![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
134 Cards in this Set
- Front
- Back
|
All areas of the GI tract have basically the same 4 histological layers. Name em and their components.
|
Mucosa (comprised of epithelium, lamina propria, muscularis mucosa)
Submucosa (classified as dense irregular CT, Meissner's plexi) Muscularis externa (inner circular and outer longitudinal layers of smooth muscle w/ Auerbach's (myenteric) plexus between the layers. Adventitia (dense irregular CT, blood vessels, lymphatics and nerve fibers) p. 169,70 |
|
|
Which component of the GI tract mucosa is avascular and sits on a basement membrane?
A. Epithelium B. Lamina propria C. Muscularis mucosa |
A. Epithleium
p. 169 |
|
|
This layer of the GI tract is composed of collagen and elastic fibers, has occasional areas of diffuse and nodular lymphoid tissue, can contain exocrine glands, and contains small blood vessels, nerves and lymphatics.
A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
C. Lamina propria (of mucosa layer)
p. 169 |
|
|
The _______'s contractions helps empty glands of mucosa and helps transport material along the GI tract tube.
A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
E. Muscularis mucosa
p. 169 |
|
|
This component of the mucosa has its greatest relative thickness in the esophagus.
A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
E. Muscularis mucosa
p. 169 |
|
|
This layer of mucosa is innervated by post-ganglionic parasympathetic fibers originating from Meissner's plexus.
A. Epithelium B. Lamina propria C. Muscularis mucosa |
C. Muscularis mucosa
p. 169 |
|
|
Which GI tract histological layer has the following characteristics:
- classified as dense irregular CT - large plexi of blood vessels and lymphatics, nerves and Meissner's plexi (pre-ganglionic fibers from Vagus nerve) |
Submucosa
p. 169 |
|
|
In what two areas of the GI tract are there glands in the submucosa?
|
The submucosa ONLY has glands in two areas of the GI tract: dudodenum and esophagus.
p. 169-70 |
|
|
True or False:
There are glands in the submucosa of the pancreatic and duodenal organs. |
FALSE. The submucosa glands only occur in the duodenum and esophagus.
p. 169 |
|
|
Name the layers of the GI tract from innermost to outermost. Include the components of the mucosa.
|
"MUCOSA" = epithelium --> lamina propria --> muscualris mucosa --> SUBMUCOSA --> MUSCULARIS EXTERNA --> ADVENTITIA
p. 169 |
|
|
The muscularis externa is formed of smooth muscle except in [where]?
|
the upper esophagus. There it is actually some skeletal muscle!
p. 170 |
|
|
True or False:
Muscularis externa is innervated by post-ganglionic parasympathetic fibers originating from Meissner's plexus. |
FALSE. originates from Auerbach's (myenteric) plexus located between its two muscle layers.
p. 170 |
|
|
Which GI histological layer has these features?
- Has inner circular and outer longitudinal layers. - Innervated by post-ganglionic parasympathetic fibers originating from Auerbach's (myenteric) plexus - functions mainly inperistalsis |
Muscularis externa.
p. 170 |
|
|
Which layer does this describe:
Function is conduction, absorption and secretion in the GI tract. A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
B Epithelium
p. 169 |
|
|
Which layer does this describe:
Innervated by post-ganglionic parasympathetic fibers originating from Meissner's plexus. A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
E. Muscularis mucosa
p. 169 |
|
|
Which layer does this describe:
Functions mainly in peristalsis A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
D. Muscularis externa
maintains tonus and propels food onward. Circular layer controls caliber of lumen, also churns and propels food along. Longitudinal muscle contraction shortens tube locally. p. 170 |
|
|
Which layer does this describe:
When covered with visceral peritoneum is called a serosa. A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
A. Adventitia
p. 170 |
|
|
Which layer does this describe:
Innervated by post-ganglionic parasympathetic fibers originating from Auerbach's (myenteric) plexus. A. Adventitia B Epithelium C. Lamina propria D. Muscularis externa E. Muscularis mucosa F. Submucosa |
D. Muscularis externa
Myenteric plexus is located between the inner circular and outer longitudinal muscle layers of the muscualris externa layer. p. 170 |
|
|
The myenteric plexus innervates [ muscularis externis / muscularis mucosa ] while the Meissner's plexus innervates [ muscularis externis / muscularis mucosa ].
|
Myenteric plexus = muscularis externis
Meissner's plexus = muscularis mucosa |
|
|
True or False:
The entirety of the esophagus is intrathoracic. |
False. The first ~10 inches are, but the last ~ 1 inch has visceral peritoneum becuase it does jut into the peritoneal cavity a little bit.
p. 170 |
|
|
Regarding the esophagus' innervation, the smooth muscle layers are innervated by..... while the vascular smooth muscle is innervated by.... and the skeletal muscle by.....
A. efferent fibers of Vagus nerve B. postganglionic parasympathetics from Meissner's and Auerbach's plexi C. postganglionic parasympathetics from cervical and thoracic sympathetic trunks |
B, C, A respectively
SMOOTH MUSCLE = postganglionic parasympathetics from Meissner's and Auerbach's plexi VASCULAR SMOOTH MUSCLE = postganglionic parasympathetics from cervical and thoracic sympathetic trunks SKELETAL MUSCLE= efferent fibers of Vagus nerve p. 170 |
|
|
True or False:
The esophagus functions as purely a food conveyor from oropharynx to stomach. It does not secrete mucus for lubrication of food. |
False. Yes it functions to convey food, but it does have glands that secrete mucus for lubrication!
p. 170 |
|
|
In the esophagus, the muscularis mucosa is mostly
A. circularly oriented B. thickest in the upper portion due to skeletal muscle C. innervated by postganglionic fibers from Auerbach's plexus D. occurs in discreet bundles in the upper portion |
D. occurs in discreet bundles in the upper portion
p. 170 |
|
|
In the esophagus, which histological layer
- contributes to large longitudinal folds of the esophagus that smooth out during swallowing - contains compound tubuloalveolar, mucus secreting |
submucosa
p. 171 |
|
|
What kind of glands are in the esophagus' submucosa?
|
compound tubuloalveolar glands that secrete mucus!
p. 171 |
|
|
Which histological layer of the esophagus "determines" the level of histological section? How so?
|
The muscularis externa. Upper 1/3 is composed of almost all skeletal muscle. Middle 1/3 is composed of a mix of smooth and skeletal muscle. Lowest 1/3 is composed only of smooth muscle. p.171
|
|
|
True or False:
The esophageal-stomach junction's anatomical sphincter prevents regurgitation of the stomach contents. |
FALSE. There is an anatomical sphincter here, but it is not anatomical, it is physiological.
p. 171 |
|
|
Which three things were given as examples that relax the sphincter and can help one feel less "full" after a meal?
|
Alcohol, nicotine, peppermint.
p. 171 |
|
|
In the esophagus' muscularis externa layer, the smooth muscle is innervated by .... and skeletal muscle by....
|
SMOOTH MUSCLE = postganglionic parasympathetics from Auerbach's plexus
SKELETAL MUSCLE = spinal nerves p. 171 |
|
|
Which histological layer of the esophagus does this describe?
- intrathoracic portion blends with surrounding dense irregular CT - below diaphragm covered with visceral peritoneum |
adventitia
p. 171 |
|
|
The stomach acidifies and converts swallowed food into a viscous fluid called __________.
|
chyme
p .171 |
|
|
True or False:
The esophagus' mucosa produces digestive enzymes. |
FALSE. Just lubricating mucosa.
p. 170 |
|
|
What are the four gross anatomic divisions and three histological divisions of the stomach?
|
4 gross: cardiac, fundus, body, pyloric
3 histo: cardiac, fundic (fundus + body area), pyloric based on gland structure p. 172 |
|
|
True or False:
There are no sharp divisions between the stomach's three histological areas. |
True. The three areas (cardiac, fundic, pyloric) all differ with respect to gland structure but there is no distinct demarcation where one area begins and another stops. p. 172
|
|
|
What are rugae?
|
Rugae are large longitudinal folds formed by the mucosa and submucosa in the stomach. They are most prominent when the stomach is empty.
|
|
|
In the stomach, the rugae are formed by which histological layer(s)?
|
mucosa and submucosa
p. 172 |
|
|
In the esophageal-gastric junction, there is an abrupt change from _______ to _______ regarding the epithelium.
A. stratified simple squamous to simple columnar cells B. stratified cuboidal to simple columnar cells C. stratified simple squamous to stratified columnar cells |
A. stratified simple squamous to simple columnar cells
p. 172 |
|
|
The stomach's mucosa has ______ ,which are fine furrows lined by simple columnar epithelium that that lead into / forms sheet glands which are all mucus secreting.
A. gastric pits B. rugae |
gastric pits
p. 172 |
|
|
True or False:
Stomach's mucosa is acidic to aid in digestion of food boluses. |
FALSE. The mucus is actually basic to counteract the acidity! The basic pH forms protective barrier from strong acidity of stomach content. Cells are continuously sloughed off and survive only ~ 3 days. p.172
|
|
|
True or False:
The glands of the stomach are all simple, branched tubular glands that occupy the entire thickness of the mucosa. |
True! All three types of glands in the stomach (gastric glands = cardiac, fundic, pyloric glands) are all simple, branched tubular glands that tend to occupy the entire thickness of mucosa. They differ in the proportion of neck, body and base lengths.
p. 172 |
|
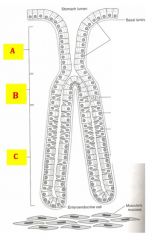
Identify the parts of the gastric gland diagrammed.
|

|
|
|
Each gastric gland can be divied up into three parts. What are those parts?
|
Neck, body, and base.
p. 172 |
|
|
All gastric glands are classified as...
|
simple branched tubular glands
p. 172 |
|
|
What histological layer component occupies the space between the gastric glands and gastric pits?
|
Lamina propria
p. 172 |
|
|
Which gastric gland does this describe:
- length of gland approximately equal to depth of pit - composed of mostly mucus secreting cells with few parietal and enteroendocrine cells - primary function is to produce a protective mucus secretion |
Cardiac glands
p. 173 |
|
|
Which gastric gland does this describe:
- one or more open into each gastric pit, short pits and deep glands - are closely packed and orientated perpendicular to surface - are major source of gastric juice - composed of mucous neck cells, parietal cells, chief cells, enteroendocrine cells |
Fundic glands
p. 173 |
|
|
Which gastric gland does this describe:
- pit seems much longer than gland - gland is simple, branched tubular which are very coiled - composed completely of mucus secreting cells with a few parietal cells and enteroendocrine cells |
Pyloric glands
p. 174 |
|
|
Regarding gastric glands, identify each by
A. the pit length: gland length B. the cells they are composed of C. their main function(s) |
A. Cardiac gland length: 1:1, Fundic gland: short pits, deep glands , Pyloric gland: deep pits, short glands
B. Both cardiac and pyloric glands are mostly mucus secreting with few parietal and enteroendocrine cells. Fundic glands are composed mucus cells primarily in the neck region and then parietal cells in the upper region, chief cells predominantly in the lower half of glands, and enteroendocrine cells at base of glands C. Cardiac: protective mucus secretion, Fundic: major source of gastric juice, Pyloric: protective mucus p. 174 |
|
|
Regarding gastric glands, identify each by the following:
A. deep pits, short glands B. short pits, deep glands C. Pit and gland length roughly equal |
A. pyloric gland
B. fundic gland C. cardiac gland p. 174 |
|
|
This gastric gland is composed of mucus cells primarily in the neck region and then parietal cells in the upper region, chief cells predominantly in the lower half of glands, and enteroendocrine cells at base of the gland.
|
Fundic gland
p. 174 |
|
|
The fundic gland is composed of various cells at different points of the gland. Where is each?
- chief cells - enteroendocrine cells - mucus cells -parietal cells |
The fundic gland is composed of mucus cells primarily in the neck region and then parietal cells in the upper region, chief cells predominantly in the lower half of glands, and enteroendocrine cells at base of the gland. p.174
|
|
|
The mucous neck cells in fundic glands produce what?
A. acidic mucous secretion B. gastric intrinsic factor C. gastrin D. pepsinogen E. serotonin |
mucous neck cells, located in the neck area of the gland, produce
A. acidic mucous secretion This appears basophilic with H&E stain (dark purple/blue color). p. 173 |
|
|
The parietal cells in fundic glands secrete what?
A. acidic mucous secretion B. gastric intrinsic factor C. gastrin D. pepsinogen E. serotonin |
B. gastric intrinsic factor
This appears acidophilic with H&E stain. p. 174 |
|
|
The chief cells in fundic glands secrete what?
A. acidic mucous secretion B. gastric intrinsic factor C. gastrin D. pepsinogen E. serotonin |
D. pepsinogen
This appears basophilic with H&E stain (dark purple/ blue color). p. 174 |
|
|
The enteroendocrine cells in fundic glands secrete what?
A. acidic mucous secretion B. gastric intrinsic factor C. gastrin D. pepsinogen E. serotonin |
sometimes C. gastrin & sometimes E. serotonin
This has variable staining with H&E. Note: Gastrin stiulates secretions of chief and parietal cells and increases gastric motility. Serotonin triggers contraction of smooth muscle of blood vessels which eventually leads to a slowing of gastric activity. p. 174 |
|
|
What gland do these come from and what are their respective effects?
A. acidic mucous secretion B. gastric intrinsic factor C. gastrin D. pepsinogen E. serotonin |
A. acidic mucous secretion = fundic gland; protective
B. gastric intrinsic factor = fundic gland's parietal cells; binds to vitB12 and allows it to be absorbed into small intestine C. gastrin = fundic gland's enteroendocrine cells; stimulates secretion of chief and parietal cells, increases gastric motility D. pepsinogen = fundic gland's chief cells; important enzyme in digestion of proteins E. serotonin = fundic gland's enteroendocrine cells; triggers contraction of smooth muscle of blood vessels, leads to slowing of gastric activity p. 174 |
|
|
What gastric gland releases gastric intrinsic factor and what does it do?
|
gastric intrinsic factor = fundic gland's parietal cells; binds to vitB12 and allows it to be absorbed into small intestine. Lack of this or B12 vitamin causes pernicious anemia. p. 174
|
|
|
Lack of what can cause pernicious anemia?
|
Lack of gastric intrinsic factor or B12 vitamin causes pernicious anemia. gastric intrinsic factor = fundic gland's parietal cells; binds to vitB12 and allows it to be absorbed into small intestine. p. 174
|
|
|
What gastric gland releases gastrin and serotonin?
|
Fundic gland's enteroendocrin cells
p. 174 |
|
|
What gastric gland releases pepsinogen?
|
pepsinogen = fundic gland's chief cells; important enzyme in digestion of proteins p. 174
|
|
|
Which cell in the fundic gland matches the description:
- have secretory canaliculus that increases surface area contain an abundance of mitchondria - secrete HCl - greater proportion of these cells is in upper part of glands |
parietal cells
p. 174 |
|
|
Which cell in the fundic gland matches the description:
- dominant cell type is in the lower half of glands have zymogen granules in their apical cytoplasm |
chief cells
these also secrete pepsinogen which is an important enzme in the digestion of proteins p. 174 |
|
|
Which cell in the fundic gland matches the description:
- a collection of at least 12 different cell types each of which secrete a specific endocrine hormone. - their secretions enter blood or affect adjacent cells |
enteroendocrine cells
these are found mostly in bases of glands p. 174 |
|
|
In the stomach, the muscularis externa has how many layers? How are they arranged?
|
THREE (usually has just two - inner circular and outer longitudinal). The third layer is added to the innermost area and is an oblique one.
Pyloric sphincter is formed by middle circular layer, Auerbach's plexus is between the circular and longitudinal layers still p. 174 |
|
|
The small intestine is approximately _____ feet long. How long are the duodenum, jejunum and ileum, repsectively?
|
~ 21 feet long total. Duodenum is 1 ft long, Jejunum 8 feet, Ileum 12 feet. p. 176
|
|
|
The small intestines have structural specializations that increase the surface area 500-fold.
Plica circulares increase the surface area ____ times. Intestinal Villi increase the surface area ____ times. Microvilli increase the surface area _____ times. |
Plica circulares = 2-3x
Intestinal villi = 10x Microvilli = 20x p. 176 |
|
|
[ plica circulares / intestinal villi / microvilli ] are permanent folds, involve mucosa and submucosa, and increase surface area 2-3 times.
|
Plica circulares
p. 176 |
|
|
[ plica circulares / intestinal villi / microvilli ] are finger-like projections 0.5-1.5 mm high, have a core of lamina propria and increase surface area 10 times.
|
Intestinal villi
p. 176 |
|
|
[ plica circulares / intestinal villi / microvilli ] are on absorptive cells and increase surface area 20 times.
|
Microvilli
p. 176 |
|
|
True or False:
Intestinal villi, permanent evaginations of the mucosa, are diagnostic for small intestines. |
True
They are covered with absorptive cells and goblet cells and have lacteals (blind-ended lymphatic channels in lamina propria core of villi. p. 176 |
|
|
True or False:
Lacteals are important in absorption of products of lipid digestion. |
True.
p. 176 |
|
|
Intestinal glands are composed of four cell types. Name em.
|
Goblet cells, absorptive cells, Paneth cells, enteroendocrine cells.
p. 176 |
|
|
In the small intestine, lymphatic nodules are scattered along the tract. Their nodular aggregates are known as:
A. crypts of Lieberkuhn B. Paneth patches C. Peyer's patches |
C. Peyer's patches
p. 176 |
|
|
Which cell type is the dominant one in the small intestines?
A. Enterocytes (Intestinal epithelial cells) B. Enteroendocrine cells C. Goblet cells D. Mucous neck cells E. Parietal cells |
A. Enterocytes (Intestinal epithelial cells) - these are ABSORPTIVE, tall columnar cells with a brush border p. 177
|
|
|
Enterocytes are intestinal epithelial cells, the dominant cell type in the small intestine. Which of the following is FALSE regarding it?
A. It is tall columnar cell with a brush border B. It has a well-developed glycocalyx which has enzymes that help convert pancreatic proenzymes inton active forms C. cells are bound together by junctional complexes D. responsible for the absorption of protein, carbohydrate and lipid digestions E. none are false |
E. none are false
p. 177 |
|
|
How are the following absorbed in the small intestine?
A. proteins B. carbohydrates C. Lipids |
A. proteins = as amino acids, via blood
B. carbs = as monosaccharides via blood C. as monoglycerides and fatty acids emulsified as bile, via lacteals p. 177 |
|
|
This cell type of the small intestine produces mucinogen which when released and mixed with water, creates mucus.
A. Enterocytes B. Goblet cells C. Paneth cells D. Enteroendocrine cells |
B. Goblet cells
p. 178 |
|
|
True or False:
The relative proportion of goblet cells decreases as you move distally along the GI tract. |
FALSE. Their proportion increases as you move along, though they never quite become THE dominant ones. p. 178
|
|
|
This small intestine cell type is found in bases of intestinal glands and contains large eosinophilic granules and secret lysozyme.
A. Enterocytes B. Goblet cells C. Paneth cells D. Enteroendocrine cells |
C. Paneth cells
p. 178 |
|
|
Enteroendocrine cells of the small intestine include a variety of cell types which are stimulated to release hormones in response to chyme entering the dudenum from the stomach. It also secretes _____ triggered by the acidity of chyme, whose function is to secrete bicarbonate made by centroacinar cells of the pancreas.
|
Secretin
p. 178 |
|
|
What cell of the small intestine secretes secretin and CCK?
|
Enteroendocrine cell
p. 178-9 |
|
|
True or False:
Secretin's release is triggered by fatty acids and L-amino acids in the duodenum. This hormone stimulates release of secretory granules by pancreatic acinar cells and stimulates contraction of the smooth muscle in the wall of the gall bladder. |
FALSE. This is actually describing CCK (cholecystokin)
p. 179 |
|
|
Plicae circulares are permanent ridges in the small intestine formed by what histological layers?
|
mucosa and submucosa
p. 179 |
|
|
True or False:
Plicae circulares are permanent ridges in the small intestine found only in the first 2/3. |
True
p. 179 |
|
|
The duodenum has submucosal glands called... what do they produce and secrete? What stimulates them to secrete?
|
Duodenal glands of Brunner, produce alkaline mucus (for protection), and are stimulated to secrete by acidic chyme entering duodenum p. 179
|
|
|
CCK (cholecystokinin) stimulates release of secretory granules by ________ and also stimulates contraction of the smooth muscle in the wall of the ________.
|
secretory granule release by pancreatic acinar cells ; contraction of smooth muscle in the wall of the gall bladder p. 179
|
|
|
True or False:
The large intestine does not have plicae or villi. |
True! Histologically, mucosa has a smooth surface and there are no plicae or villi.
p. 180 |
|
|
What is the function of the large intestine?
|
Dehydration of luminal contents (ie. water recovery) and vitamin absorption.
p. 180 |
|
|
True or False:
The large intestine's intestinal glands are classified as simply tubular glands. |
True.
p. 180 |
|
|
The appendix mucosa resembles the large intestine in the respect that it....
|
has no villi or plicae. In addition, like the small intestine and colon, it has simple tubular glands; prominent and numerous lymphoid nodulesas in both small intestine and colon. p. 181
|
|
|
True or False:
The rectum has simple tubular glands that are short and irregular, but otherwise the same as the large intestine. |
True
p. 181 |
|
|
The distal part of the rectum has 5-10 longitudinal columns called...
|
the anal columns of Morgagni. At the end of those colums is the pectinate line which marks the end of the rectum muscularis externae. There is no taeniae coli. p. 181
p. 181 |
|
|
The junction of the rectum and anal canal is called the ...
|
pectinate line
p. 181 |
|
|
True or False:
At the pectinate line, the muscularis mucosa disappears. |
True
p. 181 |
|
|
At the pectinate line, the hemorrhoidal venous plexus lies in which histological layer of the GI tract?
|
Mucosa's lamina priopria.
p. 181 |
|
|
At the pectinate line, the inner circular layer of muscularis externa [ forms the inner anal sphincter / forms the outer anal sphincter / disappears ] while the outer longitudinal layer [ forms the inner anal sphincter / forms the outer anal sphincter / disappears ].
|
Inner circular layer = internal anal sphincter ; outer longitudinal layer disappears. p. 181
|
|
|
Which organ of the GI tract does this describe: compound acinar gland lies retroperitoneal near duodenum, has slight regenerative capacity.
|
Pancreas p. 182
|
|
|
True or False: The anus is lined by keratinized stratified squamous epithelium.
|
True!
p. 182 |
|
|
The anus has an external anal sphincter formed by skeletal muscle and under control of what nerves?
|
spinal nerves!
p. 182 |
|
|
The pancreas is both and exocrine and endocrine gland. How so?
|
Exocrine component = compound acinar gland, secretion dependent upon hormones from the intestinal enteroendocrine cells (secretin and CCK) ; endocrine component = islet of Langerhands, hormonal secretions play role in carbohydrate metabolism p. 182
|
|
|
Iselts of Langerhans are scattered throughout the pancreas. Islets of Langerhans are made of three different cells. Name em and what they make.
|
Beta cells: most common in islet, make insulin. Alpha cells: next most common, make glucagon. Delta cels: makes somatostatin p. 183
|
|
|
True or False:
The exocrine pancreas is a purely serous gland. |
True! Made of acini as the main functional units. Secretory product of acinar cells include: trypsinogen, chymotrypsinogen, DNAse, RNAse, amylase, lipase. Release of enzymes dependent on CCK secreted by intestinal enteroendocrine cell. p. 183
|
|
|
This is the first part of the pancreatic duct system at the center of acini, granules are released into this space.
A. centroacinar cells B. excretory ducts C. intercalated ducts D. secretory canaliculi E. interlobular ducts |
D. secretory canaliculi
p. 184 |
|
|
This is the part of the pancreatic duct system that is still within the acini but involves the first non-acinar cell of the duct system. It lines the initial smallest part of intercalated ducts and can be squamous or cuboidal in shape.
A. centroacinar cells B. excretory ducts C. intercalated ducts D. secretory canaliculi E. interlobular ducts |
A. centroacinar cells
p. 184 |
|
|
This part of the pancreas duct system lies within pancreatic lobules and are lined by simple cuboidal and low columnar epithelium.
A. centroacinar cells B. excretory ducts C. intercalated ducts D. secretory canaliculi E. interlobular ducts |
C. intercalated ducts
p. 184 |
|
|
This part of the pancreatic duct lies in CT septa and has simple or stratified columnar epithlium.
A. centroacinar cells B. excretory ducts C. intercalated ducts D. secretory canaliculi E. interlobular ducts |
E. interlobular ducts
p. 184 |
|
|
This part of the pancreas duct system lies in the CT septa and has stratified columnar epithleium.
A. centroacinar cells B. excretory ducts C. intercalated ducts D. secretory canaliculi E. interlobular ducts F. none of the above |
F. none of the above.... it is excretory duct
p. 184 |
|
|
What are the two main ducts that empty into the duodenum?
|
Main pancreatic duct (of Wirsung) opens into duodenum at the papilla (ampulla of Vater) whose opening is controlled by a sphincter (of Oddi) ; accessory duct (of Santorini) p. 184
|
|
|
The liver receives a large volume of blood via two vessels. What are they?
|
Portal vein, Hepatic artery.
p. 185 |
|
|
Which portion of the GI tract is responsible for metabolizing products of digestion, storing glucose and detoxifying?
|
Liver
p. 185 |
|
|
True or False:
The liver, like the pancreas, functions as an exocrine and endocrine gland. |
True! The liver synthesizes bile (exocrine) and synthesizes plasma proteins (endocrine).
p. 185 |
|
|
Regarding liver lobulation, the basic lobule is a hexagon with ______ at the center and a ________ at each corner.
|
central vein in center; portal canal at each corner.
p. 185 |
|
|
Describe the blood flow through the liver lobule. (As in enters from... flows through.... to get to...)
|
Blood enters lobule from terminal branches of the portal vein and hepatic artery and flows through the sinusoids to the central vein. p. 185
|
|
|
Three definitions of loublation patterns exist to help explain the anatomy and function of the liver:
Classical hepatic lobule, Portal lobule, Liver acinus. Describe each. |
Classical hepatic lobule hexagon with portal canals at each corner, one central vein in middle. Based on blood flow. Portal lobule (corresponds to exocrine gland function) - a triangle with central vein at each corner and portal canal at center. Based on bile flow. Liver acinus - diamond shaped. Tissue supplied by terminal branch of portal vein and hepatic artery and drained by initial segment of bile duct system. Two central veins and two portal canals involved with two adjacent classical lobules. p. 185
|
|
|
Which liver lobulation pattern does this describe:
- Based on blood flow. - portal canals at each corner, one central vein in middle. |
Classical hepatic louble. p. 185
|
|
|
Which liver lobulation pattern does this describe:
- Based on bile flow. - triangle with central vein at each corner and portal canal at center |
Portal lobule p. 185
|
|
|
Which lobulation pattern does this describe:
- diamond shaped. - Tissue supplied by terminal branch of portal vein and hepatic artery and drained by initial segment of bile duct system. - Two central veins and two portal canals involved with two adjacent classical lobules. p. 185 |
Liver acinus
p. 186 |
|
|
Portal canal is formed of connective tissue plus blood vessels and ducts. The hepatic artery brings in [ 30% / 70% ] of the blood to liver and carries [ deoxygenated / oxygenated ] blood and brings products of [ carbohydrate and protein digestion absorbed by small intestine / fat digestion absorbed by small intestine to liver].
|
Hepatic artery = 30% , oxygenated blod, products of fat digestion absorbed by small intestine to liver.
p. 186 |
|
|
Portal canal is formed of connective tissue plus blood vessels and ducts. The portal vein brings in [ 30% / 70% ] of the blood to liver and carries [ deoxygenated / oxygenated ] blood and brings products of [ carbohydrate and protein digestion absorbed by small intestine / fat digestion absorbed by small intestine to liver].
|
portal vein = 70% , deoxygenated but carries products of carbohydrate and protein digestion absorbed by small intestine. p. 186
|
|
|
The bile duct is formed of what type of epithelium?
A. simple columnar B. simple cuboidal C. simple squamous |
B. simple cuboidal
p. 186 |
|
|
True or False:
Hepatocytes are six-sided cells with two free surfaces and four associated with other hepatocytes. |
True
p. 187 |
|
|
Regarding hepatocyte intercellular relationships, _____ is between the free surface of hepatocytes and sinusoidal lining cells. It contains blood plasma and microvilli of hepatocytes and is an area of exchange of metabolites.
A. bile cannaliculi B. cell junctions C. space of Disse |
C. space of Disse
p. 187 |
|
|
Regarding hepatocyte intercellular relationships, _____ is the dilated space between adjacent hepatocytes and form the first components of bile pathways.
A. bile cannaliculi B. cell junctions C. space of Disse |
A. bile cannaliculi
p. 187 |
|
|
Regarding hepatocyte intercellular relationships, _____ is how adjacent hepatocytes are joined together by a pair of zonule occludens junctions with bile canaliculi between.
A. bile cannaliculi B. cell junctions C. space of Disse |
B. cell junctions
p. 187 |
|
|
Almost half the cells in this part of the GI tract are binucleate or polyploid with one or more prominent nucleoli.
|
Liver
p. 188 |
|
|
True or False:
Hepatic sinusoids are a type of discontinuous capillary. |
True.
p. 189 |
|
|
Hepatic sinusoids have a zonation pattern with respect to oxygenation, nutrition and disease. Name the three zones and describe them.
|
Zone of permanent function- most metabolicaly active and least suceptible.
Zone of varying activity - variable metabolic activity. Zone of permanent repose - least metabolically active and most suceptible to damage. p. 189 |
|
|
______ are resident macrophages of the liver, lie on endothelium and are exposed to blood in lumen of sinusoids to filter out debris in plasma.
|
Kupffer cells
p. 189 |
|
|
______ drain sinusoids, they eventually come together to form two or more hepatic veins and later join with the IVC.
|
central veins
p. 189 |
|
|
Put the following components of the bile passageway in order:
A. Bile canaliculi B. Canals of Hering C. Hepatic duct D. Intrahepatic bile ducts |
A. --> D. (of which B. is a part of ) --> C.
Bile cannaliculi --> intrahpatic bile ducts (canals of Hering, ducts of portal canals) --> hepatic duct formed from fusion of large bile ducts from different hepatic lobules. Joins with cystic duct from gallbladder to form common bile duct. p. 189 |
|
|
The gall bladder's function is to...
|
store and concentrate bile. Bile emulsifies fat.
p. 190 |
|
|
True or False:
The epithelium of the pancreas is identified as "pseudodiverticulae". Due to the convoluted architecture, it resembles glands. |
FALSE. Pseudodiverticular belongs to the epithelium of the GALLBLADDER! p. 190
|
|
|
Under influence of what hormone from what cell does the gallbladder contract to send bile down?
|
CCK from enteroendocrine cells
p.190 |
|
|
Which part of the GI tract histologically has a diagnostic honeycomb look (deep invaginations)?
A. Colon B. Gallbladder C. Liver D. Pancreas E. Small Intestines |
B. Gallbladder
from Lecture III |

