? |
- Decreases the Anti-coagulation
- antagonizes warfarin activity |
|
|
DRUG INTERACTIONS
Warfarin + Cholestyramine = ? why? |
- Decreases the Anti-coagulation
- Inhibits absorption |
|
|
WARFARIN TIDBITS
- Warfarin would affect what lab test and how? - why so? |
- Prolonged PT
- due to deficiency in Factor SEVEN (PTT stays fine cuz factor 12 don't change nun) |
|
|
WARFARIN TIDBITS
- why would Warfarin cause cutaneous necrosis? |
- results from microvascular thrombosis caused by Deficiency in Vitamin K dependent ANTI-coagulant proteins C & S.
(think "C" for "C"utaneous necrosis) |
|
|
HEPARIN
- describe its Molecular Weight - describe its structure - where are Heparin found? |
2 to 40 kDa
N- & O- sulfated sugars polymerized by glycoside bonds Secretory granules of Mast Cells |
|
|
HEPARIN
- which Heparins possess most of the biological activity? |
- Lower MW polymers of Heparin
|
|
|
HEPARIN
- describe the activity of heparin in vitro vs. in vivo - describe its acidity - describe its absorbance following PO |
- Active in vitro and in vivo
- most acidic organic acid in the body - NOT absorbed following oral administration |
|
|
HEPARIN
- Heparin forms a complex by binding to what enzyme? - this combined complex can then bind to what? (thus forming what complex?) - what is the end enzymatic effect? - thus the enzymatic effects of Heparin affects coagulation how? |
- Binds & Activates AT III
(Anti-Thrombin III) - Serine Protease (forming the ternary complex) - Serine Protease is inhibited - Accelerates the Inactivation of Clotting Factors IIa (2a), Xa (10a), IXa (9a), XIa (11a), XIIa (12a) |
|
|
HEPARIN
- what type of enzyme is AT III? - AT III is endogenous or exogenous? - AT III inactivates what clotting factors? x5 - is this inactivation reversible or irreversible? |
- Serine Protease Inhibitor
(when activated by Heparin) - AT III is Endogenous - Factors IIa (2a), Xa (10a), IXa (9a), XIa (11a), XIIa (12a) - Irreversible |
|
|
HEPARIN
- what unique sequence of Heparin binds to AT III with high affinity - what F(x)'al group in the above sequence is required in binding? - what is also required for UNFRACTIONATED Heparin - what about for LOW MOLECULAR WEIGHT Heparin (LMWH) |
- PENTA-saccharide sequence
- Sulfate groups (-SO3-) - Polysaccharide of at least 18 units is required - 5 units for LMWH |
|
UNFRACTIONATED HEPARIN
Explain what is going on here. |
1.) AT III + Heparin
2.) Activated AT III will bind to Serine Protease 3.) Formation of Ternary complex 4.) Inactive Serine Protease bound to AT III 5.) Heparin released from the Ternary complex is free to bind and activate other AT III |
|
|
LOW MOLECULAR WEIGHT HEPARIN
- MW? - LMWH-AT III complex Preferentially binds to? |
- 4,000 Dalton to 6,000 Dalton
- Factor Xa (10a) (via AT III & not the LMWH) |
|
|
LOW MOLECULAR WEIGHT HEPARIN
- compare half life vs unfractionated Heparin - compare side effects vs unfractionated Heparin |
- double the half life
- less bleeding |
|
|
LOW MOLECULAR WEIGHT HEPARIN
- LMWH has Less Effect on what Anti-coagulation processes when compared to Unfractionated Heparin. x2 |
- Less Effect on Platelet Activation
- Less Effect on Factor XIII (13) Activation |
|
|
UNFRACTIONATED HEPARIN
- monosaccharide units? - binding components? LOW MOLECULAR WEIGHT HEPARIN - monosaccharide units? - binding components? |
UNFRACTIONATED HEPARIN
>= 18 monosaccharide units Heparin binds ATIII & Factor IIa (2a) Factor IIa (2a) also binds to AT III LMWH < 18 monosaccharide units (minimum 5 required) LMWH binds to AT III only Factor Xa (10a) binds to AT III only (& not LMWH) |
|
|
HEPARIN PHARMACOKINETICS
- administration - distribution |
- IV or SubQ
(no oral absorption) - Vd is small due to extensive binding |
|
|
HEPARIN PHARMACOKINETICS
- onset for IV - onset SubQ - Duration |
- immediate
- 20 to 60 minutes - less than 2 hours |
|
|
HEPARIN SIDE EFFECTS
- what is the main concern - what is the antidote |
- Bleeding
- Protamine Sulfate |
|
|
HEPARIN SIDE EFFECTS
- 1% to 5% of Heparin patients suffers from what condition? - results from the formation of what? - the complex formed above will bind to what? - above binding will lead to inappropriate formation of? |
Rapid & Profound Thrombocytopenia
(w/ paradoxical arterial or venous thrombosis) - Ab directed against platelet Factor IV (4) complexed w/ Heparin - Heparin-Ab complex binds to Platelets - Aggregation & Thrombous formation |
|
|
HEPARIN SIDE EFFECTS
- patients on Heparin for 6 months may suffer from? - usually accompanied with how much dosage? |
- Reversible Osteoporosis
- 6 months therapy w/ >15,000 U/day |
|

What type of Heparin is this?
# of Monosaccharide units? |

LMWH
< 18 monosaccharide units |
|

What kind of Heparin is this?
# of monosaccharide units? |

Unfractionated Heparin
> than 18 monosaccharide units |
|
|
ANTI-PLATELET DRUGS
- list 3 anti-platelet drugs |
- ASA
- Clopidogrel - Glycoprotein IIb / IIIa inhibitors |
|
|
ASPIRIN
- MOA will Inactivate? - via what reaction? - Irreversible or Reversible |
- inactivates Cyclooxygenase
by - Covalent Acetylation is - Irreversible |
|
|
ASPIRIN
- ASA inhibits what Constitutively? - ASA inhibits what in Induced way? |
- COX-1
(prostaglandin G/H synthase 1) - COX-2 (prostaglandin G/H synthase 2) |
|
|
ASPIRIN
- ASA inhibition of COX will lead to the inhibition of what important Platelet Aggregator? |
- Thromboxane A2
(TxA2) |
|
|
ASPIRIN
- Selectivity of ASA occurs for COX where? |
- Platelet COX
|
|
|
ASPIRIN
- Platelet COX is ______ in the ______ circulation BEFORE or AFTER - ASA is ________ in the _____ |
- Acetylated
- Portal Circulation BEFORE - Deacylated - Liver |
|
|
ASPIRIN
- the selectivity of ASA for platelet COX means that the Systemic Vasculature is unaffected because? |
- Platelets are NOT affected by Salicylate
|
|
|
ASPIRIN PHARMACOKINETICS
- Absorption - Distribution in Low doses - Distribution in High doses |
- 70%
- mostly bound to plasma protein - smaller % is plasma protein bound (thus more available to tissues) |
|
|
ASPIRIN PHARMACOKINETICS
- Elimination by what? and what %? - what is excreted and how? |
- Hepatic Metabolites (75%)
- Parental compound excreted - via Urine |
|
|
ASPIRIN PHARMACOKINETICS
- Onset? - Duration? |
- 30 minutes
- 7 to 10 days |
|
|
ASA ADVERSE ACTIONS
- primarily occurs in what system? - give 3 examples of major side effects - list other minor side effects x5 |
- GI
- Epigastric pain (heartburn, nausea) - GI blood loss - Gastric Ulcers (GRANT) - Gout - Rash - Acid-base disturbance - Nasal polyps - Tinnitus |
|
|
ASPIRIN INTERACTIONS
- Decreases the effectiveness of what drugs? - though usually not a problem if? |
- Anti-Hypertensives
- with Low doses, not a problem |
|
|
ASPIRIN INTERACTIONS
- Increases the effects of what drug? |
- Warfarin
|
|
|
ASPIRIN INTERACTIONS
- Attenuates the actions of what drugs? - give example |
- Uricosuric agents
- Probenecid |
|
|
OTHER ANTI-PLATELETS
- list 2 other Anti-platelet drugs - what is their MOA? - thus, the MOA will have what effect on cAMP? |
- Ticlopidine
- Clopidogrel - P2Y2 Purine Receptor Antagonists - Increase cAMP (thus decrease aggregation) |
|
|
TICLOPIDINE & CLOPIDOGREL
- will reduce the incidence of? x2 - currently the drug of choice in? x2 - particularly effective when combined with? |
- MI
- CVA - Prophylaxis of Subacute Stent Thrombosis - Post-Ischemic Stroke Tx - ASA |
|
|
GLYCOPROTEIN IIb/IIIa INHIBITORS
- list 3 |
- Abciximab
- Tirofiban - Eptifibatide |
|
|
GLYCOPROTEIN IIb/IIIa INHIBITORS
- what type of compound is Abciximab? - Tirofiban? - Eptifibatide? |
- Fab fragment
(directed to GP IIb/IIIa receptor) - NonPeptide Inhibitor (of GP IIb/IIIa receptor) - Cyclic Peptide (GP IIb/IIIa receptor antagonist) |
|
|
FIBRINOLYTICS
- restores blood flow to an Injured area by ....? |
- lysing Thrombus into Soluble Fibrin Degradation products
|
|
|
FIBRINOLYTICS
- give 4 examples |
(Alt USA)
- Alteplase (rtPA) - Urokinase - Streptokinase - Anistreplase |
|
|
FIBRINOLYTICS
- MOA? |
- accelerates the conversion of Plasminogen to Plasmin
|
|
|
FIBRINOLYTICS
- Plasmin is what type of enzyme? - functionally does what? |
- Protease
- Breaks down Fibrinogen & Fibrin into degradation products |
|
|
FIBRINOLYTICS
- the major M&M of ThromboEmbolic Dz is due to? - thus leading to? |
- Vascular occlusion
- Ischemia & Infarction |
|
|
FIBRINOLYTICS
- what is the purpose and Tx goal? |
- Rapid Reperfusion of Infarcted area preserves more tissue.
|
|
|
FIBRINOLYTICS
- Fibrinolytic success is Dependent upon what? |
- Time lapse btw onset of Sx & administration of fibrinolytic
|
|
|
FIBRINOLYTICS
Time Lapse btw Sx onset & Fibrinolytic administration for: - DVT? - PE? - MI - CVA (stroke)? |
DVT: <= 7 days
PE: <= 2 days MI: 2 to 4 hours Stroke : < 3 hours |
|
|
FIBRINOLYTICS
- Major side effect? |
- Bleeding
|

