![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
To what extent do the pulmonary arteries accompany the airways in their branching pattern and outreach in the lung parenchyma?
|
The airways are accompanied by a similar size pulmonary artery and branch in a similar pattern down to airways prior to respiratory bronchioles. At that level, pulmonary arteries usually start losing their smooth muscle cells (i.e., vessels measuring less than 70 micros in diameter) and progressively taper off into alveolar capillaries.
|
|
|
What is the approximate size equivalency between the pulmonary arteries and their accompanying airways?
|
They are of approximate size both in the hilum as well as in the peripheral of the lung, down to the area corresponding to the respiratory bronchioles.
|
|
|
What is the characteristic histological landmark of large, medium and small pulmonary arteries?
|
Large pulmonary arteries are composed predominantly by an elastic medial layer with few interspaced smooth muscle cells. They measure from 20 mm in diameter down to .5 mm in diameter. The medium sized pulmonary arteries are characterized by a prominent and well-defined medial layer composed of smooth muscle cells with interspaced elastic fibers. Small pulmonary arteries usually are located below the size of 70 microns in diameter and they have progressively similar medial smooth muscle cell layer, eventually loosing the smooth muscles cells and acquiring a pericitic layer.
|
|
|
Does the presence of intima thickening automatically imply in the presence of pulmonary hypertension?
|
Intima thickening, of mild extent, may be present in a normal lung and in normal pulmonary arteries. However, extensive (both in distribution as well as the extent to which it impacts the blood vessel lumen) is predominantly seen in pulmonary hypertension.
|
|
|
What is the size range in which the medium size pulmonary arteries loose their medial smooth muscle cells?
|
Approximately 70 microns in diameter.
|
|
|
What are the cellular layers of the pulmonary arteries in the size range below 70 microns in diameter?
|
Intima with endothelial cells, a layer of connective tissue with embedded pericytes
|
|
|
Why is it important to have a low perfusion pressure at the level of the pulmonary capillaries?
|
Perfusion pressure is a key determinant of the driving force to move water out of the capillaries into the alveolar space. A low perfusion pressure assures a low hydraulic pressure, contributing to the retention of fluid within the capillaries rather than in alveolar space. Increase in venous pressures such as left heart failure causes acute and chronic passive congestion with increased loss of fluid into alveolar spaces. The fluid is pumped back by Na/K ATPases in epithelial cells and the remainder drains via the lymphatics.
|
|
|
Is it possible to distinguish pulmonary veins from pulmonary arteries at the histological level?
|
No. The only approach that we allow is the distinction between pulmonary arteries from pulmonary veins is either three dimensional reconstruction of the intraparenchymal pulmonary veins and establishment of their connection with interlobular septal veins in the subpleural space.
|
|
|
What is the definition of pulmonary hypertension?
|
Pulmonary hypertension is defined by increase in pulmonary artery pressure above 25mmHg at rest 30mmHG during exercise.
|
|
|
How can pulmonary hypertension be classified etiologically and by site of involvement?
|
Pulmonary hypertension can be divided into idiopathic (example idiopathic pulmonary arterial hypertension) or pulmonary hypertension associated with underlying diseases.
|
|
|
Which is the gender most frequently compromised by idiopathic pulmonary arterial hypertension (IPAH)?
|
Women are compromised at rates of 3 to 4:1 in relation to man.
|
|
|
List three diseases that are associated with pulmonary arterial hypertension:
|
Congenital heart malformations with left to right shunting, collagen vascular disease, HIV infection
|
|
|
What are the pressure levels that define mild/moderate and severe pulmonary hypertension?
|
Mild to moderate pulmonary hypertension occurs when the pulmonary artery pressure are in the levels of 40-45mmHg. Severe pulmonary hypertension occurs when the pulmonary artery pressure are in access of 45mmHg, often times at the levels of systemic arterial pressures
|
|
|
Why is it important to differentiate mild/moderate vs. severe pulmonary hypertension?
|
Severe pulmonary hypertension is mostly irreversible and therefore carries a high mortality, whereas mild to moderate pulmonary hypertension can be treated by addressing the underlying condition causing the pulmonary hypertension.
|
|
|
What is the most common cause of death in patients with severe pulmonary hypertension?
|
Right heart failure.
|
|
|
List the cells that participate in the intimal component of pulmonary vascular remodeling in pulmonary hypertension:
|
Endothelial cells and smooth muscle cells that have migrated from the medial and behave as myofibroblasts.
|
|
|
What are the critical cells that participate in intimal and medial thickening in pulmonary arteries with pulmonary hypertension?
|
Endothelial and smooth muscle cells
|
|
|
What are the alterations present in the large elastic pulmonary arteries in pulmonary hypertension?
|
The large pulmonary arteries undergo atherosclerotic changes, morphologically similar to those seen in systemic arteriosclerosis.
|
|
|
Is pulmonary artery artherosclerosis specific of particular forms of pulmonary hypertension?
|
Atherosclerosis of pulmonary arteries is not specific of any particular form of pulmonary hypertension. It is usually more prominent with more severe forms of pulmonary hypertension
|
|
|
Can medial hypertrophy distinguish between mild/moderate vs severe pulmonary hypertension?
|
Medial smooth muscle cell hypertrophy cannot accurately discriminate between mild to moderate vs. severe pulmonary hypertension. The final diagnosis relies on pulmonary hemodynamics.
|
|
|
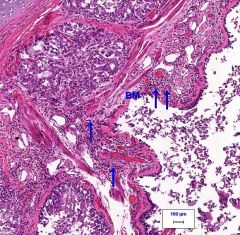
Which is the intimal lesion that categorically distinguishes severe vs mild/moderate pulmonary hypertension?
|
The characteristic plexiform lesion distinguishes severe vs mild/moderate pulmonary hypertension. Plexiform lesions correspond to an abnormal proliferation of endothelial cells in the vascular lumen pulmonary arteries.
|
|
|
List the diseases that cause endothelial cell dysfunction in severe pulmonary hypertension:
|
Idiopathic pulmonary arterial hypertension, HIV, liver cirrhosis, collagen vascular disease, congenital heart malformation with left to right shunting.
|
|
|
What is the genetic basis of the familial form of primary or idiopathic pulmonary hypertension?
|
The genetic basis of the familial form of pulmonary hypertension is germline mutations in one copy of the bone morphogenetic protein receptor2. In idiopathic pulmonary hypertension somatic (lesional) mutations of transforming growth factor receptor 2 have been identified in lungs with pulmonary arterial hypertension.
|
|
|
What is the frequency of individuals with mutated bone morphogenetic protein receptor 2 who develop pulmonary hypertension?
|
Approximately 50 percent of family members with pulmonary arterial hypertension have mutations of the bone morphogenetic protein receptor 2. Only 20 percent develop pulmonary hypertension.
|
|
|
What is the mortality rate of patients with pulmonary embolization?
|
The mortality rate is 10 – 30 percent.
|
|
|
What is the frequency of pulmonary infarction after pulmonary embolization and what is the requirement for the development of pulmonary embolization and what is the requirement for the development of pulmonary hypertension after pulmonary embolization?
|
Pulmonary infarction occurs in 10 – 20 percent of patients with pulmonary embolization, usually in patients with left heart side failure.
|
|
|
ADALECTASIS: alveolar walls are juxtaposed because air is no longer distending the alveoli
|
|
|
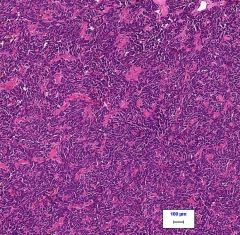
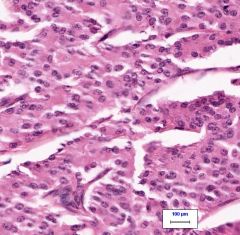
Small Cell Carcinoma of Lung: Invasive, with very high nuclear to cytoplasmic ratio, very uniform in appearance with highly chromatophillic nuclei with many mitoses
Small cells resemble lymphocytes, with some signs of neuroendocrine differentiation. Aggressive, metastasize widely and are non-resectable. Genetics: p53 Diagnose with sputum cytology or brochoscopy because of central location. |
|
|
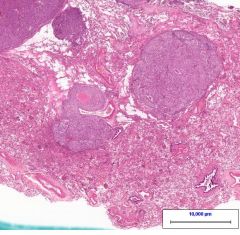
Metastatic carcinoma to the lung: can tell because of the multiple nodules seen in the lung parenchyma, this is melanoma, but many cancers can metastasize to the lung.
|
|
|
ASTHMA: Note over distention and mucous plugs. Thickened basement membrane, numerous eosiniphils, prominent submucosal glands, hypetrophic smooth muscle in airways.
|
|
|
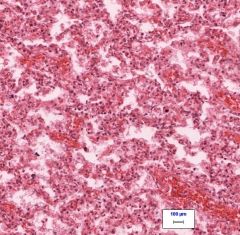
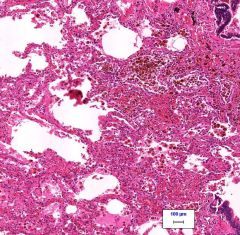
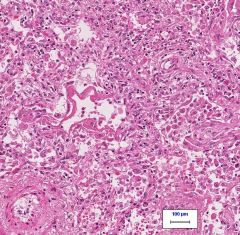
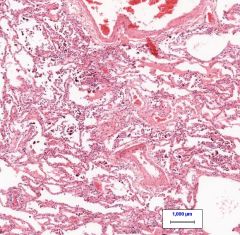
Chronic passive lung congestion:
Note erythrocytes in septal capillaries, hemosiderin laden macrophages in lung Patient has history of CAD with multiple MIs, also presentw with ansarca, palpable liver and spleen. Cough is mildly productive, sputum stains positive for iron. |
|
|
Squamous cell carcinoma: Invasive neoplasm, tightly cohesive, epitheliod, with keritinaceous whorls and pearls. Poorly differentiated with some focal squamous differentiation. Large tumors can have necrotic centers. Found in centrally, in large airways.
Clinically occurs mostly in smokers, present with weight-loss, productive cough, and fatigue. On chest x-ray, well circumscribed nodules can be seen. Diagnose with sputum cytology and bronchoscopy. |
|
|
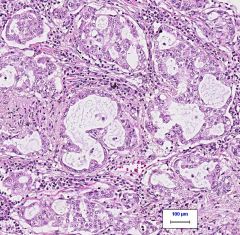
ADENOCARCINOMA of lung: Gland forming carcinoma with abundant luminal secretions (mucin stain +) with surrounding desmoplastic response. Cytoplasm is delicate.
Clinically pt presents with weight-loss and fatigue, will often have a history of smoking, and dyspnea with chest pain. Genetics: EGFR and Ki-ras - reciprocal associated with adenocarcinoma. EGFR mutated cancers are responsive to EGFR inhibitors, but they do not change survival. Diagnose with transthoracic aspriate or open lung biopsy (because they are more peripheral). |
|
|
Carcinoid tumor of lung: Located centrally near large airways, major morbidity from obstruction of said airway. Derived from neuroendocrine cells in the lung, they have variable malignancy. Small, round cells surrounded by capillaries.
Do NOT progress to small cell carcinoma. Excellent prognosis. |
|
|
Bronchoalveolar carcinoma (BAC)
|
A subtype of adenocarcinoma of the lung that is seen as lepidic grwoth pattern (meaning that it follows the walls of the alveoli without invasion).
Clinically it mimics pneumonia: intersitial opacity on CXR and productive cough. |
|
|
Atypical adenomatous hyperpasia
|
Non-invasive pulmonary neoplasia that resembles adenocarcinoma in its formation. Much like BAC but AAH is NON-INVASIVE and is <8mm. No evidence to support that this is pre-adenocarcinoma.
|
|
|
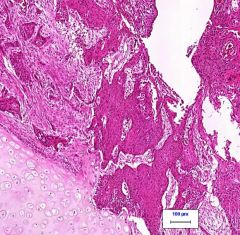
Mseothelioma
|
Cancer caused mostly by asbestos - cancer of the mesothelial lining (plural surface) of the lung. Causes thickening and adhesion of pleura to lung. Poor prognosis.
|
|
|
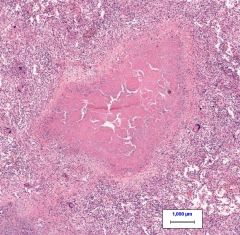
Tuberculosis
|
|
|
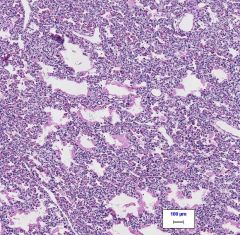
DIFFUSE ALVEOLAR DAMAGE
-Alveolar architechture still in tact -No fibrosis -Hyaline membranes -Acute process -Interstitium is widened but not fibrotic |
|
|
Hyaline Membrane disease of a newborn:
|
|
|
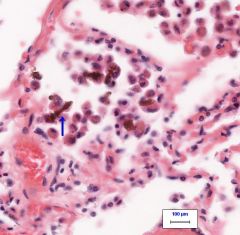
ASBESTOSIS BODY:
-Forms around asbestosis fibers -Not to be confused with hemosiderin laden macrophages |
|
|
ASBESTOSIS
-Fibrosis -msothelioma in pleural space |

