![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
What is fissure in ano? |
Longitudinal split in the anoderm of the distal anal canal, which extends from the anal verge proximally towards dentate line BUT not beyond it. |
|
|
Difference between posterior and anterior anal fissure |
Posterior Commonly seen in most anal fissure cases Anterior Commonly in females after vaginal delivery |
|
|
Difference between acute and chronic fissure in ano |
Acute Tear on the anal mucosa Chronic Acute fissure persist more than 6 weeks |
|
|
Causes of fissure in ano |
1. Constipation -Traumatisation of the anal mucosa by passage of hard stool
2. Chronic diarrhea (less commonly)
3. Vaginal delivery (anterior anal fissure)
4. STI / HIV / TB
5. IBD / Cancer
6. Pregnancy
7. Prior anal surgery
8. Anal sexual intercourse |
|
|
Risk factors fissure in ano |
1. Trauma (hard bowel movements, diarrhea, anal instrumentation, child birth) 2. Low fibre intake 3. Physiological stress (sustained tonic rise anal canal pressure) 4. Inflammatory bowel disease (Crohn’s D) |
|
|
Common complaint fissure in ano |
1. Severe pain during defecation (feel like broken glass passed through anal) 2. Passage of fresh blood 3. Itchiness (in chronic)
|
|
|
What can be seen during inspection of fissure in ano |
1. Hypertrophied anal papilla internally (chronic anal fissure) 2. Sentinel tag externally (chronic anal fissure) 3. Demarcated, fresh mucosal edges and granulation tissue (at the base of the fissure) |
|
|
What is the classic triad of chronic fissures |
1. Deep ulcer 2. Sentinel pile at the distal fissure margin 3. Enlarged anal papillae proximal to fissure |
|
|
What investigations done for fissure in ano? |
1. Examination under anaesthesia (particularly to exclude presence of occult perianal abscess or tumour in older patients) -secondary causes of anal ulceration. 2. Flexible sigmoidoscopy- determine cause of fissure (<50 y/o with no risk factors for intestinal disease or colon ca) 3. Colonoscopy- for pt >50y/o with abdominal sx like diarrhea. |
|
|
What is the treatment for acute anal fissure |
*main aim of the tx is to breaking the cycle of hard stool, pain and internal anal sphincter spasm* 1. Dietary modification- high fibre diet + increase water intake 2. Laxatives- syrup lactulose/liquid paraffin 3. Warm sitz baths- relieve symptoms 4. Avoidance of topical preparations of hydrocortisone and local anesthetics |
|
|
What is the tx of chronic anal fissures |
*main aim of tx is to reduce internal sphincter spasm and anal canal pressure* 1. Pharmacologic agents- topical nitroglycerin, CCB (nifedipine, diltiazem), botulinum toxin -to lower resting anal pressure and promote fissure healing 2. Surgery- Lateral internal sphincterotomy, Lord’s anal stretch, fissurectomy, lateral anal sphincterotomy (Notaras) and advancement flap anoplasty (reserved for refractory anal fissures) 3. Oral analgesics- avoid use of codeine (adverse effect of constipation) 4. Other oral and topical agents- bethanecol, indoramin, albuterol, sildenafil (decrease resting pressure of anal sphincter BUT not promoting healing) 5. F/up to assess outcome of tx |
|
|
Mdm Choo, a 30y/o Chinese woman presented to your clinic with a hx of severe pain on defecation for the last 1 month. she has noticed a small amount of blood on the stool and also on the toilet paper after wiping. the pain is severe and she felt like a broken glass passed through her anus, and it often persists for hours after defecation.
State FIVE causes of anorectal pain. |
1. Acute anal fissure
2. Thrombosed hemorrhoids
3. Peri-anal ulcer (Crohn's D, extrapulmonary TB or syphilis)
4. Anal fistula (infected with abscess formation)
5. Solitary rectal ulcer syndrome |
|
|
Mdm Choo, a 30y/o Chinese woman presented to your clinic with a hx of severe pain on defecation for the last 1 month. she has noticed a small amount of blood on the stool and also on the toilet paper after wiping. the pain is severe and she felt like a broken glass passed through her anus, and it often persists for hours after defecation.
What further histories would you like to obtain from this pt? |

Ask hx of TB, Crohn D and use of opiate analgesia - Extrapulmonary TB and Crohn D may be associated with anal fissures - Use of opiate analgesia is associated with constipations and subsequent increased incidence of anal fissure |
|
|
What is fistula in ano |
Fistula in ano is refers to an abnormal communication (tract) between the anal canal or rectum (deeply) and the perianal skin (superficially). |
|
|
What are the four main types of anal fistula according to Park’s classification? And which one is the most common? |
1. Inter-sphincteric (MOST COMMON) 2. Trans-sphincteric 3. Supra-sphincteric 4. Extra-sphincteric |
|
|
What is the classification for fistula in ano |

Park’s classification - Based on the relationship of tract with the external anal sphincter |
|
|
Explain the types of fistula in ano |
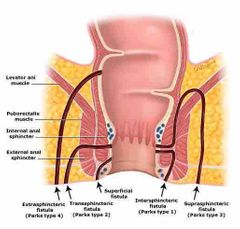
1. Inter-sphincteric - MOST COMMON - Begins at dentate line and ends at anal verge, tracking along the intersphincteric plan between the internal and external anal sphincters and terminates in perianal skin
2. Trans-sphincteric - Tracks through the external sphincter into the ischiorectal fossa, encompasses a portion of the internal and external sphincter and terminates in the skin overlying the buttock
3. Supra-sphincteric - RARE (usually due to iatrogenic) - Originates at the anal crypt and encircles the entire sphincter apparatus, terminates in the ischiorectal fossa
4. Extra-sphincteric - Commonly due to pelvic trauma, very high in anal canal, located proximal to the dantate line. It encompasses the entire sphincter apparatus including levator and terminates in the skin overlying the buttock |
|
|
What are the complications of anorectal abscesses? |
1. Fistula formation 2. Bacteremia and sepsis 3. Fecal incontinence 4. Malignancy |
|
|
What are the factors that contributing to recurrence of the anorectal abscess? |
1. Inadequate drainage of the abscess 2. Presence of unrecognised anal fistula 3. TB 4. Actinomycosis 5. HIV or immunosuppression |
|
|
What fascia anteriorly separates the rectum from prostate and seminal vesicles in men and from the vagina in women? |
Denonvillier’s fascia |
|
|
What is used clinically to predict the trajectory of a fistula tract |
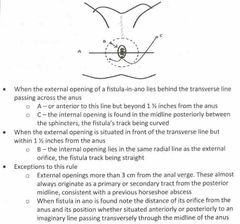
Goodsall’s rule |
|
|
What is the length of surgical anal canal? |
2 - 4cm Begins at anorectal juction and terminates at the anal verge Longer in men than women |
|
|
What is the dentate / pectinate line marks? |
The dentate / pectinate line marks the transition point between columnar rectal mucosa and squamous anoderm |
|
|
Causes of anorectal abscess |
1. Obstructed anal crypt originating at the dentate line 2. Extension of an infection of an anal gland 3. Hematogenous infections 4. Penetrating foreign bodies 5. Extension of cutaneous boil |
|
|
State level of fistula in ano |
Low level fistula (below ano-rectal ring) - Submucous - Inter muscular - Anorectal
High level fistula (above ano-rectal ring) - Total fistula secondary to local disease - Total fistula with high perforating secondary tract - High intersphincteric fistula starting as a primary anal gland |
|
|
Clinical presentation of pt with anorectal abscess |
1. Severe pain in the anal or rectal area - Pain is constant (not necessarily a/w bowel movement) exacerbated when sat down - Throbbing in nature
2. Localised swelling 3. Fever and malaise 4. Urinary retention (progressive infection) 5. Purulent rectal drainage |
|
|
Supralevator abscesses are typically a/w ? |
Pelvic pain and tenderness |
|
|
What positioning can be done to inspect pt with anorectal abscess? |
1. Left lateral position (Sim’s) 2. Knee-elbow position 3. Lithotomy position |
|
|
Where do the anorectal abscesses occur classically? Which one is the commonest? |
1. Perianal (MOST COMMON) 2. Ischiorectal 3. Inter-sphincteric 4. Supralevator 5. Submucosal |
|
|
Mr X, 45 y/o gentleman presented to the outpatient clinic due to peri-rectal pain a/w mild fever, generalised malaise, loss of appetite and chills, for 4 days duration. List FIVE differential diagnosis |
1. Anorectal abscess 2. Anal fissure 3. Thrombosed hemorrhoids 4. Pilonidal abscess 5. Perianal hidradenitis suppurativa |
|
|
What investigations can be done for anorectal abscess pt? |
1. FBC 2. Serum glucose - TRO DM (predisposed to abscess formation) 3. Renal profile - serum BUN and creatinine may be elevated, metabolic acidosis (decreased bicarbonate and increased base deficit) common in pt with necrotising soft tissue infections 4. Pus culture and sensitivity for antibiotic 5. CT or MRI - for nonpalpable anorectal abscess, complicated, unclear, or chronic disease (immunocompromised or those with ischiorectal abscesses) 6. Anoscopy (after pain subsides)- to determine whether anal fistula has developed as sequelae of abscess |
|
|
What is the outline of management of anorectal abscess? |
1. Antibiotic therapy, as guided by protocol
2. Sufficient analgesia
3. The main management for anorectal abscesses- incision and drainage procedure (always be performed under general anaesthetic) These can left to heal by secondary intention.
4. Once drained, proctoscopy should be performed (presence of any identifiable fistula-in-ano) |
|
|
What is the classification for fistula in ano |
Park’s classification - Based on the relationship of track with the external anal sphincter |
|
|
Explain the types of fistula in ano |
1. Inter-sphincteric - MOST COMMON - Begins at dentate line and ends at anal verge, tracking along the intersphincteric plan between the internal and external anal sphincters and terminates in perianal skin
2. Trans-sphincteric - Tracks through the external sphincter into the ischiorectal fossa, encompasses a portion of the internal and external sphincter and terminates in the skin overlying the buttock
3. Supra-sphincteric - RARE (usually due to iatrogenic) - Originates at the anal crypt and encircles the entire sphincter apparatus, terminates in the ischiorectal fossa
4. Extra-sphincteric - Commonly due to pelvic trauma, very high in anal canal, located proximal to the dantate line. It encompasses the entire sphincter apparatus including levator and terminates in the skin overlying the buttock |
|
|
Causes of fistula in ano |
1. Consequence of an perianal or submucous abscess bursting both outside and inside
2. Inadequate drainage of an ano-rectal abscess
3. Other associated risks factors |
|
|
Risk factors for the formation of fistula in ano |
1. IBD – Crohn’s disease or ulcerative colitis 2. Systemic diseases – Tuberculosis, diabetes, HIV 3. History of trauma to the anal region 4. Previous radiation therapy to the anal region |
|
|
Clinical presentation of pt with fistula in ano |
1. Presented with non-healing/ persistent anorectal abscess following drainage, or with chronic purulent drainage and a pustule-like lesion in the perianal or buttock area 2. Intermittent rectal pain (during defecation, also with sitting and activity) 3. Intermittent and malodorous perianal drainage 4. Pruritus 5. On PE, an external opening on the perineum may be seen (these can be fully open or covered in granulation tissue) 6. A fibrous tract may be felt underneath the skin on digital rectal examination. |
|
|
What is used clinically to predict the trajectory of a fistula tract |
Goodsall’s rule |
|
|
What investigations can be done in pt with fistula in ano |
1. Proctoscopy - May demonstrate inner opening of the fistula 2. Probing and sinogram -EUA (demonstrate tract of the fistula) 3. MRI - Gold standard for fistula imaging (reserved for difficult recurrent cases or view secondary extension that may be missed during surgery) 4. Fistulography and CT - useful for extra-sphincteric fistula 5. Barium enema - useful for pt with multiple fistula or recurrent disease TRO IBD |
|
|
What are the tx options for fistula in ano? |
1. Therapeutic intervention is indicated for symptomatic
2. Surgical tx is the mainstay of therapy *injection of hydrogen peroxide to detect internal opening of anal fistula*
3. Surgical options: - Fistulotomy - Ligation of the inter-sphincteric fistula tract (LIFT) - Mucosal advancement flap
4. Others: - Seton placement (single stage and two stage) - Fibrin glue - Bioprosthetic plug |

