![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
276 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What does the lymphatic system include? |
1. lymphatic vessels, tissues, and fluid 2. organs (nodes, tonsils, spleen, thymus, and the thoracic duct) |
|
|
|
What does lymph contain? |
1.excess interstitial fluid, 2. white blood cells, and 3. some proteins |
|
|
|
What tissues do not have lymphatic vessels? |
All do with the exception of the following: 1. superficial portions of the skin, 2. the CNS, and 3. bones |
|
|
|
What do lymphatic vessels accompany? What do they do? |
arteries and veins; drain lymph from bodily tissues and return it to the venous circulation |
|
|
|
What does the R lymphatic duct drain? Where does it drain into? |
The R arm, the R side of the head, and the R side of the thorax into the R subclavian vein. |
|
|
|
Where does the rest of lymph fluid in the body go (aside from that which R lymphatic duct drains)? |
into the thoracic duct which drains into the L subclavian vein. |
|
|
|
Name the major lymph nodes: |
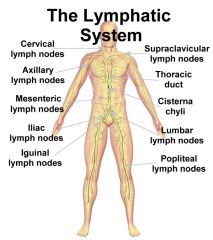
1. submaxillary, 2. cervical, 3. axillary, 4. mesenteric, 5. iliac, 5. inguinal, 6. popliteal, and 7. cubital |
|
|
|
What are the layers of the skin from superficial to deep?
|
1. Epidermis, 2. dermis, 3. subcutaneous tissue |
|
|
|
Which layer of the skin does not contain blood vessels? |
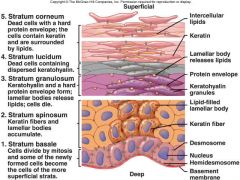
Epidermis |
|
|
|
Which layer of the skin is the outer, most superficial layer?
|
Epidermis |
|
|
|
Which layer of the skin is the in between layer? |
Dermis |
|
|
|
Which layer of the skin is composed of collagen and dense regular connective tissue you?
|
Dermis |
|
|
|
What does the dermis contain?
|
1. Blood vessels, 2. lymphatics, 3. nerve endings, 4. sebaceous and sweat glands |
|
|
|
Which layer of the skin contains blood vessels, lymphatics, nerve endings, sebaceous and sweat glands?
|
Dermis |
|
|
|
Which layer of the skin is deep to the dermis?
|
Subcutaneous tissue
|
|
|
|
What is the subcutaneous tissue also known as? |
Superficial fascia or subcutaneous fat
|
|
|
|
What does the subcutaneous tissue consist of?
|
Loose connective tissue and fat
|
|
|
|
What is the purpose of subcutaneous tissue?
|
Provides insulation, support, and cushion for skin and stores energy for skin |
|
|
|
What lies deep to the subcutaneous layer?
|
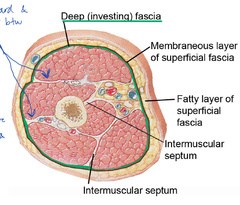
Deep investing fascia and muscles |
|
|
|
What does a system review of the integumentary system consist of?
|
Noting the following: -recent rashes, -nodules, or other skin changes; -unusual hair loss or breakage; -increased hair growth; -nail-bed changes and shape; -itching; -turgor |
|
|
|
What is hirsutism?
|

Increased hair growth |
|
|
|
What is clubbing?
|
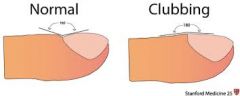
Changes in nailbed shape due to lack of oxygen to the periphery |
|
|
|
What is pruritus?
|

Itching |
|
|
|
What is turgor?
|
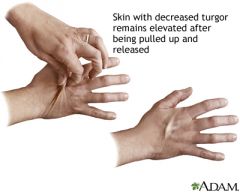
Is the test for hydration status performed by lifting the skin on the back of the hands |
|
|
|
What are the laboratory values for normal pre-albumin? |
20 – 40 mg/dL are
|
|
|
|
What would a poor pre-albumen lab value be and what with this indicate?
|
<15 mg/dL would indicate to malnutrition
|
|
|
|
What is the half-life of pre-albumin?
|
2 – day half-life |
|
|
|
What do pre-albumen lab values gauge?
|
short-term gauge of nutrition
|
|
|
|
What are the laboratory values for normal albumin?
|
3.5 to 5.5 g/dL |
|
|
|
What would a poor albumin lab value be and what with this indicate?
|
<3.5 g/dL; would indicate malnutrition |
|
|
|
What is the half-life of albumin?
|
18 to 20 day half life |
|
|
|
What do albumin lab values gauge?
|
Long term gauge of nutrition |
|
|
|
What are the lab values for normal glucose levels?
|
70 to 115 mg/dL (fasting)
|
|
|
|
What do glucose lab values indicate?
|
Short-term management of diabetes
|
|
|
|
What is another name for glycosylated hemoglobin? |
HbA1C |
|
|
|
What are the lab values for normal glycosylated hemoglobin? |
4 to 6% |
|
|
|
What do glycosylated hemoglobin lab values indicate? |
Long-term management of diabetes |
|
|
|
When performing and integumentary examination what exactly are you examining and recording (the nine things that you actually examine,test, measure, or observe)?
|
1. Characteristics 2. Color 3. Temperature 4. Texture 5. Edema 6. Vascular status 7. Sensation 8. Melanoma 9. Measurements |
|
|
|
Name some characteristics you would note during an integumentary examination: |
shiny, hair loss/hairless, pigmentation |
|
|
|
When describing skin color, what do the following words mean: Cyanosis, rubor, pallor, jaundice?
|
Blue, red, pale, yellow |
|
|
|
What are the two types of edema? |
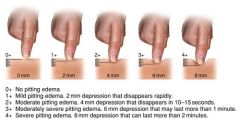
pitting and non-pitting |
|
|
|
When examining vascular status what test, measures, or exams might you do?
|
1. Posterior tibial and dorsal pedal pulses 2. Capillary refill 3. Rubor of dependency test 4. Ankle brachial index |
|
|
|
What is normal capillary refill?
|
<3 sec. |
|
|
|
What is the Rubor of dependency test?
|

Elevate LE for 1 min., soul of the foot goes pale, lower LE to neutral, if there's adequate arterial circulation but sole of the foot should exhibit rubor in <15 seconds |
|
|
|
How do you calculate ankle brachial index? |

Tibial systolic blood pressure divided by brachial systolic blood pressure |
|
|
|
What is considered a normal ABI? |

1.0 |
|
|
|
Name the various ways to test sensation: |
1. dermatome testing 2. Semmes-Weinstein monofilament testing 3. Vibratory Sense testing |
|
|
|
How would you test for light touch? |
Dermatome Testing |
|
|
|
How would you test for discriminatory touch/protective sensation? |
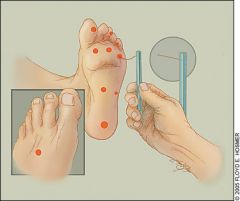
Semmes-Weinstein monofilament testing |
|
|
|
What is the norm for protective sensation? |
5.07 (10g) |
|
|
|
What the ABCDEs of a Melanoma examination? |

1. Asymmetry 2. Boarders (irregular) 3. Color (various shades in one mole) 4. Diameter 5. Evolving |
|
|
|
Wound measurements and documentation should include what? |
LETS: Location Exudate Characteristics Tissue Characteristics Size and Shape |
|
|
|
Wound description of size and shape should include what? |
length, width, depth, tunneling, and undermining |
|
|
|
Wound description of tissue characteristics should include what? |
percent of viable vs non-viable tissue |
|
|
|
Describe and state what may be indicated if exudate is sanguineous? |
red; signifies bloody discharge |
|
|
|
Describe and state what may be indicated if exudate is serous? |
clear; signifies watery discharge |
|
|
|
Describe and state what may be indicated if exudate is purulent? |
yellow, tan, or green; signifies potential infection |
|
|
|
Name three wound care interventions
|
debridement, dressing, modalities
|
|
|
|
What is debridement?
|
A process in which necrotic tissue is removed to aid the healing process
|
|
|
|
What is selective debridement? In other words what are methods of selective debridement?
|
Debridement may be done by scalpel, scissors, enzymes, surgery, or autolytic dressings |
|
|
|
What is nonselective debridement? In other words what are methods of nonselective debridement?
|
Nonselective debridement may include the use of hydrotherapy and various dressings (went to went, but to dry, and dry to dry) in which necrotic tissue clings to the dressing when removed from the wound
|
|
|
|
What affect do antimicrobial agents have on wound healing and when should they be used?
|
They may retard healing and should not be used routinely in whirlpool or is topical agents on the wound unless the antimicrobial action is absolutely desirable |
|
|
|
Name some antimicrobial agents
|
Povidone-iodine, bleach, Dakin's solution
|
|
|
|
What role do dressings play in the wound care? |
1. Protect the wound contamination and trauma, 2. Permit application of medication, 3. Absorb drainage, 4. Debride necrotic tissue, and 5. Enhance healing |
|
|
|
Dressing choices for a wound are based on what three primary characteristics of the wound? |
1. Color, 2. Depth, and 3. Exudate production |
|
|
|
Name the various dressings typically used by physical therapist
|
HHOG FFANS: hydrocolloid, hydrogels, occlusive dressings, gauze, films, foam, alginates, non-adherents, and semi-rigids |
|
|
|
When is gauze useful for wound care? |

During early debridement, exudate present, wound with dead spaces or tunneling, necrotic tissue with exudate |
|
|
|
When would wet to dry gauze be useful for wound care?
|

With mechanical debridement of necrotic tissue and slough |
|
|
|
When would continuous dry gauze be useful for wound care?
|

With heavily exudating wounds |
|
|
|
When would continuous moist gauze be useful for wound care? |

for protection of clean wounds, autolytic debridement of eschar, or delivery of topical needs |
|
|
|
What are the advantages of gauze for wound care? |
1. Readily available 2. Can be used with saline, gels, or topical anti-microbials 3. Can be used on infected wounds 4. it's a good mechanical debridement 5. Is a cost-effective filler for larger wounds |
|
|
|
What are the disadvantages of gauze for wound care?
|
1. Frequent dressing changes can disrupt newly formed granulation tissue 2. Pain on removal (Wet to dry) 3. labor-intensive 4. May require secondary dressing 5. Delayed healing if used improperly |
|
|
|
What is a contraindication of using gauze for wound care?
|

Over granulation tissue out some type of intermediate nonadherent dressing |
|
|
|
When would and occlusive dressing be useful for wound care?
|

1. To maintain tissue hydration 2. To facilitate autolytic debridement 3. For wound healing with less pain |
|
|
|
What are contraindications to using occlusive dressing for wound care?
|
1. Infected wound 2. Ischemic ulcers 3. Full thickness burns 4. Very heavy exudate 5. Over stage IV ulcers |
|
|
|
What are alginates and what do they do?
|
They are derived from seaweed and react with exudate to form gel over the wound |
|
|
|
When would alginate dressing be useful for wound care?
|
With wounds containing moderate to large amounts of exudate or with combination exudate and the necrosis |
|
|
|
Wounds that require packing and absorption would benefit best from what type of wound dressing? |
Alginates |
|
|
|
What are the advantages of alginates for wound care?
|
1. Easy to apply 2. Supports debridement in presence of exudate 3. Fills dead space 4. Can be used over infected wound |
|
|
|
What are the disadvantages of alginate for wound care?
|
1. Need a secondary gauze or film dressing on top 2. Not recommended for dry or lightly exiting wound. 3 they can dry the wound to bed |
|
|
|
What are films? What that are used for in wound care? What are the permeable to? What are they in permeable to?
|
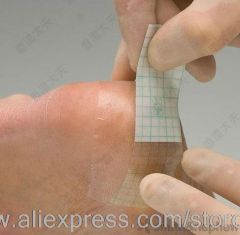
Clear adhesive membrane; used to maintain moist wound environment with minimum to moderate text you date often in stage 1 and stage 2 pressure ulcer's; permeable to atmospheric oxygen and moisture vapor; Impermeable to water, bacteria, and contaminants. |
|
|
|
What would be the best and most common dressing used for stage 1 and stage 2 pressure ulcer's? |
Films
|
|
|
|
What are the advantages of films for wound care?
|
1. Minimize friction 2. Transparent and comfortable 3. Excellent bacterial barrier 4. Promote faster healing and autolytic debridement 5. Visual of evaluation of wound without removal |
|
|
|
What are the films for wound care? |
1. Non-absorptive 2. Application can be difficult 3. Not to be used on wounds with fragile surrounding skin or infected wounds |
|
|
|
When would foam dressings be useful for wound care?
|

To cushion and protect the wound |
|
|
|
What are foam dressings hydrophilic and hydrophobic towards?
|
These dressings are hydrophilic (absorb moisture) on the wound side, and hydrophobic on the non-wound side |
|
|
|
What are the advantages of foams for wound care?
|
1. Insulate wounds 2. Provide padding 3. large amounts of exudate 4. Comfortable 5. Easy to use |
|
|
|
What are the disadvantages of foam for wound care? |
1. Require secondary dressing 2. not for use with dry eschar or wounds with no exudate 3. Nontransparent |
|
|
|
What are hydrocolloid dressing? When would hydrocolloid dressing be useful for wound care?
|

adhesive wafers that interact with wound to form gelatinous mass; These may be occlusive or semi-occlusive, absorbs minimal to moderate exudate, protects partial thickness wounds |
|
|
|
What wound dressing should be used to protect partial thickness wound?
|
Hydrocolloid dressing
|
|
|
|
What are the advantages of hydrocolloid dressing?
|
1. Maintaines a moist wound environment 2. Excellent bacterial barrier 3. Nonadhesive to healing tissue 4. Comfortable 5. Supports autolytic debridement 6. Reduces pain 7. Easy to apply 8. Time-saving 9. Diminishes friction |
|
|
|
What are the disadvantages of hydrocolloid dressing? |
1. Not used over infected wounds 2. Nontransparent 3. May soften or change shape with heat or friction 4. Not for wound with heavy exudate or with fragile surrounding tissue 5. Dressing edges may curl |
|
|
|
What are hydrogel's and what type of wounds are these used with? |

Water or glycerin based; used with partial or full thickness wounds with necrosis ( ie. tissue damage from burns or radiation); Absorb minimal amounts of exudate, letting some exudate passed through to a secondary dressing |
|
|
|
What are the advantages of hydrogel dressing?
|
1. Conforms to the wound 2. Rehydrates and maintains a moist wound environment 3. Promotes autolytic debridement 4. Soothing and cooling 5. Transparent 6. Nonadherent 7. Amorphis form can be used when infection is present |
|
|
|
What are the disadvantages of hydrogel dressing?
|
1. Not used with high exudate production 2. most require secondary dressing 3. may macerate surrounding skin |
|
|
|
What is a non-adherent wound dressing? When would a non-adherent dressing be useful for wound care? |

Gauze like dressings that do not adhere to the wound; they're often petroleum based (Adaptic or Tegaderm) and impregnated with some type of solution to promote granulation (scarlet red) or inhibit bacterial formation (Xeroform); they require a secondary dressing and are non-absorptive |
|
|
|
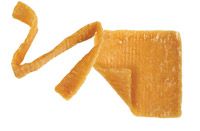
What are semi rigid dressings? When are semirigid dressings useful and wound care? |

Unna boot is a pliable, non-stretchable dressing impregnated with appointments (zinc oxide, calamine, and gelatin); used for venous insufficiency ulcers to control for edema and help with healing |
|
|
|
What treatment modalities promote wound healing? |
1. Iontophoresis 2. Ultrasound 3. Electrical stimulation 4. Vacuum assisted closure (VAC) |
|
|
|
When using iontophoresis to promote wound healing, what two substances can be utilized? |
zinc or histamine |
|
|
|
What is the polarity of the zinc? What is the polarity of histamine?
|
Positive; positive
|
|
|
|
What role does ultrasound play in wound healing? |
To speed up wound healing
|
|
|
|
What are the parameters for using ultrasound and healing? |
Frequency: 3X/week, intensity: low intensity, Type: pulsed ultrasound
|
|
|
|
Why is electrical stimulation used in wound care/what does it do
|
Electrical stimulation can be used to increase wound healing or reduce bacterial contaminants |
|
|
|
What parameters of electrical stimulation are applied to wound healing?
|
Hi voltage pulsed current (HVPC) is most commonly used; low-voltage continuous direct-current has also been proven beneficial
|
|
|
|
What are the pros and cons of using different voltage and current with regard to E-stim and wound care?
|
High-voltage post current has relatively no side effects where as low voltage continuous direct-current has the potential (similar to iontophoresis) to harm the client
|
|
|
|
What is an anode and what is it used to promote?
|
a positive pole; used to promote epithelial cell migration and for reactivation of the inflammatory phase |
|
|
|
What is a cathode and what is it used to promote? |
a negative pole; used to promote granulation, control information, and inhibit certain bacteria
|
|
|
|
What is the vacuum assisted closure (VAC)? When is VAC indicated? |
This is a negative pressure system used for any type of wound (including arterial); Indicated when a wound is not closing, when there is a lack of arterial perfusion, or when there is excessive exudate that cannot be controlled with dressing |
|
|
|
How is a vacuum assisted closure applied? Can it be used in the presence of infection? |
It is applied continuously and can be used in the presence of infection |
|
|
|
What are the sequence of events for dermal wound healing (What are the stages)? |
1. Inflammatory phase 2. Granulation formation/proliferation or fibroblastic phase 3. Maturation, repair, and matrix formation |
|
|
|
What is the timeframe of the inflammatory phase? |
Begins at the time of injury and ends in 3 to 5 days
|
|
|
|
What is the inflammatory phase characterized by? |
Redness, edema, warmth, pain, and decreased range of motion |
|
|
|
What cells are common during the inflammatory phase? |
Neutrophils and macrophages |
|
|
|
What is the timeframe of the granulation formation/proliferation or fibroblastic phase?
|
Begins 2 to 3 days after the injury and continues for several weeks |
|
|
|
What is the granulation formation/proliferation or fibroblastic phase characterized by?
|
Granulation buds and epithelialization; wound contraction, granulation tissue filling the defect, and epithelial cells migrating from the wound margins |
|
|
|
What cells are common during the granulation/proliferation phase of healing?
|
Fibroblasts, myofibroblasts, and epithelial cells |
|
|
|
What do fibroblasts do? What is critical during the granulation/proliferation phase of healing?
|
Fibroblasts synthesize collagen, CAGs (glycosaminoglycan's),and elastin; collagen synthesis is critical for the integrity of the wound |
|
|
|
What occurs during re-epithelialization?
|
Re-epithelialization occurs as cells migrate from the wound margin to provide a protective barrier preventing fluid and electrolyte loss and producing the chances of infection
|
|
|
|
What is the timeframe of the maturation, repair and matrix formation phase? |
Begins within 2 to 4 weeks of injury and continues even after the wound is healed |
|
|
|
What is the maturation, repair, and matrix formation phase characterized by?
|
Weaker collagen is replaced with a stronger collagen
|
|
|
|
How is the alignment of collagen determined?
|
the alignment of the collagen is dependent on the forces imposed
|
|
|
|
When can healing be considered complete?
|
When the epithelium covers the surface
|
|
|
|
Remodeling of the scar tissue can last how long? |
Up to 2 years
|
|
|
|
What are the time frames of normal scar formation? |
1. 6 to 12 weeks: bright pink scar, immature wound 2. 12 to 15 months: changes to a soft lavender and finally faint pink scar 3. Mature scar will be soft white and flat |
|
|
|
What may cause delays in wound healing?
|
Intrinsic factors, exit contact factors, and chronic inflammation
|
|
|
|
What are some intrinsic factors that would delay wound healing? |
1. Aging 2. Chronic diseases 3. Circulatory diseases 4. Malnutrition 5. Neuropathy |
|
|
|
What are some extrinsic factors that would delay wound healing? |
1. Medications (steroids) 2. Necrotic tissue 3. Infection 4. Excessive pressure 5. Wrong dressing choice |
|
|
|
How can chronic inflammation affect wound healing? |
You can persist for months or years into labor and healing due to the chronic tissue, colonization, infection, or foreign materials present with in the wound. |
|
|
|
How is chronic inflammation usually recognized?
|
By a wound not healing normally and or a Halo of redness (for lighter pigmented individuals) or purple hue (darker pigmented individuals) from an extensive release of histamine |
|
|
|
With chronic inflammation why is there an excess release of histamine? |
This maybe due to over react of macrophages and mast cells |
|
|
|
Can inflammation and healing occurs simultaneously?
|
No, the source of information must be resolved before healing can begin
|
|
|
|
What are the various types of wound union?
|
Primary, secondary, and tertiary |
|
|
|
What is primary union? |
The healing that takes place following a noninfected laceration or surgical incision; No major loss of connective tissue you
|
|
|
|
How does primary union occur?
|
Sealing by blood clot
|
|
|
|
With primary union, what occurs with in hours? Days? Weeks? Months?
|
Hours: blood clot formation Days: 1–3 days epithelialization and fibroblast proliferation weeks: over a period of weeks subsequent formation of collagen tissue occurs months: the college and eventuallyloses its excess vascular supply and the tissue strength increases by the end of 2 months
|
|
|
|
What is secondary union?
|
The prolonged process of dermal healing the results from necrosis of tissue due to inflammation or dramatic distraction (to cubitus ulcer healing)
|
|
|
|
How does secondary union occur?
|
There's a delay of wound healing unless dead tissue and debris are removed from the wound |
|
|
|
What is indicative of healthy secondary union healing?
|
A beefy red appearance indicates healthy healing of the wound and no debridement or chemical antibacterial agent is indicated
|
|
|
|
Moist wound healing should be promoted with the exception of when?
|
Except in the presence of infection
|
|
|
|
What is tertiary union?
|
This is delayed primary union; a delay in the suturing of the site for 5 to 7 days
|
|
|
|
When is tertiary union indicated?
|
In the presence of wound contamination (risk of infection), large tissue loss, or excessive edema
|
|
|
|
What is the healing sequence in tertiary union?
|
Similar to an injury treated with a primary union except for a delay of about a week
|
|
|
|
What occurs with bone healing with regard to sequence of events?
|
Occurs within a few days that the Boone is not infected; the process involves considerable hemorrhage, followed by proliferation of osteoblasts, then to the formation of a callous at about a week, which eventually remodels into bone |
|
|
|
What is the ideology of pressure ulcers (bedsores, decubitus or trophic ulcers)?
|
Primarily the result of prolonged pressure, necrosis of tissues most often occurs over a bony areas |
|
|
|
Where do pressure ulcers typically occur?
|
The most common areas affected include the heels, plantar surface of the foot, malleoli, trochanters, ischial tuberosity, sacrum, and scapula
|
|
|
|
What is the primary risk factor associated with pressure ulcers?
|
Immobility
|
|
|
|
Other risk factors for pressure ulcers include what?
|
Decreased sensation, moisture, friction or sheering forces, decreased arterial perfusion, and and abnormally low or high BMI |
|
|
|
To prevent pressure ulcers, how often must pressure sensitive areas be relieved in a recombinant position? In a sitting position?
|
3 to 4 times per hour, every 15 to 20 minutes
|
|
|
|
What can be done to the skin to prevent pressure ulcers?
|
The skin should be inspected and kept clean and dry
|
|
|
|
What are pressure ulcer risk assessment scales?
|
Braden and/or Norton
|
|
|
|
How many stages are represented in pressure ulcer staging?
|
4
|
|
|
|
Describe stage I of a pressure ulcer including: the skin, intervention, and if applicable other indicators
|
non-blanching erythema; this stage is reversible with intervention; other indicators include discoloration, warmth, edema, and induration (firming or hardening of tissue secondary to edema) |
|
|
|
Describe stage II of a pressure ulcer including: the skin, intervention, and if applicable other indicators
|
partial thickness skin loss; epidermis and dermis are involved; presents as an abrasion, blister, or shallow crater
|
|
|
|
Describe stage III of a pressure ulcer including: the skin, intervention, and if applicable other indicators
|
Full thickness skin defect extending into the fat layer (subcutaneous tissue), but not through the fascia |
|
|
|
Describe stage IV of a pressure ulcer including: the skin, intervention, and if applicable other indicators
|
Full thickness skin defect that extends beyond the fascia into the muscle; other structures are often exposed (tendon, capsule); the ultimate extend down to and include bone destruction |
|
|
|
There's another term used for staging that does not include stages one through four, what is this term and when is this term used?
|
Unstageable; The term is used if the wound is obscured by necrotic tissue
|
|
|
|
What are the treatments involved in stage I pressure ulcer care?
|
vigorous pressure, friction, and moisture alleviating measures are required
|
|
|
|
What are the treatments involved in stage II pressure ulcer care?
|
dermis is exposed; if there is no infection, and appropriate dressing that includes the wound from the environment is required; similar pressure, friction, and moisture alleviating measures from stage ulceration are required |
|
|
|
What are the treatments involved in stage III pressure ulcer care?
|
subcutaneous tissue is exposed; this stage often requires debridement (necrotic tissue), dressings, and advanced pressure alleviating measures |
|
|
|
What are the treatments involved in stage IV pressure ulcer care?
|
extends beyond the fashion; debridement, appropriate dressing choice, and advanced pressure alleviating measures are required; surgery and grafting maybe more likely at this stage |
|
|
|
If a pressure Alster wound is infected and no healing has occurred, at what point me a new interventions may be introduced? What is that modality?
|
2 weeks, then antibacterial agents or a treatment modality maybe indicated
|
|
|
|
What is the etiology of arterial insufficiency ulcers?
|
Causes include arteriosclerosis obliterans
|
|
|
|
In what population do we tend to see arterial insufficiency ulcers?
|
Patients with diabetes
|
|
|
|
How do you arterial insufficiency ulcers typically present?
|
deep and painful with skin pale and cold
|
|
|
|
Where are arterial insufficiency ulcers typically located?
|
On the lateral malleolus and toes
|
|
|
|
Name optional treatment for arterial insufficiency ulcers
|
bed rest, see station of smoking, wound care, range of motion, and protective environment (these are conservative ways of managing these wounds)
|
|
|
|
If bedrest is a treatment selected for arterial insufficiency ulcers, how should the bed be set up?
|
With the head of the bed elevated moderately
|
|
|
|
What type of modality maybe used to treat an arterial insufficiency ulcer?
|
A wound VAC maybe useful
|
|
|
|
If an ABI is at what level, the wound will not heal without medical intervention such as surgery or medications? |
An ABI of 0.5 or below
|
|
|
|
What is the etiology of Venus insufficiency ulcers? |
venous thrombosis, varicose veins, and other venous problems |
|
|
|
Describe the characteristics of Venus insufficiency ulcers
|
painless and superficial with good peripheral pulses
|
|
|
|
Is edema present with Venus insufficiency ulcers?
|
Yes
|
|
|
|
What does the skin look like in a patient with Venus insufficiency ulcers?
|
Pigmented
|
|
|
|
What is hemosiderinosis?
|
Pigmented skin
|
|
|
|
Where are Venus insufficiency ulcers typically located?
|
On the medial side of the ankle
|
|
|
|
What type of treatment (to control edema) is typically used for Venus insufficiency ulcers?
|
Elevation and compression to control edema is vital
|
|
|
|
What are some ways to elevate and compress a venous insufficiency ulcer?
|
Unna boot, custom fitted elastic stockings, and intermittent compression therapy
|
|
|
|
Would whirlpool treatment be helpful in a patient with Venus insufficiency ulcers? Why or why not?
|
Whirlpool is not helpful to you too dependent position
|
|
|
|
What type of exercises, positions, and garments should be used with a patient having a Venus insufficiency ulcer?
|
Active exercise, elevation of the body part, support garments
|
|
|
|
What is necessary for long-term management of Venus insufficiency ulcers?
|
Compression stockings
|
|
|
|
What is the etiology of diabetic foot ulcers?
|
peripheral vascular disease and neuropathy
|
|
|
|
What are characteristics of a patient with the diabetic foot ulcer?
|
Decreased perspiration, dry cracked skin, decreased sensation and circulation, and Charcot foot
|
|
|
|
What type of neuropathy is a diabetic foot ulcer?
|
Autonomic Neuropathy
|
|
|
|
How is staging of diabetic foot ulcers performed?
|
According to the Wagner scale
|
|
|
|
Why is use of pressure ulcer scale not used to measure or stage a diabetic foot ulcer?
|
it is considered inappropriate
|
|
|
|
Treatment of a diabetic foot ulcer includes what?
|
Debridement of necrotic tissue and promote moist wound healing, offload the ulcer from abnormal pressures, modify the shoe to use of a rocker bottom soul
|
|
|
|
How do you offload a diabetic foot ulcer from abnormal pressures?
|
Total contact cast and/or change in weight bearing status with the use of assistive device What type of exercises, positions, and garments should be used
|
|
|
|
What are contraindications for total contact cast?
|
Infection or ulcer depth greater than width
|
|
|
|
How is the amount of skin destruction beast with regard to burns?
|
It is based on the temperature to which the skin is exposed and the length of time the tissue is exposed to the heat
|
|
|
|
What are the types of insults that result in burns?
|
Flame, liquid, chemical, electrical
|
|
|
|
What determines the extent of tissue damage in a burn?
|
The type of insult
|
|
|
|
The burn wound consists of what three zones?
|
Zone of coagulation, zone of stasis, zone of hyperemia
|
|
|
|
What is the zone of coagulation?
|
Cells are irreversibly damaged and skin death occurs
|
|
|
|
What is the zone of stasis?
|
Contains injured cells that may die within 24 to 48 hours without specialized treatment
|
|
|
|
What is the zone of hyperemia?
|
Site of minimal cell damage and the tissue should recover within seven days with no lasting ill effects
|
|
|
|
How are burn injuries classified?
|
By severity; the layers of skin damaged
|
|
|
|
What does the amount of skin damage depend upon?
|
Duration and intensity of heat, skin thickness and area exposed, vascularity, age, and persons pigmentation
|
|
|
|
What degree is a superficial burn?
|
First degree
|
|
|
|
What is damaged in a superficial burn?
|
Only the epidermis
|
|
|
|
What is an example of a superficial burn?
|
Sunburn
|
|
|
|
What is a superficial burn characterized by?
|
Erythema, slight edema, tenderness, and no blistering
|
|
|
|
What integumentary changes occur with a superficial burn?
|
Some peeling of skin will occur spontaneous
|
|
|
|
What is the healing time frame for a superficial burn?
|
healing in 2 to 5 days
|
|
|
|
What degree is superficial partial thickness burn?
|
Second degree
|
|
|
|
What is damaged in a superficial partial thickness burn?
|
this has damage to the upper layers of the dermis as well as the epidermis
|
|
|
|
What is a superficial partial thickness burn characterized by?
|
Blisters, inflammation, and severe pain occur
|
|
|
|
What integumentary changes occur with a superficial partial thickness burn?
|
minimal scarring with some residual skin color changes
|
|
|
|
What is the healing time frame for a superficial partial thickness burn?
|
healing should be complete without surgical intervention within 7 to 10 days
|
|
|
|
What degree is a deep partial thickness to burn?
|
Second degree
|
|
|
|
What is damaged in a deep partial thickness burn?
|
Most of the dermis is destroyed with injury to the hair follicles, nerve endings, and sweat glands
|
|
|
|
What is a deep partial thickness burn characterized by?
|
Red or white appearance, Adema, blistering, and severe pain
|
|
|
|
What is damaged in a deep partial thickness burn?
|
Not all of the nerve endings are destroyed, so pain is experienced
|
|
|
|
What integumentary changes occur with a deep partial thickness burn?
|
hypertrophic and keloid to scarring are common
|
|
|
|
What is the healing time frame for a deep partial thickness burn?
|
3 to 5 weeks
|
|
|
|
What degree is a full thickness burn?
|
Third degree
|
|
|
|
What is damaged in a full thickness burn?
|
Complete destruction of the epidermis, dermis, and subcutaneous tissues with some muscle damage
|
|
|
|
What is a full thickness burn characterized by?
|
White, gray, or black tissue with a try surface, edema, a scar formation, and insensate or little pain (Nerve endings are destroyed)
|
|
|
|
What is damaged during a full burn?
|
Nerve endings are destroyed so there is no pain or little pain in the immediate area, but there's often significant pain in the surrounding tissue
|
|
|
|
What is the healing time frame for a full thickness burn?
|
Surgical removal of S car and skin grafting are necessary for healing to occur and no time is given for healing time in the review book
|
|
|
|
What is an escharotomy?
|
Surgical removal of eschar
|
|
|
|
What's integumentary changes occur with a full thickness burn?
|
Infection and hypertrophic scarring, and keloid scarring
|
|
|
|
What is a hypertrophic scar?
|
a raised scar that stays within the boundaries of the burn wound, often occurs with a full thickness burn
|
|
|
|
What is a sub dermal burn characterized by?
|
The skin is chard, dry and appearance, or mummified
|
|
|
|
What is damaged in a subdermal burn?
|
Destruction of the vascular system which may also lead to additional process
|
|
|
|
How does a subdermal burn typically occur?
|
From prolonged contact with the flame or hot liquid or from an electrical burn
|
|
|
|
What is a common outcome of a subdermal burn?
|
Imputation and muscle paralysis are common
|
|
|
|
What is the healing time frame for a subdermal burn?
|
Usually the patient will need extensive surgery and rehabilitation; a timeframe is not provided in the review book
|
|
|
|
How is the extent of a burned area determined?
|
By the percentage of the body's total surface area that has been burned and the depth of the burned areas
|
|
|
|
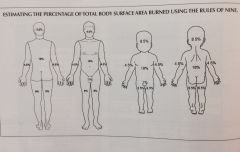
What is the rule to determine the extent of a burned area?
|
The rule of nines is a quick technique to estimate the total burn surface area of adults
|
|
|
|
How is the rule of nines determined?
|
The surface area of the body is divided into segments that are approximately 9% of the total children and infants are slightly different due to the size of their head and respect their body classification system often used to determine the extent of the burned area?
|
The Lund Browder classification
|
|
|
What is the leading cause of death in patients with Burns?
|
Infection
|
|
|
|
What makes a burn wound very susceptible to infection?
|
The distraction of defense mechanism against bacteria
|
|
|
|
What are pulmonary complications a burn injuries?
|
smoke inhalation, pneumonia, restrictive lung disease
|
|
|
|
What is the incidence of smoke inhalation?
|
Maybe in excess of 33%
|
|
|
|
What is the incidence of death due to pneumonia with burn injuries?
|
Pneumonia may account for over one third of deaths of burn patients
|
|
|
|
When they restrictive lung disease occur in patients with Burns?
|
Inpatient to have moderate sized burns over the trunk regions
|
|
|
|
What are metabolic complications of burn injuries?
|
There's an overall increase in metabolic and catabolic activity
|
|
|
|
What are the consequences of an increase in metabolic and catabolic activity in a patient with Burns?
|
Rapid decrease in body weight, negative nitrogen balance, and decreased energy stores
|
|
|
|
What are cardiac and circulatory complications of burn injuries?
|
loss of the plasma and intravascular fluid
|
|
|
|
In a patient with a complicated burn injury there maybe loss of plasma and intravascular fluid. Immediately following the burn what occurs initially? What occurs after these initial changes?
|
The fluid loss will initially decreased cardiac in output, which then gradually increases to normal or above normal levels
|
|
|
|
How does the epidermis heal?
|
by the epithelialization Of viable cells that grow, proliferate, and migrate to cover the wound
|
|
|
|
What should the therapist be concerned about with epidermal healing?
|
Protecting and moisturizing the epithelial cells to promote wound healing
|
|
|
|
How does the dermis heal?
|
Healing result in scar formation, following growth, proliferation, and migration to cover the wound
|
|
|
|
How does hypertrophic or keloid scarring result?
|
If the production rate of collagen exceeds the breakdown
|
|
|
|
What are the treatment options for burn injuries?
|
Debridement, topical medications, dressings, surgery, skin grafting, compression therapy, physical therapy, sprinting and positioning
|
|
|
|
When is debridement indicated for use with burn injuries?
|
To remove the dead tissue, prevent infection, and promote revascularization and or re-epithelialization of the burn area
|
|
|
|
When is the use of topical medications indicated with burn injuries?
|
With infection
|
|
|
|
Name the antibacterial agents used with burn injuries
|
nitrofurazone or Furacin, silver sulfadiazine or Silvadene, mafenide acetate or Sulfamylon, bacitracin, and Neosporin
|
|
|
|
When are dressings indicated for use with burn injuries?
|
Secondary dressings are required over the topical agent
|
|
|
|
Why are secondary dressings required over a topical agent in burn injuries?
|
Prevent bacterial contamination, prevent fluid loss, and protects the wound
|
|
|
|
What is the primary reason for surgery with regard to burn injuries?
|
Surgical removal of the eschar
|
|
|
|
During what time frame is surgery following a burn most beneficial? Why?
|
Early excision is easier on the patient, promotes more rapid healing, reduces infection and scarring, and is more economical than repeated debridement
|
|
|
|
When is skin grafting indicated with burn injuries?
|
To close a burn wound at the time of primary excision
|
|
|
|
What is an autographed?
|
A skin graft made from the patients in the skin
|
|
|
|
What is an allograft or homograft?
|
Skin taken from an individual of the same species, usually cadaver skin
|
|
|
|
What does the patient receive an aloe graft is used?
|
That me know suppressive drug for)
|
|
|
|
What is the Xenograft or hetero graft?
|
Skin of another species
|
|
|
|
What is Xenograft typically made of?
|
Skin of a pig
|
|
|
|
What does a split thickness graft contain?
|
Epidermis and upper layers of dermis from a donor site
|
|
|
|
What does a full thickness graft contain?
|
Epidermis and dermis from the donor site
|
|
|
|
What is compression therapy and when is it used?
|
following grafting, the injured part is rested and pressure dressings are applied to reduce craft separation
|
|
|
|
Why are pressure garments used with burn injuries?
|
They're used to help prevent or minimize hypertrophic or keloid scarring
|
|
|
|
When is physical therapy indicated for burn injury and what does it consist of?
|
Prevention of scar contracture, maintenance of normal range of motion, maintenance or improvement in muscular strength and cardiovascular endurance, return to normal function and performance of ADLs
|
|
|
|
Physical therapy intervention for patient with Burns include exercises designed to do what?
|
Promote deep breathing and chest expansion, with ambulation used to prevent pneumonia
|
|
|
|
When is splinting and positioning indicated for patients with Burns?
|
When needed to prevent or correct deformities or contractures
|
|
|
|
When should splinting and Positioning begin in patients with burn injuries?
|
On the day of admission
|
|
|
|
What is the best method to reduce joint contractures?
|
Implementing a program of active range of motion every two hours within 24 hours of hospital admission
|
|
|
|
What is the second best option for reducing contractures?
|
Passive range of motion
|
|
|
|
What type of contracture (deformity) typically occurs at the anterior neck? What position should be used for prevention or correction?
|
Flexion; hyper extension with a firm cervical breaks
|
|
|
|
What type of contracture (deformity) typically occurs at the shoulder? What position should be used for prevention or correction?
|
adduction and IR; Abduction and ER using an airplane splint
|
|
|
|
What type of contracture (deformity) typically occurs at the elbow? What position should be used for prevention or correction?
|
flexion and pronation; extension and supination splint
|
|
|
|
What type of contracture (deformity) typically occurs at the hand? What position should be used for prevention or correction?
|
Clawhand, flexion and adduction; for clawhand: Wrist extension, MCP flexion, IP extension brace, for flexion and adduction: extension and abduction brace
|
|
|
|
What type of contracture (deformity) typically occurs at the knee? What position should be used for prevention or correction?
|
Flexion; extension, posterior knee splint
|
|
|
|
What type of contracture (deformity) typically occurs at the ankle? What position should be used for prevention or correction?
|
Plantarflexion; Dorsiflexion or splinted in neutral with AFO |
|
|
|
Dressing Choice Flowsheet |

|
|
|
|
Rule of Nines Image |
|
|

