![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back

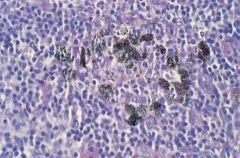
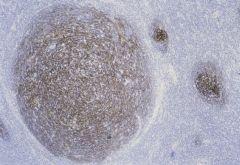
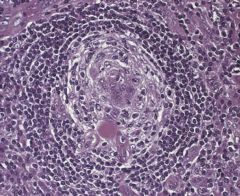
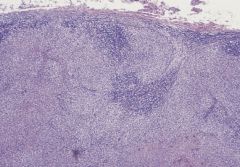
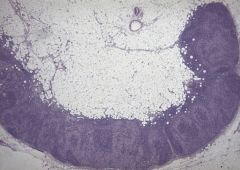
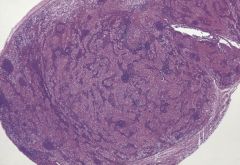
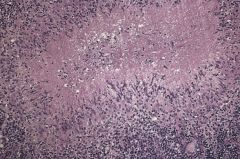
What is this
|
Rheumatoid lymphadenopathy: lymph node stained with methyl-green pyronin.The node shows follicular hyperplasia with numerous red (pyroninophilic)
plasma cells in the medullary cords. |
|
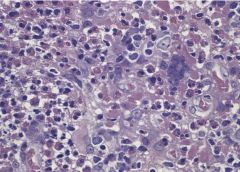
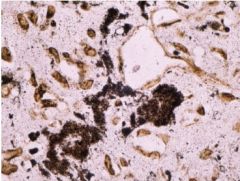
Axillary lymph node, what are the pigments?
|
‘Gold lymphadenopathy’. Axillary lymph node from a patient with rheumatoid disease treated with
colloidal gold. Black pigment is seen within histiocytes |
|
|
Does germinal center express BCL-2?
|
No. Therefore there are a lot of apoptosis of B-cells in the germinal cell. Only the selected ones are allowed to have BCL-2 expressed when they exit the germinal center.
|
|
|
In the paracortex, there are these monocytoid cells, what are they called? What do they expressed?
|
They are "plasmacytoid monocytes", once used to be called T-cells, but they express CD68 or CD4, not T-cells.
|
|
|
Where does B-cell development begin?
|
In bone marrow.
|
|
|
What are the phenotypes of B lymphoblasts in the bone marrow?
|
IgM, IgD, naive B cells with CD5 expression.
|
|
|
Where do these lymphoblasts go next?
|
To primary follicles and mantle zone of secondary follicles. Therefore, there are malignancies that derive from these cells with CD5 positivity such as CLL and Mantle cell lymphoma.
|
|
|
What makes the naive B cell in the lymph node (in primary follicles and mantle zone of secondary follicles) transform?
|
Antigenic stimulation.
|
|
|
If the lymphoblasts are stimulated by antigen what do they do next? What is the name of the cell type they turn into?
|
They migrate to the center of primary follicle and form germinal center of the secondary follicle, and turn themselves into centroblasts.
|
|
|
Describe cytology centroblasts. What are their phenotype?
|
Large with vesicular chromatin, and several eccentrically located nucleoli. Express BCL-6, CD10 but NOT BCL-2 (therefore susceptible to apoptosis),
|
|
|
What do centroblasts do in the germinal centers.
|
Hypermutation. Somatic hypermutation of their rearranged variable region genes, developing high affinity to the antigen stimulating them in the first place.
|
|
|
Describe centrocytes?
|
Intermediate sized cells with cleaved nuclei and inconspicious nucleoli. Those who developed high affinity to antigen are "rescued" by expressing BCL-2, therefore preventing apoptosis.
|
|
|
What are the lymphomas derived from germinal center B-cells?
|
Follicular lymphoma and Burkitts, and a subset of diffuse large B-cell lymphoma.
|
|
|
Where do centrocytes go next?
|
They turn into memory B-cell or plasma cells. With the help of follicular dendritic cells through CD23 and T-cells through CD40 ligand, the BCL-6 expression is switch off and they exit the germinal center and go into the mantle zone if they become memory cells. If they become plasma cells, they go to the bone marrow.
|
|
|
What are the phenotypes of these memory cells who are derived from centrocytes?
|
IgM+. But they have switched off IgD, CD5, CD10, CD23 and BCL-6.
|
|
|
What are the phenotypes of plasma cells derived from these centrocytes?
|
Lack all B-cell markers, no IgM or IgD (lack surface immunoglobulin). Express CD79a, CD138 and cytoplasmic IgG or IgA
|
|
|
What are the two basic classes of T cell base on the differences of TCR?
|
95% are alpha-beta TCR. 5% gamma delta.
|
|
|
How is T-cell with TCR gamma-delta different? Where do you see them?
|
Mostly in gut and spleen. They DO NOT express CD4 or CD8! They
|
|
|
What do TCR complex with?
|
CD3's gamma, delta, and epsilon chain.
|
|
|
How is NK cell different from T-cell?
|
NK cells do not have a complete TCR, they usually express only the epsilon part of CD3. Hence they stain CD3 if polyclonal CD3 stain is used.
|
|
|
Phenotype of NK cells? What do they look closest to?
|
Look closest to CD8+ T, they express CD2, CD7, CD8, CD56, CD57, granzyme B, perforin, T-cell intracellular antigen 1 (TIA-1).
|
|
|
Hypercalcemia. What malignancy?
|
Adutl T-cell leukemia
|
|
|
Hemophagocytic syndrome. What malignancy?
|
T-cell or NK-cell malignancies.
|
|
|
Severe neutropenia. What malignancy?
|
T-cell granular lymphocyte leukemia.
|
|
|
Patient with edema, pleural effusion, ascites, arthritis, anemia, polyclonal hypergammaglobinemia. What do you think of?
|
Angioimmunoblastic T-cell lymphoma.
|
|
|
A lymph node with follicular hyperplasia. What is your differential?
|
Non-specific follicular hyperplasia
Rheumatoid lymphadenopathy Syphilis Toxoplasmosis Kimura disease Measles Human immunodeficiency virus (HIV) lymphadenitis Progressive transformation of germinal centres Castleman disease |
|
|
Enlarged germinal centres may contain amorphous periodic acid–Schiff (PAS)-positive hyaline deposits and infrequently
sarcoid-like granulomas may accompany the follicular hyperplasia. Large numbers of plasma cells, often with Russell bodies, infiltrate the medullary cords and may also be present within germinal centres. What does this describe? |
Rheumatoid lymphadenopathy (mainly produce follicular hyperplasia)
|
|
|
Persistence of the organisms with
continuous antigenic stimulation of B- and T-cells. And is represented by marked follicular hyperplasia that extends into the medulla. This is accompanied by expansion of the paracortex and marked fibrosis of the capsule, the fibrosis sometimes penetrating into the node. Plasmacytosis is prominent within the medullary cords. Small non-caseating epithelioid granulomas are sometimes present with single so-called naked giant cells in the paracortex. There is arteritis and phlebitis. What is this? |
Syphilis lymphadenopathy. Accompany all three stages of syphilis. Treponema pallidum --> chancre --> mucosal ulcers or lymphadenopathy --> gammata
|
|
|
Oriental male with lymphadenopathy that show follicular hyperplasia, paracortical expansion with prominent high endothelial venules and marked eosinophilic infiltration. There is often a proteinaceous precipitate in the germinal centres and
immunostains reveal immunoglobulin E (IgE)Serum IgE very high. What does he has? |
Kimura. Lymph nodes may appear matted. Regress on its own.
|
|

Lymph node. What is this.
|
Kimura disease. High-power view of the
follicle containing an eosinophil microabscess. |
|
Lymph node. What is this?
|
Kimura disease. Follicle centre largely
replaced by eosinophils and amorphous eosinophilic material. Also shown is a follicular dendritic cell polykaryon. |
|

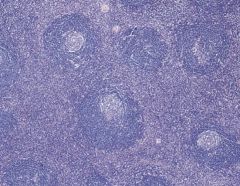
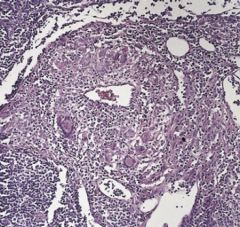
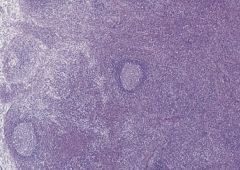
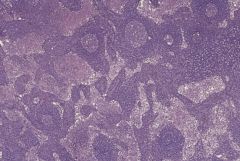
Lymph node. What is this?
|
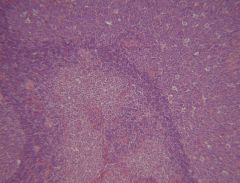
Human immunodeficiency virus lymphadenopathy.
Lymph node showing follicular hyperplasia with large irregular germinal centres. Islands of pale-staining monocytoid B-cells can be seen in the centre of the field. Second slide shows Human immunodeficiency virus lymphadenopathy. High-power view showing part of a germinal centre and an island of monocytoid B-cells. |
|
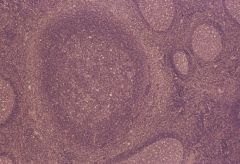
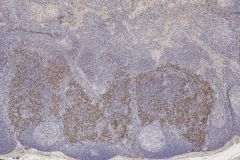
Lymph node from the young adolescent with cervical lymphadenopathy. What is this? What stain would you use to confirm?
|

Progressive transformation of germinal
centres. Section stained for CD79a showing strong positive staining of mantle cells.The ‘transformed’ follicle is expanded and broken up by mantle cells. Staining for immunoglobulin D would show a similar appearance. |
|
This is CD21 stain on the lymph node of progressive transformation of germinal center. What does it demonstrate?
|
Progressive transformation of germinal
centres. Section stained for CD21 showing follicular dendritic cells.The ‘transformed’ follicle shows an expanded of follicular dendritic cells in comparison with the tight networks seen in the adjacent reactive follicles. |
|
|
What does HIV lymphadenitis associated with burnt out stage lymphadenitis?
|
Human immunodeficiency virus shows strong tropism for lymphoid tissues, especially CD4-positive T-cells,
monocytes and dendritic cells. The result of continued infection causes cytopathic destruction of CD4 positive T-cells and dendritic cells in germinal centres so that the latter involute. The progression as follows: 1) florid follicular hyperplasia; 2) mixed follicular hyperplasia and follicular involution; 3) follicular involution; 4) lymphocyte depletion. |
|
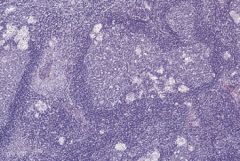
25 year old presented with mediastinal mass/lymphadenopathy. Section shows lymph node. What is the differential?
|
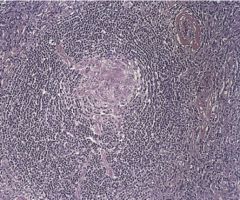
Castleman disease, hyaline vascular type. Follicle showing hyalinization of the germinal centre with penetrating vessels, onion-skin layering of the mantle cells and vascularized interfollicular tissue. Note hyalinized follicles and lack of sinus structures in the first picture.
|
|
|
Buzz words for what disease:
1) Most common in young adults 2) Commonly presents in mediastinum 3) Hyaline follicles consist mainly of endothelial cells and dendritic reticulum cells 4) Mantle zone shows onion-skin layering 5) NO systemic symptoms ■ Interfollicular areas vascular ■ Sinus structure not usually visible |
Hyaline Vascular Castleman Disease
|
|
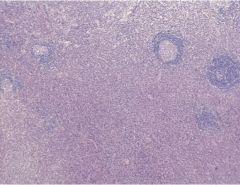
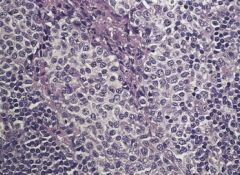
This is also castleman disease. How is it different from the previous castleman?
|
Castleman disease, plasma cell variant. Reactive follicles in a background of plasma cells. No sinus structure visible. Hyalinized follicle composed mainly of dendritic and endothelial cells surrounded by plasma cells.
|
|
|
What do the following describe?
■ Wide age range ■ Systemic symptoms ■ Anaemia, hyperglobulinaemia, elevated erythrocyte sedimentation rate (ESR), increased plasma cells in bone marrow ■ Abdominal nodes most commonly involved ■ Follicular hyperplasia with narrow mantle zones ■ Dense interfollicular infiltrate of plasma cells obscures underlying architecture ■ One-third of cases show light-chain restriction |
CASTLEMAN DISEASE PLASMA CELL VARIANT – LOCALIZED
|
|
|
What is POEMS syndrome? What lymphadenopathy is it associated with?
|
Polyneuropathy, organomegaly, endocrine abnormalities, monoclonal gammopathy, skin rashes. Associated with MULTICENTRIC CASTLEMAN DISEASE. This is seen in older patients, associated with HIV, infection Kaposi sarcoma, plasma cell neoplasms, malignant lymphomas and autoimmune disease. The underlying pathogenesis appears to be the overproduction of IL-6 either from endogenous sources or from the viral homologue of IL-6 produced by human herpes virus 8 (HHV-8). Histology looks like localized form of Castleman.
|
|
What is happening in this lymph nod?
|
Syphilitic lymph node showing marked venulitis with giant cells
|
|
This patient lives with cat.
|
Toxoplasmosis.The epithelioid cell clusters appear to encroach on and enter the germinal centres.A collection of monocytoid B-cells is seen between the two germinal centres. Second pic shows prominent monocytoid B-cells distributed in and around a sinus
|
|
|
What are the following entities have in common?
Dermatopathic lymphadenopathy Kikuchi–Fujimoto disease Systemic lupus erythematosus Viral lymphadenitis, including infectious mononucleosis Drug-induced lymphadenopathy |
Paracortical expansion
|
|
|
Young Asian female presented with painful cervical lymphadenopathy and fever. Lymph node sections show paracortical expansion with small lymphocytes, plasmacytoid monocytes, blast cells, and histiocytes. NO plasma cells. NO neutrophils. There are wide spread apoptosis and necrosis. The phagocytic histiocytes have crescentic nuclei. Diagnosis?
|
Kikuchi
|
|
Those areas of the lymph node are wide spread apoptosis and necrosis with disruption of architecture. What is it?
|
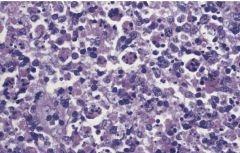
Blast cells with numerous apoptotic bodies in the background.
|
|
This is the lymph node from a young boy with paracortex expanded by large cell and blast cells and apoptotic nuclei. What is it?
|
Infectious Mononucleosis Lymphadenitis with the following features:
■Teenagers and young adults affected ■ Paracortical expansion ■ Numerous B- and T-immunoblasts present in paracortex ■ Atypical Hodgkin/Reed Sternberg-like cells may be seen, but are more common in the tonsil than in lymph nodes IgM will highlight the blastic B-cells in the paracortex |
|
Axillary lymph node showing expanded pale-staining paracortex.
|
Dermatopathic lymphadenopathy:
■ Superficial lymph nodes draining chronic dermatoses ■ Cut surface of node may show subcapsular rim of pigment ■ Paracortical expansion with aggregates of interdigitating reticulum cells and Langerhans cells ■ Scattered macrophages containing lipid and melanin Section stained for S100 protein showing the expanded network of interdigitating reticulum cells in the paracortex. |
|
You see paracortical expansion and eosinophils, what process is this?
|
Drug-induced lymphadenopathy. Patient often has history of drug use, fever, skin rash, lymphadenopathy, blood hypereosinophilia, Paracortical expansion usually involves eosinophils. May have small area of necrosis.
|
|
|
What is common among the following:
Rosai–Dorfman disease (sinus histiocytosis with massive lymphadenopathy) Langerhans cell histiocytosis Lipogranulomatous reaction Silicone lymphadenopathy Storage diseases |
Sinus histiocytosis
|
|
Is this follicular hyperplasia, paracortex hyperplasia or sinus histiocytosis.
|
Sinus histiocytosis.
|
|
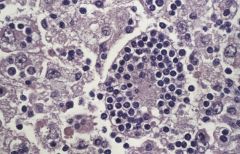
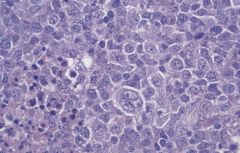
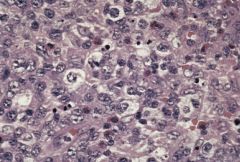
What is going on here? What disease/process is associated with this?
|
Rosai–Dorfman disease. High-power view showing lymphophagocytic histiocytes. The above picture shows prominent sinus histiocytosis.
|
|
|
Lymphadenopathy presented most commonly in childhood and young adult life and with following characteristics is most likely what?
■ Cervical lymphadenopathy most common presentation ■ May occur at other nodal and extranodal sites ■ Fever, night sweats, weight loss, malaise and arthralgia may occur ■ Anaemia, hypergammaglobulinaemia and raised erythrocyte sedimentation rate (ESR) frequent ■ Capsular fibrosis ■ Sinuses expanded by histiocytes with rounded nuclei, prominent nucleoli and abundant cytoplasm ■ Histiocytes engulf lymphocytes and other haematopoietic cells ■ Large numbers of plasma cells in medullary cords |
Rosai-Dorfman Disease.
|
|
|
Does Rosai-Dorfman has large number of plasma cells?
|
Yes. In the intervening medullary cords.
|
|
|
How the histiocytes in Rosai-Dorfman different from histiocytes in reactive sinus histiocytosis?
|
The histiocytes in Rosai-Dorfman are CD68 positive, whereas in others, are S100 positive (indicating origin from antigen presenting cell). All negative for CD1a (Langerhans cells histiocytosis).
|
|
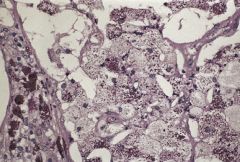
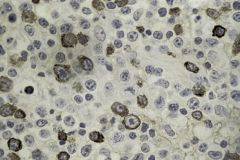
If this is a lymph node from the mesentery, what do you think it is?
|
Whipple disease. Periodic acid Schiff stained section showing large numbers of bacilli in foamy histiocytes. In lepromatous leprosy, the foamy histiocytes are seen mostly in the paracortex; and AFB shows acid fast bacilli.
|
|
What is the causative agent for Cat Scratch Disease. What systemic disease does it cause?
|
Bortonella hensalae. A Gram positive coccobacilli stained positive for Warthin Starry stain. Cat scratch disease is the most common cause of suppurative granulomatous lymphadenitis and may show systemic involvement including suppurative hepatosplenic granulomas and osteomylitis. Bacillary angiomatosis.
|
|
|
How is suppurative granulomatous lymphadenopathy different from epithelioid granulomatous lymphadenitis.
|
Suppurative granulomatous lymphadenitis generall represents a B-cell-associated granulomatous reaction that is different from the hypersensitivity type or epithelioid granulomatous lymphadenitis seen in tuberculosis, leprosy and sarcoidosis. Suppurative granulomas often appear to start as an accumulation of monocytoid B-cells followed by polymorph infiltration with necrosis developing in these foci, leading eventually to granuloma formation. This contrasts with the formation of epithelioid granulomas of the hypersensitivity- type, which appears to be mediated by activated T-cells, dendritic cells and histiocytes without the participation of B-cells. Suppurative granulomas are distinguished from the hypersensitivity-type granulomas by the presence of neutrophils, prominence of monocytoid B-cells and a paucity of multinucleated giant cells.
|
|
|
Examples of suppurative granulomatous lymphadenopathy?
|
Bartonella henselae (cat scratch disease)
Chlamydia trachomatis (lymphogranuloma venereum) Francisella tularensis (tularaemia) Yersinia enterocolitica, Y. pseudotuberculosis |

