![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
Biopsy or Observation for Lymphadenopathy?
>40 years |
Biopsy
|
|
|
Biopsy or Observation for Lymphadenopathy?
Location: cervical, inguinal, axillary |
Observation
|
|
|
Biopsy or Observation for Lymphadenopathy?
Size >2 cm |
Biopsy
|
|
|
Biopsy or Observation for Lymphadenopathy?
Tenderness present |
Observation
|
|
|
Biopsy or Observation for Lymphadenopathy?
Rock hard, fixed |
Biopsy
|
|
|
Biopsy or Observation for Lymphadenopathy?
Greater than 2 weeks |
Biopsy
|
|
|
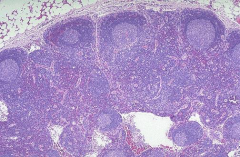
Benign reactive lymph node
|
|
|
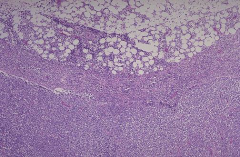
Diffuse D-cell Lymphoma
|
|
|
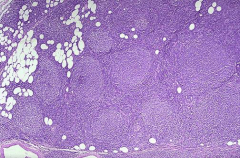
Follicular Lymphoma
CD10+ |
|
|
CD5- and CD10-
|
MALT lymphoma
|
|
|
CD23+, CD5+, FMC7-
|
CLL/SLL
|
|
|
CD23-, FMC7+, CD5+
|
Mantle cell lymphoma
|
|
|
effect of increased Bcl-2
|
decreased apoptosis; accumulation of mutations/transformation and proliferation
|
|
|
Cyclin D1
|
t(11;14) MCL
|
|
|
BCL-2
|
Follicular cell t(14;18)
|
|
|
t(8;14)
|
Burkitt's NHL
|
|
|
NF-kB inhibitor
|
t(11;19); CLL
|
|
|
What are the two most common NHL
|
Follicular and Diffuse Large B-Cell lymphoma
|
|
|
Presenting symptoms of non-Hodgkin's lymphoma
|
Painless enlargement of lymph nodes
Presence of B symptoms Back pain Severe fatigue Swelling, epecially in ankles or legs Severe fatigue |
|
|
Clinical features of NHL
|
Lymphadenopathy
Splenomegaly-(early satiety, LUQ pain) Hepatomegaly Skin Infiltration B symptoms CBC abnormalities |
|
|
Stage one (Ann Arbor Staging)
|
Localized disease
Single lymph node region Single organ outside of the Lymph Nodes |
|
|
Stage 2 (Ann arbor)
|
Two or more lymph node regions near to each other
|
|
|
Stage 3 (Ann Arbor)
|
2 or more lymph node regions in different parts of the body
|
|
|
Stage 4 (Ann Arbor)
|
Widespread disease
Multiple organs With or without lymph node involvement |
|
|
Tx for Diffuse Large B-cell Lymphoma
|
Chemo-immunotherapy
•Cyclophosphamide (Cytoxan) •Doxorubicin (Adriamycin) •Vincristine (Oncovin) •Prednisone •Rituximab (Rituxan) Referred to as R-CHOP (or CHOP-R) Administered every six weeks x 6 cycles |
|
|
Hemorrhagic cystitis side effect
|
Cyclophosphamide
Acrolein is a highly reactive aldehyde--associated with sterile hemorrhagic cystitis MESNA mops up the acrolein and prevents hemorrhagic cystitis |
|
|
Side effects of Vincristine
|
Peripheral Neuropathy, neurotoxicity
Alopecia, constipation |
|
|
Side effects of Doxorubicin
|
Cardiotoxicity
|
|
|
Bind tubulin; block polymerization of microtubules
|
Vincristine
|
|
|
Mech of Doxorubicin
|
Binds DNA/topoisomerase II
Causes lipid peroxidation and free radical damage Intercalates in DNA, distorts DNA helix |
|
|
Monoclonal Ab that binds to CD20 on cell surface of B lymphocytes (>90% of non-Hodgkins lymphomas)
Bound antibody recruits immune cells-->cell lysis |
Rituximab
|
|
|
lactate dehydrogenase
|
Non specific marker; goes up when cells are proliferating; extra-nodal sites
|
|
|
RICE chemo drugs
|
Rituxan, Ifosfamide, Carboplatin, and Etoposide (RICE)
|
|
|
Platinum coordination complex that causes DNA crosslinks
|
Carboplatin
|
|
|
Irreversibly binds/stabilizes DNA-topoisomerase II complexes
|
Etoposide
|
|
|
Side effects of ifosfamide
|
Like cyclophosphamide (GI, alopecia, myelosuppression)
•Additional: nephrotoxicity, neurotoxicity (encephalopathy) - related to chloroacetaldehyde metabolite |
|
|
Lymphadenopathy in kids may be d/t generally
|
cellular hyperplasia, cellular infiltration, or reactive tissue edema
|
|
|
Enlarged nodes in neonates
|
should prompt consideration of congenital infections such as toxoplasmosis or CMV
In general, newborns should not have palpable lymph nodes, though may have congenital lesions that could mimic a node |
|
|
will frequently have “shotty” nodes in the head and neck, axillary, or inguinal regions, even when otherwise healthy.
|
Older infants and younger children
Pre-school and early school aged children are constantly bombarded with viruses! |
|
|
School-aged children and adolescents lymph node prevalence
|
will less frequently have palpable nodes
|
|
|
Inguinal Adenopathy
|
STIs in teenages
|
|
|
Size thresholds for locations
Inguinal Head and Neck |
Inguinal-1.5 cm
Head and Neck-1 cm |
|
|
Left sided supraclavicular adenopathy
|
from thoracic duct; probably some abdominal cancer
|
|
|
Differential for generalized lympadenopathy Child
|
Viral, EBV, EMV, HIV, Toxo
|
|
|
Differential for generalized lympadenopathy: INfant
|
syphillis, Toxoplasmosis, CMV, HIV
|
|
|
Differential for generalized lympadenopathy: Adolescent
|
Viral, EBV, CMV, HIV, Toxo, syphilis
|
|
|
Tenderness of lymph node
|
indication of infection and may be associated with overlying skin changes such as redness or swelling
|
|
|
Hard nodes are indicative of
|
Fibrosis secondary to cancer or previous infection
|
|
|
Firm and rubbery nodes
|
may indicate lymphomatous
|
|
|
Fixing and matting nodes are signs of
|
infiltrative changes
|
|
|
Acute lymph node enlargements
|
More likely to be infectious
|
|
|
Acute cervical lymphadenitis
|
recent upper respiratory tract infection with resolution, followed by new development of left-sided neck swelling, redness, and fevers. No new exposures from initial history.
|
|
|
Post viral lymph node syndrome presents with
|
Abdominal pain
|
|
|
Strawberry tongue, extremitiy changes; 5 day history of fever, rashes
|
Kawasaki disease
|
|
|
Acute bilateral (reactive) lymphadenopathy
|
lymphoid hyperplasia usually secondary to a head and neck infection. Typical pathogens include the following:
–RSV, adenovirus, influenza, other viral upper respiratory tract pathogens (also maybe EBV and CMV) |
|
|
frequently bacterial in nature, with either Staphylococcus aureus or group A streptococcal species being implicated
|
Acute unilateral cervical lymphadenitis
Other important pathogens include oral flora, including anaerobes, from poor dentition The presence of bacterial species in a lymph node incites a localized inflammatory reaction |
|
|
–Tuberculosis
–Atypical mycobacteria –Bartonella henselae infection (cat scratch disease) |
Chronic cervical lymphadenopathy
|
|
|
Non-Infectious etiologies of cervical lymphadenopathy
|
Malignant
Immunologic Endocrinologic |
|
|
First line drug options for Acute unilateral cervical lymphadenitis
|
–Cephalexin, clindamycin, amoxicillin+clavulanate
|
|
|
Tx for Cat-scratch disease
|
Azithromycin: caution-get a PPD first
Ciprofloxacin, rifampin, TMP/SMX Resistant to B-lactams Bartonella henselae is bug |
|
|
Tx for Mycobacterium avium-intracellulare
|
Clarithromycin, rifabutin
|

