![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
452 Cards in this Set
- Front
- Back
|
Knee joint is made up of what four bones?
|
femur, tibia, fibula, and patella
|
|
|
What are the three separate joints of the knee joint?
|
tibiofemoral, patellofemoral, and tibiofibular
|
|
|
Intercondylar notch is made up of what anteriorly and posteriorly?
|
Femoral trochlea anterior- patellar articulation.
Intercondylar notch posteriorly- reference for ligamentous attachments. |
|
|
Medial and lateral tibial condyles articulate with:
|
femoral condyles
|
|
|
Which tibial plateau is larger and why?
|
Medial to accommodate larger medial femoral condyle
|
|
|
Tibial tuberosity/tubercle is teh attachment site for:
|
infrapatellar tendon
|
|
|
What types of structures attach to fibular head?
|
muscles and ligaments
|
|
|
Superior pole of patella is for what attachment?
|
quad attachment
|
|
|
Inferior pole of patella attaches to:
|
infrapatellar tendon
|
|
|
Prepatellar bursa is where and does what?
|
covers patella anteriorly to protect it
|
|
|
Lateral femoral epicondyle is associated w/ what syndrome?
|
IT band friction syndrome
|
|
|
List structures for anterior knee anatomy:
|
Femur- medial and lateral condyles
Tibia Patella Fibula |
|
|
List structures for lateral knee anatomy:
|
Lateral epicondyle
Lateral condyle Tibial plateau Gerdy's tubercle (lateral tubercle of tibia) Tibial tuberosity Apex of fibular head (styloid process) Fibular head |
|
|
List structures for medial knee anatomy:
|
Femur: adductor tubercle, distal end of adductor magnus tendon, uppermost part of MCL, medial epicondyle.
Tibia: medial condyle and tibial plateau |
|
|
Intercondylar fossa:
|
Separates the medial and lateral femoral condyles and medial and lateral tibial plateaus posteriorly.
Within the capsule. Not part of articular surface so not covered by articular cartilage. Popliteal surface. |
|
|
Tibiofibular joint-
|
Fibula attached proximally to tibia by ligaments and along its length by interosseus membrane.
Fixed joint. Head of fibula moves with ankle motion. Tib/fib joint plus ligaments of talus, calcaneus, and tibia allow little motion between tib and fib. |
|
|
ACL function:
|
Primary restraint to anterior tibial translation and contributes the most at 30 degrees of flexion.
Prevents hyperextension Secondary restraint to internal tibial translation. Resists ab/adduction at full extension Guides screw home rotation as it approaches terminal extension. |
|
|
Bundles of ACL:
|
Anteromedial bundle- taut in flexion
Posterolateral bundle- taut in extension. Increases knee stability. Likelihood of partial tears in these positions. |
|
|
PCL:
|
Primary restraint to posterior tibial rotation.
Secondary restraint to external tibial rotation at 90 degrees of flexion, decreasing w/ extension. Doesn't fan out; fibers parallel to bone. |
|
|
MCL primary role:
|
Primary restraint to abduction (valgus) and internal tibial rotation.
Superficial-MCL; deep- medial capsular ligament. |
|
|
What's commonly injured along w/ ACL?
|
MCL
|
|
|
What type of motion commonly injures the ACL?
|
hyperextension or internal rotation injury
|
|
|
Secondary role of MCL:
|
Provides anterior stability, which is enhanced by external tibial rotation.
In ACL deficient knees, MCL provides most of the anterior stability. |
|
|
LCL:
|
Primary restraint to adduction (varus) of knee.
Secondary restraint to anterior and posterior tibial displacements when drawer displacements are large. Combined with other lateral structures, is a significant restraint to external tibial rotation. |
|
|
Secondary static stabilizers: anterior-medial:
|
MCL
|
|
|
Secondary static stabilizers- posteriormedial:
|
Posterior oblique ligament
Semimembranosis fascia |
|
|
Secondary static stabilizers- anterolateral:
|
IT band
|
|
|
Secondary static stabilizers- posterolateral:
|
LCL
Popliteus tendon Popliteus arcuate complex |
|
|
Dynamic stabilizer-
|
Any muscle or tendon that crosses the joint. Kick in when start to see failure of static stabilizers.
|
|
|
Dynamic stabilizers of the knee:
|
Pes anserine muscles
Semimembranosis Gastroc Biceps femoris IT band Patellar tendon |
|
|
Medial knee stabilizers (primary and secondary)
|
MCL
Posterior oblique ligament PM capsule ACL PCL medial patellar retinaculum Semimembranosis Pes anserine Medial gastroc |
|
|
Lateral knee stabilizers (primary and secondary)
|
LCL
PL capsule Popliteus Arcuate ligament complex ACL PCL Lateral gastroc Biceps femoris |
|
|
Anterior knee stabilizers
|
ACL
PM/PL capsule MCL IT band Posterior oblique ligament Arcuate ligament complex |
|
|
Posterior knee stabilizers
|
PCL
ACL Posterior oblique ligament Arcuate ligament complex |
|
|
Differentiate between shapes of medial and lateral menisci
|
Medial- larger and C shaped
Lateral- smaller and O shaped |
|
|
2 Primary functions of menisci
|
Load bearing and stability
|
|
|
Secondary functions of menisci:
|
Joint lubrication
Prevent capsule, synovial impingement Shock absorber |
|
|
3 zones of menisci:
|
red-red: outermost
red-white white-white: innermost |
|
|
Meniscofemoral ligaments:
|
Anterior- ligament of Humphrey
Posterior- ligament of Wrisberg |
|
|
Coronary ligaments
|
Meniscotibial
Circle the outside of tibial plateau and hold menisci in place. Medial meniscus is most immobile, which is why its injured more. |
|
|
Baker's cyst:
|
Herniation of posterior medial joint capsule through the semimembranosis capsule. Check for involvement of posterior medial meniscus.
|
|
|
Other meniscal ligament:
|
Transverse ligament (anterior side) connects medial and lateral menisci.
|
|
|
Purpose of meniscofemoral ligaments
|
Increase stability of the knee joint by moving the lateral meniscus slightly medially and anteriorly when knee is in flexion.
|
|
|
Which meniscus has a firm bond to collateral ligament?
|
Medial meniscus has a firm bond to MCL
Lateral meniscus has no attachment to LCL |
|
|
What attaches to the posterolateral corner of the lateral meniscus?
|
popliteus tendon
|
|
|
What attaches to the posterolateral corner of the medial meniscus?
|
Semimembranosus fascia
|
|
|
In extension, menisci move ___. In flexion, they move ___ and tend to ___.
|
Anteriorly; posteriorly; narrow b/c articular surface becomes smaller.
|
|
|
Transitory pain
|
pain that moves with the meniscus
|
|
|
Anterior knee musculature
|
Vastus medialis, lateralis, and intermedius
Rectus femoris |
|
|
Origin, insertion, innervation of rectus femoris
|
O: AIIS
I: tibial tuberosity via infrapatellar tendon N: femoral |
|
|
Vasti O, I, N
|
O: lateralis- greater trochanter, upper 1/2 of linea aspera; intermedius: anterolateral upper 2/3 of femur, lower 1⁄2 of linea aspera; med: distal intertrochanteric line, medial linea aspera
I: tibial tubercle N: femoral |
|
|
Posterior knee musculature
|
Biceps femoris
Semimembranosis Semitendinosis Popliteus Gastroc |
|
|
Biceps femoris O,I,N
|
O: long- ischial tuberosity; short- lateral linea aspera, upper 2/3 of supracondylar line
I: fibular head, lateral tibial plateau N: Long- tibial; Short- common peroneal. May see injuries due to timing being off b/c of differing innervations. |
|
|
Semimembranosis OIN
|
O: ischial tuberosity
I: posteromedial border of the medial tibial plateau N: tibial |
|
|
Semitendinosis OIN
|
O: ischial tub
I: pes anserine N: tibial |
|
|
Popliteus OIN
|
O: lateral femoral condyle (under the LCL)
I: Posteromedial tibial N: tibial |
|
|
Pes anserine muscles:
|
Semitendinosis
Gracilis Sartorius |
|
|
Lateral knee pain due to popliteus needs to be differentiated from pain due to:
|
LCL
|
|
|
Gracilis OIN
|
O: Pubic symphasis and inferior pubic ramus
I: pes anserine N: Obturator |
|
|
Sartorius OIN
|
O: ASIS
I: pes anserine N: femoral |
|
|
IT/TFL OIN
|
O: ASIS
I: anterolateral tibia at Gerdy's tubercle N: superior gluteal |
|
|
Gastroc OIN
|
O: posterior condyles of femur
I: calcaneus via achilles N: tibial |
|
|
Borders of popliteal fossa
|
Superomedia: semimembranosis
Superolateral- biceps femoris Inferomedial- medial head of gastroc Inforolateral- lateral head of gastroc |
|
|
Contents of popliteal fossa:
|
Popliteal A and V; tibial and common peroneal NN
|
|
|
Patella-
|
A sesamoid bone imbedded in the quads and patellar tendon.
Serves similar to a pulley for improving angle of pull (results in greater mechanical advantage in knee extension) |
|
|
Femoral trochlea
|
primarily responsible for the stability of the patella in its groove from 30 degrees of flexion to full flexion.
The lateral trochlear facet provides a buttress to lateral patellar subluxation and helps maintain the patella centered in the trochlea. |
|
|
7 patellar facets
|
R and L superior, middle and inferior, and odd medial facet
|
|
|
Degrees of flexion are correlated w/ areas of articulation on the patella. Superior= __ degrees, middle= __ degrees, inferior = __ degrees, odd medial facet= __ degrees
|
90; 45; 20; 135
|
|
|
Knee pain w/ full knee flexion, there's a pathology of what facet?
|
Odd medial
|
|
|
What's the sunrise view?
|
Looking down on the inferior surface of the patella.
|
|
|
Trochlear dysplasia
|
Trochlear Dysplasia : There is substantial variability in trochlear depth with "trochlear dysplasia". This changes the ability to stabilize the patella.
|
|
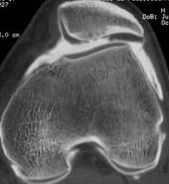
What is shown in this radiograph?
|
Trochlear dysplasia
|
|
|
How many patellar shape types are there?
|
4
|
|
|
Passive soft tissue restraints
|
Medial soft tissue stabilizers:
Layer 1:Superficial medial retinaculum, Medial patellotibial ligament Layer 2: Medial patellofemoral ligament, Superficial medial collateral ligament Layer 3: Medial patellar meniscal ligament |
|
|
Active soft tissue restraints
|
VMO
Lateral retinaculum- VL and ITB |
|
|
Forces of the quad tendon along with forces of the patellar tendon cause what?
|
Patellar compression
|
|
|
PFJ reaction forces with: walking, stairs, squatting, and running:
|
walking-= .5x weight
stairs= 3-4 x weight Squatting= 7-8 x weight running= 8 x weight |
|
|
Neurovascular anatomy of the knee includes:
|
Femoral A, popliteal A, genicular AA, popliteal V.
Tibial and sural N; common, superficial, and deep peroneal NN; saphenous N |
|
|
How many degrees of freedom at knee?
|
6- 3 translations, 3 rotations
|
|
|
Knee translations:
|
AP, compression/distraction, mediolateral
|
|
|
Knee rotations:
|
flex/ext
varus/valgus IR/ER |
|
|
Arthrokinematics of OC knee extension
|
Tibia glides anteriorly on femur and rotates externally (screw home)
|
|
|
Arthrokinematics of CC knee extension
|
Femur glides posteriorly on tibia and internally rotates (screw home)
|
|
|
Arthrokinematics of OC knee flexion
|
Tibia glides posteriorly on femur and IRs (reverse screw home)
|
|
|
Arthrokinematics of CC knee flexion
|
Femur glides anterior on tibia and ERs
|
|
|
Tibial glide is produced by what type of forces?
|
ligamentous
|
|
|
Ligamentous effects on arthrokinematics during knee flexion
|
tibia rolls posteriorly, elongating ACL.
ACL pulls on tibia causing it to glide posteriorly. |
|
|
Ligamentous effects on arthrokinematics during knee extension
|
tibia rolls anteriorly, elongating PCL.
PCL pulls on tibia causing it to glide anteriorly. |
|
|
Three forces that drive the screw home mechanism:
|
1. The shape of the medial femoral condyle
2. The passive tension in the anterior cruciate ligament 3. Lateral pull of the quadriceps muscle |
|
|
MOI of MCL
|
Valgus force with
foot fixed (often blow from lat side) Valgus, ext. tibial rotation force (skiing) |
|
|
MOI of LCL
|
Varus force with foot fixed
|
|
|
collateral ligament injuries S&S
|
Pain along course of ligament
Variable joint line laxity Minimal to moderate swelling Positive stress test at 0 and 30 |
|
|
Sprain grades
|
1- less than 5
2- 5-99 3- complete disruption |
|
|
Why do you test collateral ligaments at 30 and 0??
|
flex to 30 first to relax secondary, dynamic stabilizers so you're testing the ligaments. If positive at 30 and 0, more severe injury.
|
|
|
ACL: intracapsular, extracapsular, intra articular or extraarticular?
|
Intra articular, but extracapsular
|
|
|
ACL MOI
|
Hyperextension
Plant and cut to same/opp side Force to posterior tibia with knee flexed Rapid deceleration |
|
|
ACL S&S
|
Pop
Usually not associated with external trauma Rapid effusion- hemarthrosis Anterior joint line laxity: + Lachman, +/- anterior drawer, +/- pivot shift |
|
|
PCL MOI
|
Anterior force with knee flexed- fall w/ ankle dorsiflexed
Hyperflexion Severe hyperextension |
|
|
S&S of PCL injury
|
Vague knee pain
Posterior joint line laxity? Variable swelling Positive posterior drawer test Posterior rotatory instability Tibial sag sign Difficult to diagnose |
|
|
Rotatory instability:
|
Defined by the ligamentous complex involved allowing tibial subluxation
|
|
|
Anterolateral instability:
|
Structures on anterolateral side are compromised so tib comes forward and tibial plateau becomes more prominent on lateral side.
Tibia comes forward and medially rotates. Pivot shift injury/test. |
|
|
Anteriormedial instability:
|
anterior medial structues involved, medial tibial plateau most prominent b/c tibia laterally rotates. Tibia comes forward and laterally rotates
|
|
|
Posterolateral instability:
|
tibia moves backward and rotates laterally to make lateral tibial plateau most prominent
|
|
|
Posteromedial instability:
|
tibia moves backward and rotates medially to make medial tibial plateau most prominent
|
|
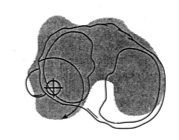
What type of instability?
|
Posteromedial instability
|
|
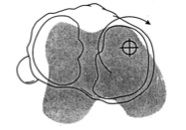
Type of instability
|
Anterolateral
|
|
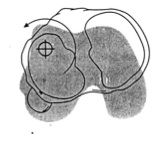
Type of instability
|
Anteromedial
|
|
Type of instabiltiy
|
Posterolateral
|
|
|
Anteromedial rotatory stabilizers
|
MCl
Medial capsular ligament Posterior oblique ligament PM capsule ACL |
|
|
Anterolateral stabilizers
|
ACL
PL capsule Arcuate ligament complex LCL ITB |
|
|
Posteromedial stabilizers
|
PCL
MCL Posterior oblique ligament Medial capsular ligament Semimembranosis Posteromedial capsule ACL |
|
|
Posterolateral stabilizers
|
PCL
Arcuate ligament complex LCL Biceps femoris PL capsule ACL |
|
|
Majority of strains involve:
|
mm that cross 2 joints
|
|
|
Hip flexor strain
|
Most commonly rectus femoris
|
|
|
2 common mechanisms of strains:
|
maximum contraction before the muscle is ready (concentric)
force generated exceeds the muscle's ability to withstand such a force (eccentric) |
|
|
S&S of rectus muscle strain
|
pain with resisted knee extension and passive stretch.
Swelling Location Defect |
|
|
Patellar/ quadriceps tendonitis (jumpers knee)
|
Microtrauma- repetitive eccentric loading
|
|
|
S&S patellar/quad tendonitis
|
Pain with deceleration
Quadriceps weakness Palpable tenderness History is key- when is pain most severe? Generally worse during eccentric loading like going down stairs. |
|
|
Patellar tendon rupture MOI
|
Usually a deceleration force
Landing off balance from jump Stepping in a hole Previous tendon pathology |
|
|
Patellar tendon rupture S&S
|
Inability to extend
knee Significant swelling Pain High riding patella R/O patellar dislocation If quads tendon, quads will ball up |
|
|
Patellar s/l or d/l MOI
|
Usually non-‐contact
Cutting maneuver- Valgus stress with strong quadriceps contraction Anatomical predisposition- incrreased Q angle and bony anomalies Recurvatum/hyperextension increases instability |
|
|
S&S of patellar s/l or d/l
|
Sensation of knee going out
Intense pain with effusion Inability to actively flex knee Laterally displaced patella Significant soft tissue damage Positive patellar apprehension |
|
|
R/O w/ patellar s/l or d/l
|
Osteochondral fracture and knee d/l
|
|
|
MOI hamstring strain
|
Sudden maximal contraction- jumpers push leg out of box or jumpers plant leg.
rapid eccentric contraction to decelerate limb- sprinter in full stride |
|
|
Most commonly strained hamstring: why?
|
Short head of biceps femoris due to dual innervation of biceps and timing problems w/ long head of biceps or quads- co-contraction producing hamstring strain
|
|
|
S&S hamstring strain
|
Location important - rule of thumb -> the higher the strain, the longer the rehab
Pain with resisted knee flex and passive stretch Palpable tenderness Pos/neg defect |
|
|
MOI meniscal injuries
|
Plant and cut to
opposite side (medial) Rapid extension with foot fixed (medial)- restricts screw home. Weight bearing with hyperflexion (lateral) Injuries related to ACL or MCL |
|
|
MOI secondary meniscal injuries
|
valgus/varus
hyperextension/flexion IR/ER |
|
|
S&S of meniscal injuries
|
Sudden locking
Localized joint line pain End-feel? Mild/mod effusion Transitory pain Pain on hyperflexion + McMurrays |
|
|
Discoid meniscus
|
not a crescent shape, more pancake shaped- It's an anatomical variant of the meniscus, so meniscal tissue covers entire articular surface and femoral condyles can't articulate with tibial plateau. The meniscus isn't good at shock absorption and these people are at a high risk for tears.
|
|
|
Baker's cyst- kids
|
Children - constantly swollen bursa in relationship to the semimembranosus tendon.
Usually presents as a central popliteal fossa mass. Appear spontaneously, and typically persist for 1 or 2 years before spontaneous resolution. |
|
|
Baker's cyst- adults
|
Herniation of posterior joint capsule through defect in the semimembranosis capsule
Associated w/ medial meniscal tear |
|
|
Salter-Harris classification type I
|
Complete physeal fx w/ or w/o displacement. in child can disrupt growth of the bone and may lead to leg length discrepancy.
|
|
|
Salter Harris type II
|
Physeal fx that extends through the metaphysis, producing a chip fx of the metaphysis that may be very small
|
|
|
Salter Harris type III
|
Physeal fx that extends through the epiphysis
|
|
|
Salter Harris Type IV
|
Physeal fx plus epiphyseal and metaphyseal fx
|
|
|
Salter Harris type V
|
Compression fx of growth plate.
|
|

Salter harris type...
|
2
|
|

Salter harris type
|
4
|
|

Salter harris type
|
1
|
|
|
salter harris type
|
5
|
|

Salter harris type
|
5
|
|

slater harris type
|
3
|
|
|
More common for kids to tear a ligament or fx the epiphyseal plate?
|
fx
|
|

What's this?
|
Avulstion fx of the lateral tibial condyle- Segond fx
|
|
|
Segond fx
|
Occurs with severe rotary stress and concurrent ACL disruption.
Also associated w/ PCL rupture. |
|
|
Tibial tubercle fx
|
Occur far more commonly in children than adolescents.
The Ogden and Murphy classification system divides fractures into three categories. |
|
|
The Ogden and Murphy classification system divides fractures into three categories:
|
Group 1 -fractures are minor, distal and undisplaced.
Group 2 -fracture separation of the whole tuberosity with displacement of the fractured segment. Group 3 -proximal fractures with major displacement, and comminution involving the upper tibial region. |
|
|
Displaced tibial tuberosity fx are best managed how?
|
internal fixation
|
|
|
fibula fx
|
Occur following direct blow. These fractures heal well and rapidly.
|
|
|
Upper fibular fracture
|
Upper fibular fractures (at the neck and upper shaft) may occur with severe rotary ankle injuries, where the tibial malleolus is fractured and the fibula fractures as part of this rotary fracture-dislocation of the ankle (Dupuytren fracture).
|
|
|
The upper fibula, and especially the neck fractures, may be associated with
|
peroneal N palsy. Neuropraxia with a foot drop. Variable recovery time.
|
|
|
Styloid process fib fx
|
Direct blow or avulsion.
Biceps femoris tendon LCL |
|
|
Types of patellar fx
|
stellate
Transverse Lower pole Vertical |
|
|
Stellate fx
|
multi- fragmented fracture usually the result of falling onto a flexed knee
|
|
|
Transverse fx
|
occurs when the patella receives a relatively minor blow while the quadriceps is strongly contracting causing a transverse break separating the superior and inferior fragments.
|
|
|
Lower pole fx
|
Lower pole fx
|
|
|
Vertical fx
|
usually occurs from an indirect blow (kick) to patella
|
|
|
Osteochondral fracture and osteochondritis dissecans MOI
|
Internal vs external trauma? location dependent.
Plant and cut to opposite side- Internal trauma. intercondylar eminence impacts posterolateral corner of medial femoral condyle. Direct blow- external trauma. Fall with knee flexed. Injury to weight-‐ bearing surface of femoral condyle |
|
|
Osteochodritis dessicans
|
Osteochondral fx can alter blood supply to fx fragment, and part dies. Will eventually sleugh off and float around in joint space.
Loose body in joint; joint mouse. |
|
|
Osteochondral fracture S&S
|
Localized tenderness
Pain esp w/ WB Swelling/hemarthrosis Positive Wilson's test if fracture is in intercondylar notch |
|
|
Osteochodritis dessicans S&S
|
Mild/mod effusion
Episodes of locking Endfeel |
|
|
OA
|
A chronic joint disorder in which there is progressive softening and disintegration of articular cartilage accompanied by new growth of cartilage and bone at the joint margins (osteophytes) and capsular fibrosis
|
|
|
Varus gaps the joint on the ___ side, stessess the ___.
|
lateral; medial
|
|
|
OA classification
|
Primary or idiopathic
Secondary: infection, dysplasia, SCFE, avascular necrosis, Perthes, trauma |
|
|
OA mechanism 1- disparity between:
|
Stress applied to articular cartilage and strength of articular cartilage.
|
|
|
OA mechanism 2- increased stress:
|
increased load- BW or activity
Decreased area- varus knee |
|
|
OA mechanism 3- weak cartilage
|
Age
Stiff-ochronosis Soft- inflammation Abnormal bony support- AVN |
|
|
OA x-ray changes
|
Joint space narrowing
Subchondral sclerosis Osteophytes Cysts |
|
|
Arthritis sx
|
Pain
Swelling Stiffness Instability Deformity Loss of function |
|
|
Chronic anterior knee pain MOI
|
New activity
Incomplete rehab- weakness of VMO Hamstring tightness Extensor mechanism restriction Abnormal biomechanics Structural abnormalities |
|
|
Chronic ant knee pain predisposing factors
|
VMO atrophy
Q angle? Patella alta Hamstring tightness Excessive subtalar pronation Femoral anteversion/torsion Weak glut med |
|
|
S&S of chronic ant knee pain
|
Diffuse pain, incr. with resisted extension.
Knee stiffness (+ movie house sign) Variable swelling +/- Clarke's sign |
|
|
Chondromalacia patellae
|
wearing away of patellar articular cartilage
|
|
|
Synovial plica
|
Thickening of synovial membrane
|
|
|
Synovial plica MOI
|
Overuse
Direct trauma Biomechanical abnormalities |
|
|
S&S of synovial plica
|
Anterior knee pain
Tenderness over medial femoral condyle Clicking, popping, pseudo locking, focal swelling Hughston plica test + R/O medial meniscal injury |
|
|
IT band friction syndrome MOI
|
Overuse
Tightness of TFL/ITB Running on uneven surfaces- crown of road Faulty biomechanics |
|
|
S&S of ITB friction syndrome
|
Pain over lateral femoral epicondyle
Crepitus Localized swelling + Obers and Noble compression tests |
|
|
Osgood-Schlatter's disease
|
Apophysitis of the tibial tuberosity.
Partial avulsion of patellar tendon off of insertion. Will see enlarged tibial tubercle. |
|
|
Who's most commonly affected by Osgood-Schlatter's?
|
Young active children are most commonly affected.
Usually runners, basketball players, and jumpers. More common in males than females. |
|
|
Causes of Osgood-Schlatter's
|
Sudden increase in bone length and soft tissue isn't given enough time to adapt.
Idiopathic, familial. |
|
|
Osgood-Schlatter time of onset
|
Usually presents in the pre-‐teen years up through adolescence.
This is because the bone, muscle, and tendon are still developing. The stress from forceful contractions of the quadriceps group causes additional stress on the Tibial Tuberosity causing more calcification. |
|
|
Other injuries from Osgood-schlatter's
|
Patellar tendonitis
Patellofemoral stress syndrome Quad tendon avulsion Pes anserine bursitis Chondromalacia patellae Osteomyelitis of proximal tibia Patellar tendonitis Sinding-Larsen-Johansson syndrome |
|
|
Sinding-Larsen-Johansson syndrome
|
same as osgood-schaltter, except it occurs at the inferior pole of patella.
|
|
|
Osgood-Schlatter inspection
|
Large bump over Tibial Tuberosity
X-‐Rays usually needed to determine how much damage has been done. Usually no difference in gait unless the patient is seen when condition is acute May be swelling over the Tibial Tuberosity. Crepitus over tib tuberosity and patellar tendon |
|
|
S&S of Osgood-Schlatter
|
Sweling over tibial tuberosity
Tenderness of tuberosity during exercise Pain when contraction of the quadriceps against resistance or when contracting the muscles with the leg straight. Quad weakness: pain related early; atrophy late |
|
|
Physical exam for knee: observation
|
Gait
Assymetry (bony or soft tissue) Signs of inflammation Willingness/ability to move part |
|
|
Physical exam for knee: biomechanical exam:
|
Posture/alignment: physiological valgus, tibial varus/torsion, patellar position
Q angle Related joints: hip, foot/ankle/subtalar |
|
|
Physical exam for knee: leg alignment
|
Genu valgum, varum, or recurvatum
Patellar malalignment Leg length discrepency |
|
|
Physical exam for knee: palpation:
|
TTP
Joint effusion vs swelling- circumferential measurements Muscular atrophy Soft tissue restriction |
|
|
Observation: internal femoral rotation; Implication:
|
femoral anteversion or soft tissue adaptation
|
|
|
Observation: internal femoral rotation w/ squinting patella; Implication:
|
femoral anteversion or soft tissue adaptation
|
|
|
Observation: internal femoral rotation w/o squinting patella; Implication:
|
femoral anteversion or soft tissue adaptation w/ tight lateral structures
|
|
|
Observation: high riding patella; implication:
|
Patella alta
|
|
|
Observation: VMO assymetry
|
May be weakness
|
|
|
Observation: enlarged/puffy fat pad
|
Possible fat pad impingement
|
|
|
Observation: anterior/posterior pelvic tilt/swayback Implication:
|
lumbopelvic mechanics
|
|
|
Observation: knee hyperextension; Implication:
|
enlarged fat pad; possible impingement; skeletal laxity
|
|
|
Observation: uneven PSIS level:
|
possible leg length discrepancy
|
|
|
Observation: achilles tendon swelling; Implication:
|
acute vs chronic tendinosis
|
|
|
Differential diagnosis by LOCATION: anterior:
|
Patellofemoral syndrome, bursitis, Osgood-Schlatter's disease, patellar tendonitis, patellar fx
|
|
|
Differential diagnosis by LOCATION: Medial
|
meniscus, MCL, DJD, pes anserine bursitis
|
|
|
Differential diagnosis by LOCATION: lateral
|
Meniscus, LCL, DJD, ITB friction syndrome, fibular head dysfunction
|
|
|
Differential diagnosis by LOCATION: posterior
|
Hamstring injury, tear of posterior horn of menisci, Baker's cyst, neurovascular injury
|
|
|
MOI purpose:
|
helps predict structure and direct rehab
|
|
|
Chronic injury
|
Precipitating factors overuse, previous injury, structural/biomechanical changes.
Clicking, grinding, popping sxs. Knee locked, buckled, or given way. Pain-‐related activities |
|
|
Acute injury
|
Contact or non-contact?
|
|
|
Contact injuries/direct blows commonly cause injury to:
|
Commonly cause injury to: collateral ligaments, patellar dislocation, epiphyseal fractures in children with open growth plates
Valgus forces are more common than varus-‐ directed forces. |
|
|
Swelling w/in 24 hours of injury may indicate:
|
Hemarthrosis associated with ligament, meniscal, or osteochondral injury.
Intra-articular injury |
|
|
Swelling post-24 hours of injury
|
Reactive synovitis associated with trauma or overuse condition.
More likely extraarticular |
|

What is this view called?
|
sunrise or skyline view
|
|

What is this?
|
Fibella- small sesamoid bone
|
|
|
Ottawa Knee rules
|
1. Age 55 or older
2. Point tenderness at patella 3. Tenderness over head of fibula 4. Cannot flex knee to 90 5. Cannot bear weight for 4 steps immediately and at the emergency department/office. Presence of one indicates fx |
|
|
Vulnerable structures in non contact injuries:
|
Cruciate ligaments (most common)
Menisci Joint capsule **Think ACL INJURY any time you have a patient with a significant NON-‐CONTACT injury with foot planed on the ground |
|
|
Pop felt or heard, most likely:
|
ligament or meniscus injury
|
|
|
Immediate effusion (intraarticular)
|
Refers to less than 6 hours following an injury.
Correlates to: cruciate ligament tear, articular fx, knee d/l |
|
|
Delayed effusion (intra-articular)
|
Usually follows meniscal injury.
50% of patients with an acute ligament rupture will experience localized edema at injury site, |
|
|
In instances where swelling is less than expected:
|
Chronicity
Complete ligamentous or capsular disruption Fluid exudes through the tear "Extra-articular" swelling |
|
|
Noncontact injury w/ a pop
|
ACL tear
|
|
|
Contact injury w/ a pop
|
MCL/LCL tear, meniscal tear, fracture
|
|
|
Acute swelling
|
ACL tear, PCL tear, fracture, knee dislocation, patellar dislocation
|
|
|
Lateral blow to knee
|
MCL tear
|
|
|
Medial blow to knee
|
LCL tear
|
|
|
Knee gave out or buckled
|
ACL tear, patellar d/l
|
|
|
Fall onto flexed knee
|
PCL tear
|
|
|
Knee probs not to be missed:
|
Septic arthritis
Osteomylitis Referred pain- pain esp in young boys, rule out SCFE DVT Compartment syndrome |
|
|
Assessment of patellar position: glide
|
Midpole of patella is equidistant to medial and lateral femoral epicondyles.
|
|
|
Lateral glide (static)
|
Abnormal static alignment of patella: Midpole of patella sits closer to lateral femoral epicondyle= lateral glide.
|
|
|
Glide: abnormal dynamic alignment
|
Patella moves laterally w/ quad contraction
|
|
|
mplication of abnormal glide:
|
decreased VMO tension
|
|
|
Mediolateral patellar tilt
|
medial and lateral patellar borders equal height, and posterior edge of both borders can be palpated
|
|
|
Lateral tilt:
|
Abnormal static alignment; Medial border higher than lateral; posterior
edge of lateral border difficult to palpate. |
|
|
Abnormal dynamic alignment of lateral tilt:
|
Medial border displacement from increased lateral tilt.
|
|
|
Lateral tilt implication:
|
tight lateral retinacular structures
|
|
|
AP tilt:
|
superior and inferior borders are the same height
|
|
|
Posterior tilt:
|
Abnormal static alignment; Inferior border displaced posteriorly; may be imbedded in fat pad.
|
|
|
Posterior tilt and abnormal dynamic alignment:
|
Quad contraction leads to increased posterior tilt, esp w/ knee hyperextension.
|
|
|
Posterior tilt implication:
|
Fat pad irritation leads to inferior patellar pain, esp w/ knee extension
|
|
|
Patellar rotation
|
Long axis of patella in parallel w/ long axis of femur.
|
|
|
Patellar ER
|
Abnormal static and dynamic alignment.
Inferior pole sits lateral to the long axis of the femur. |
|
|
Implication of patellar ER
|
Implication: tight retinacular structures
|
|
|
Ligament sprain grades
|
I- pain
II- mild- moderate laxity III- significant laxity w/ no ligamentous end feel |
|
|
Valgus stress at 0 degrees tests what structures?
|
MCL (superficial and deep), posterior oblique ligament, posterior medial capsule, ACL/PCL
|
|
|
Valgus stress at 30 degrees tests what structures?
|
MCL (superficial), posterior oblique ligament, PCL, posterior medial capsule
|
|
|
Varus stress at 0 degrees tests what structures?
|
LCL
Posterior lateral capsule Arcuate complex PCL/ACL |
|
|
Varus stress at 30 degrees tests what structures?
|
LCL
Posterior lateral capsule Arcuate complex |
|
|
Anterior drawer test isn't as reliable b/c:
|
ITB runs parallel w ACL in this position. False negatives.
|
|
|
When may Lachman's test have a false negative?
|
If tibia is IR or the femur isn't properly stabilized.
|
|
|
positive anterior drawer test indicates:
|
ACL (anteromedial bundle)
Posterior lateral capsule Posterior medial capsule MCL (deep fibers) ITB Arcuate complex |
|
|
False negatives on anterior drawer:
|
If only the ACL is torn or if there's swelling or hamstring spasm.
|
|
|
False positive on anterior drawer:
|
If there's a posterior tibial tag sign present
|
|
|
When the Tibia Externally Rotates what happens to the ligaments?
|
The collaterals become taut and cruciates relax.
|
|
|
When the Tibia Internally Rotates what happens to the ligaments?
|
The cruciates become taut and collaterals relax.
|
|
|
ER Recurvatum test:
|
Tests for posterolateral rotatory instability.
Positive test: increased hyperextension and ER of tibia. Positive test indicates: PCL, LCL, posterolateral capsule, arcuate complex. |
|
|
Hughston posteromedial drawer test:
|
Tests for posteromedial rotatory instability.
Positive test: posterior tibial displacement, especially of the medial tibial condyle Positive test indicates: PCL, MCL, posteromedial capsule, posterior oblique ligament |
|
|
Hughston posterolateral drawer test:
|
Tests for posterolaterall rotatory isntability.
Positive test: posterior tibial displacement, esp of lateral tibial condyle Positive test indicates: PCL, LCL, posterolateral capsule, arcuate complex |
|
|
Slocum's test for rotatory instabiity: drawer test for ALRI
|
Drawer position w/ tibia short of full IR.
Positive test: Anterior tibial displacement esp of the lateral tibial condyle. Positive test indicates: ACL, posterior lateral capsule, arcuate complex, LCL and PCL |
|
|
Slocum's drawer test for AMRI
|
Drawer position w/ tib short of full ER
Positive test: anterior tibial translation esp of the medial tibial condyle. Positive test indicates: MCL (superficial), posterior oblique, posterior medial capsule, ACL |
|
|
Lateral pivot shift test
|
Tests for ACL and posterolateral rotary instability (ALRI). Posterolateral capsule and arcuate complex.
Positive test: test is the tibia reduces on the femur at 30 to 40 degrees of flexion, subluxation of the tibia on extension |
|
|
tibial sag sign AKA
|
Godfrey sign/test
|
|
|
Positive drawer test indicates
|
PCL
Arcuate complex Possibly ACL? |
|
|
Meniscal tests:
|
McMurray's
Apley's compression Joint line pain Thessaly's test |
|
|
Apley's distraction test:
|
Generic test for ligamentous lesions.
Positive test is pain that's increased (ligamentous) w/ distraction of knee. |
|
|
Thessaly test
|
Done w/ patient standing, 1st on normal leg.
Flex knee 5 degrees, rotate body on fixed leg back and forth 3 x, holding examiner's hands for stability. Flex further to 20 degrees and repeat. Repeat on affected leg. Positive is pain at joint line or feeling of locking or catching |
|
|
Objectives of knee rehab
|
Protect the joint with braces, crutches,etc.
Reduce inflammation and swelling. Maintain muscle responsiveness and prevent atrophy Restore range of motion (ROM) Free up adhesions Rebuild muscle strength Restore normal gait patterns Restore balance and proprioception Rebuild functional endurance Return to functional activities |
|
|
Initial management of acutely injured knee depends on:
|
Accurate diagnosis
Potential functional outcomes that are patient specific. Leads to a specific treatment plan. |
|
|
Key factors in rehab decisions following surgery:
|
Type of surgery performed
Strength of fixation Initial strength of graft Anticipated changes during revascularization of graft. Condition of secondary restraints. Condition of joint surface and menisci. Secondary procedures performed to supplement repair. |
|
|
Key factors in rehab decisions following surgery continued
|
Need and type of external supports
Post-op complications Age, occupation, activity level, and resources of patient Recreational/competitive sports goals Condition of related joints Change in tissue biomechanics Surgeon's specific concerns/guidelines |
|
|
Goal of Rehabilitation
|
Return the patient to previous level of function as quickly as possible while at the same time minimizing the risk of re-‐ injury.
|
|
|
Range of Motion deficit, possible PT treatment:
|
Joint Mobilization, Soft-‐Tissue Mobilization
|
|
|
Neuromuscular control deficit, possible PT treatment:
|
Proprioceptive Neuromuscular Facilitation
|
|
|
Postural stability deficit, possible PT treatment:
|
Core stability training
|
|
|
Muscular Strength, Endurance, and Power deficits, possible PT treatment:
|
Plyometrics, Open KC, Closed KC, Isokinetics, Aquatics
|
|
|
Knee rehab, 3 simple keys:
|
ROM- Needed to increase motion and return to function as quickly as prudent and possible
Strength- Needed to deter further problems or protect the area of injury from further injury Functionality- Needed to return the patient to normal daily activities within reason. |
|
|
What dictates stages of rehab?
|
phases of tissue healing
|
|
|
Acute phase goals
|
Immediate response phase
Minimize edema and restore functional range |
|
|
Subacute phase
|
Address strength and flexibility deficits
|
|
|
Chronic phase
|
Advanced functional rehab for preparation to return to activity
|
|
|
Acute phase
|
Catabolic response
Minimize inflammatory response: Control pain Reduce swelling Alleviate m spasm/inhibition Cool the part Minimize DVT (ankle pumps) Initiate quad reed (quad sets and neuromuscular e-stim) PROM, AROM |
|
|
PRICED
|
Protection
Rest (active) Ice Compression Elevation Drugs |
|
|
Protection
|
Minimize further injury w/ external support or gait assistive device.
|
|
|
Rest
|
Active rest
Treat the patient, not the pathology Decrease effects of disuse/immobiliztion. Earlier return to activities. |
|
|
Cryotherapy
|
Ice + exercise= cryokinetics
Early motion with controlled inflammatory response |
|
|
PROM exercises
|
Flexion exercises: wall hangs (assisting device is gravity), towel slides (assisting device is arms), stationary bike (assisting device is other leg)
Extension exercises: wall hangs |
|
|
Initial PT
|
The first few sessions of physical therapy may consist more of modalities and some manual techniques to address inflammation, pain and ROM: heat/ice
US E-STIM manual stretching Scar and patellar mobs PROM for full knee flexion and extension Retrograde massage to decrease swelling |
|
|
Subacute phase
|
Anabolic response
Tissue remodeling Graded stress: early motion, tissue mobility, strength, and flexibility Initiate knee and hip stretches: quads, hamstrings, gastroc, ITB, hip flexor, and piriformis Initiate hip and knee strengthening Initiate proprioceptive activities Kinesthetic rehab, CC exercise, OC exercise |
|
|
Initial goal of early subacute phase
|
Realign collagen along lines of stress.
Minimize scar tissue formation at the areas of the knee joint that restrict motion. |
|
|
Advantages of early protected mobilization
|
Decreased disuse effects
Retard capsular contracture Maintain nutrition of articular cartilage Allow early controlled forces on healing collagen tissue |
|
|
Reasons for soft tissue mob
|
Help prevent development of adhesions between the mm planes and other tissues.
Prevent adhesions of scar tissue to underlying soft tissue. |
|
|
Subacute phase: initiate hip and knee strengthening
|
SLR (4 planes)
Squat progressions Short arc quads Side stepping |
|
|
subacute phase: Initiate proprioception activities
|
Weight shifts
Single leg stance progressions |
|
|
Subacute phase kinesthetic rehab
|
to facilitate the limb's performance of a complicated skill without conscious guidance
|
|
|
Kinesthetic rehab progression parameters:
|
Sub-maximal to maximal effort
Slow to fast speeds in functional activity patterns Known to unknown patterns Variable limb positions Stable to unstable surfaces |
|
|
closed kinetic chain exercise
|
Multi-segmented, multi-joint exercise of the distal extremity.
Functional exercise- biomechanically and neuromuscularly Used in early rehab. More stable for the knee joint. |
|
|
CC exercise include:
|
Mini-squats
Wall slides Lunges Leg press Lateral step-ups TKE (terminal knee extension) w/ T-band At the knee- promote quad/hamstring co-contraction. Promote normal proprioceptive input to the joint. |
|
|
Sub-acute OC exercise
|
Single joint, single muscle exercise w/ distal extremity free to move.
Utilized to strengthen individual m or m group. Also used in early rehab. |
|
|
OC exercises include:
|
Hamstring curl machine
Leg extension machine |
|
|
OC Progression
|
Isometric
Isotonic- concentric, eccentric Isokinetic- concentric, eccentric |
|
|
Balance/proprioception
|
Balance can sometimes be compromised after an injury or surgery.
Exercises: single leg touches Single leg balance |
|
|
Chronic phase
|
return to function.
Activity-specific skills Power Speed Agility Functional rehab- dynamic functional stability |
|
|
Functional rehab:
|
Utilize the SAID principle (specific adaptation to imposed demands).
Analysis of imposed demands Understand the limitations of the athlete. |
|
|
Functional rehab program, types of exercises:
|
Single leg balance
Soft/unstable surfaces Eyes closed Plyometrics Functional acitities |
|
|
Plyometrics
|
Skills analysis
Warm-up and stretch Cool-down and relaxation "Advanced" rehab It's all about the LANDING- technique is crucial. |
|
|
Plyometrics- key concepts
|
Land softly and quietly
Use knees and hips as shock absorbers- keep flexed. Land on toes. Keep shoulders over knees. Keep knees over feet. Stick the landing |
|
|
Potential injuries associated w/ plyometric training:
|
Tendinitis- patellar and achilles
Heel pad bruising Chronic anterior leg pain PF pain Stress fx |
|
|
Return to functional activity:
|
When the patient can participate in activity specific exercises w/o pain or weakness.
Full ROM is apparent in injured knee. Collaborate decision between patient, PT, and physician |
|
|
Types of tape
|
linen and elastic
|
|
|
Properties of linen tape
|
Tensile strength.
Ability to resist elongation Mimics ligaments |
|
|
Uses of linen tape
|
Prevention of joint sprains
Support of injured ligament Restriction of motion |
|
|
Properties of elastic tape
|
Elasticity- deform and recover
Tensile strength Mimics muscle/tendon |
|
|
Uses of elastic tape
|
Assist/facilitate motion
Control swelling Restrict motion |
|
|
Uses of tape:
|
Hold on wound dressings
Secure compressive bandages Restrict/limit motion Assist motion Secure special pads/devices |
|
|
When is it not appropriate to tape?
|
Further assessment needed
Immediately following an acute injury to allow the athlete compete. Functional disability: limitation in movement patterns, strength, balance Acute swelling After cold application Pre-puberty b/c restrict joint and put stress on epiphyseal plates. Overnight Violation of sport rules Tape allergy/contact dermatitis If you're unsure |
|
|
Tape application
|
Select correct tape
Position part Overlap Ovoid continuous taping Keep tape roll in hand Smooth and mold Follow natural contours Anchor and lock |
|
|
Moleskin
|
increased tensile strength, used for maximal stability
|
|
|
Vulnerable feet
|
Mechanical stresses
Neuropathy- sensory, motor, autonomic dysfunction Disease- PVD, diabetes Wound care If they can't feel it, it's vulnerable |
|
|
Charcot foot-
|
destruction of supportive/ligamentous structures of the foot due to circulatory issues.
|
|
|
Charcot's arthropathy
|
Typically see patients after the destructive phase.
Rocker bottom deformity- like walking on navicular, no arch. |
|
|
Charcot's arthropathy treatment
|
Footwear, pressure reduction, orthotics.
Gait Wound care Bed rest Splints, padding Patient ed |
|
|
Causes of amputation
|
Vascular
Trauma- ankle fx Infection- often relates to vascular challenges Cancer Congenital |
|
|
Decision for surgical amputation: assessment
|
History- claudication
During exam: skin, hair, nails Pulses, positional tests (elevation, dependent) Vascular testing- collateralization of blocked main arteries. |
|
|
Most common levels of amputation
|
Toe
Ray Partial foot Ankle disarticulation Transtibial (BK) Transfemoral (AK) Hip |
|
|
Level of partial foot amputations
|
Boyd
Pirigoff Chopart Lisfranc Transmetatarsal |
|
|
Toes 2-5 amputations
|
Minimal balance loss
No treatment/insert Lose 2,3, or 4, the others will migrate over time. May use a shoe insert to prevent this. |
|
|
Great toe amputation
|
loss of pushoff and anterior lever arm.
Custom insert- steel shank/ carbon fiber |
|
|
Ray resection
|
Loss of balance and WB surface
Custom accomodative insert or shoes |
|
|
Metatarsal disarticulation
|
Loss of anterior lever arm and balance
Custom insert w/ carbon fiber and toe filler Important to work on ROM esp dorsiflexion |
|
|
Transmetatarsal amputation
|
Increased loss of lever arm and WB surface
Bony anterior section complicating prosthetic care. Custom insert w/ toe filler- steel shank or carbon |
|
|
Lisfranc amputation
|
Greater loss of balance and WB surface
Disruption of anterior compartment insertions causes tendency for equinus. Highest level of amputation to consider custom insert w/ toe filler. Recommend high top shoes May require slipper or boot type prosthesis. |
|
|
Chopart amputation
|
Almost total loss of anterior lever arm and WB surface.
Pronounced tendency for equinas. Only 2 bones left in foot (talus and calcaneus). Prosthesis that extends to patellar tendon. If ankle joint can achieve a neutral position w/ good motion, an AFO derivation prosthesis may be used. |
|
|
Boyd amputation
|
Only seen in kids.
Variation of Symes where calcaneus is transected and placed below tibia and fibula. Complete loss of foot function. Symes prosthesis- difficult due to leg length discrepancy. |
|
|
Pirogoff amputation
|
Similar to Boyd except calcaneus is transected vertically and rotated 180 degrees.
Results in no limb length discrepancy. Symes prosthesis- prosthetic care creates leg length discrepancy. |
|
|
Transtibial amputation levels
|
Proximally to distal- very short, short, standard, long
Syme |
|
|
Shorter lever arm=
|
more work for patient
|
|
|
Symes amputation
|
Ankle disarticulation
Complete loss of all foot function. Lose: shock absorption at heel contact and balance and all WB surfaces of the foot. Symes prosthesis. |
|
|
Standard transtibial amputation
|
Transverse amputation of the tibia and fibula.
Biomechanical loss same as Symes (no shock absorption). Distal WB considerations. Transtibial prosthesis |
|
|
Osteomyoplasty
|
Transtibial amputation w/ bone bridge.
Distal WB permitted. Transtibial prosthesis. |
|
|
Knee disarticulation
|
Through the knee joint amputation.
Allows distal WB. Displaces mechanical knee joint. Loss of all foot, ankle and knee function. Knee disarticulation prosthesis. Knee will be longer on this side b/c prosthetic knee joint. |
|
|
In knee disarticulation, what muscle belly is transected?
|
gracilis
|
|
|
Transcondylar/supracondylar amputation
|
Transverse amputation through or just above the condyles.
No distal WB. Preserves long lever arm. Transfemoral prosthesis. Not widely used. Adductors are maintained. Challenge- propensity for residual limb to be ER, ABD and flexed if adductors aren't present. |
|
|
Transfemoral amputation
|
Transverse amputation of femur.
Biomechanical loss same as knee disarticulation with shorter lever arm. Transfemoral prosthesis |
|
|
TKA line
|
trochanter, knee, ankle- determine if leg is set up as voluntary control or stable.
Stable- line lies slightly anterior to mechanical knee joint. This makes the patient work harder to initiate swing. |
|
|
Myoplasty
|
Suture muscles over distal femur.
|
|
|
Myodesis
|
Muscles sewn directly to distal femur. Drilled holes to put muscles in.
|
|
|
Goal in above knee amputations
|
Maintain the same adductor function. Over time these stretch out.
|
|
|
Hip disarticulation
|
Through hip joint amputation.
Loss of all lower extremity biomechanics. Hip disarticulation prosthesis. All levels through or above the greater trochanter including femoral neck are treated w/ a hip disarticulation prosthesis. Patient controls entire LE by pelvic tilt and lordosis. Primary transport is wheelchair. |
|
|
Hemipelvectomy
|
Amputation through a portion of pelvis.
Loss of WB surface for sitting. Hip disarticulation prosthesis w/ modified socket. Most patients will use a wheelchair. |
|
|
PFFD (proximal femoral focal displasia)
|
Symes amputation and knee fusion. Van Nes rotation-plasty (ankle rotates and becomes knee).
Complicated hip function w/ loss of knee and foot function. Transfemoral prosthesis w/ PFFD modifications |
|
|
Congenital deficiencies
|
Transverse and longitudinal
|
|
|
Transverse congenital deficiency
|
Limb developed normally to a certain level beyond which no skeletal elements exist.
|
|
|
Longitudinal congenital deficiency
|
Reduction or absence of an element of the long axis of the limb.
Ex: tib/fib anelias (absent); hemi- partially absent |
|
|
Hemicorporectomy
|
Amputation at the waist. Need a hoist, etc.
Usually due to cancer. |
|
|
Bilateral above the knee increases energy expenditure how much?
|
4x. Pre-prosthetic need to prepare body for increased work.
|
|
|
Complete transtibial prescription
|
Socket
Interface Suspension- how prosthetic is held on Foot Shank |
|
|
Pressure tolerant areas for WB
|
Patellar tendon
Pretibial muscles and lateral flat aspect of tibia Medial tibial flare Popliteal fossa Gastroc/soleus muscles |
|
|
Total surface bearing
|
Volume match between tissue and socket.
Weight distributed over entire surface. Total contact. |
|
|
Interface
|
Socks/hard sockets
Pelite liner Gen liners |
|
|
Suspension
|
Sleeve
Cuff strap Supracondylar (grabs above adductor tubercle) Locking pin Waist belt Vacuum assisted Joints and corset |
|
|
Vacuum assisted suspension
|
12-15 in. Hg or higher
Volume control Increased proprioception, better linkage. Reduced moisture build-up |
|
|
Types of prosthetic feet
|
SACH
Single/multi axis Flexible keel (SAFE) Dynamic response Dynamic response w/ articulated ankle (inv,ev, PF,DF) Other Hybrid- blending of categories |
|
|
Dynamic response foot
|
Integrated dynamic response shank/pylon
High density plastic or carbon fiber keel (works in only one direction) The longer it is, the more energy it can store and return. |
|
|
Additional foot features
|
Heel height adjustability
Ankle Shock and rotation Specialty components ex: swim ankle |
|
|
Shanks
|
Endoskeletal: interchangeability, post fab. adjustment, strong, lightweight.
|
|
|
Exoskeletal
|
Durable
No adjustments No weight limit |
|
|
Post-op management of the new amputee
|
Early, uncomplicated healing
Edema control Pain reduction Protection Contracture prevention Early ambulation RL countouring |
|
|
Post op protocols
|
Soft dressings
Ace wraps Shrinkers Rigid dressings |
|
|
Removable rigid dressings
|
Allow skin eval and sock ply adjustment
|
|
|
Initial prosthesis
|
Immediate vs preparatory
Psychological benefits Independence Rapid recovery Return to work |
|
|
Transtibial post-op treatment
|
Mo 1: Soft dressing and shrinkers or temporary prosthesis
Month 1-3: fit preparatory prosthesis Mo 3-12: Wear preparatory prosthesis until residual limb size stabilizes (no socks added for 3 weeks) 8-12: Definitive prosthesis usually provided. |
|
|
Decision making for post op management
|
General physical condition
UE strength Balance Sensation Cognition In pt vs out pt Staff familiarity Familial support Funding |
|
|
Patient education
|
Positioning
Prevent contractures (hip flexion/abd, knee flexion) Residual limb care Sound side care Mobility (transfer, gait transfer) |
|
|
PT protocols
|
Desensitizing- progressive tactile stimulation
Balance Strengthening ROM Increased WB |
|
|
Goals of prosthetic management
|
Mobility and independence at varying degrees
Assistive devices help to prevent contralateral limb loss. |
|
|
Preparatory prostheses
|
Fitted when limb proximal and distal circumferences are at least equal.
Changing socket fit as the limb atrophies. Teach sock management Accomodate changing alignment. Fine tune gait. |
|
|
Year One goals
|
Residual limb stabilizes in size
Increased balance Increased strength Improved mental status More confident gait Sense of independence |
|
|
5 steps of loss
|
Denial
bargaining Anger (this is where we come in) Depression Acceptance (usually not in the 1st year) |
|
|
Post op management
|
Reinforce realistic expectations
Reinforce realistic time frames Explore patients expectations and answer questions |
|
|
Fitting problems
|
General redness
Ulceration Blisters Reported pain Discoloration of distal end |
|
|
Possible causes of fitting problems:
|
Limb volume change
Improper sock ply Shoe heel height change Need for realignment Loose suspension |
|
|
Syme amputation
|
Ankle disarticulation
Length considerations Distal end bearing Suspension Appearance |
|
|
Medicare functional levels
|
usually determined by surgeon before surgery. This is what the funding for certain componentry. The lower the K level, the less the insurance will cover.
K1- transfer K2 - low level K3- community K4- unlimited |
|
|
Outcome measures for patients w/ amputation: mobility
|
AMPPro- Amputee Mobility predictor
|
|
|
Outcome measures for patients w/ amputation: function
|
LCI5- Locomotor Capabilities Index
|
|
|
Outcome measures for patients w/ amputation: Quality of life
|
PEQ- Prosthesis Evaluation Questionnaire (mobility subscale)
|
|
|
Generic outcome measure for mobility
|
TUG- timed up and go (elderly population)
2MWT- 2 minute walk test (recommended) |
|
|
General outcome measure for function
|
FIM, Barthel (not recommended)
|
|
|
General outcome measure for QOL
|
SF-36/12- not validated in amputee population
|
|
|
AMPPro
|
For mobility
Reliable: very good Valid: poor-good Target audience: amputees w/ prostheses Responsive to change-ceiling effects: young, trauma Time to administer: 10-15 minutes |
|
|
Purposes of AMPPro
|
Predictive- assess ambulatory potential of LE amputees
Evaluative- measure function during and after rehab. Assess sitting, balance, transfers, standing balance, gait, stairs, use of assistive device |
|
|
LCI5
|
• Type of Measure: mobility
• Reliable: NA- self administered, good-excellent test-retest; excellent concurrent with 2 MWT • Valid: good content, construct • Target Audience: lower limb amputee • Responsive to change: ceiling effects-young, trauma • Time to administer:5 minutes |
|
|
LCI5 purpose
|
• Part of the Prosthetic Profile of the Amputee instrument
• 14 items • Amputee’s perceived function with prosthesis • Composite score |
|
|
PEQ
|
Type of Measure: quality of life
Target audience: amputees w/ prosthetics Takes a long time to administer |
|
|
2 minute walk test
|
Type of measure: function
Target audience: LE amputees using prosthetics |
|
|
Team approach
|
Patient and supporters
Surgeon Prosthetist PT Nurse PA |
|
|
Conventional amputation effects: medullary canal
|
Ignored and remains open.
Results in: Poor ability for end WB Venous stasis Potential for bone spur formation Regional osteopenia w/ possible adjacent joint DCD |
|
|
Conventional amputation effects on musculature
|
Majority of musculature is allowed to retract.
Results in: fatty atrophy venous stasis slower speed of contraction Poor volume of residual extremity in prosthesis. |
|
|
Conventional amputation effects: incision
|
Incisions placed over prominent surfaces, potential etiology of pain.
|
|
|
Conventional amputation effects: Circulation
|
Regional circulation disturbed.
Results in: Secondary to venous stasis. Abnormal vessel formation High risk of AVM (arterial venous malformation) Dilated, tortuous vessels |
|
|
Inactive Residual Extremity Syndrome (IRES)
|
Pain
Swelling Sense of instability Prosthetic difficulties Bone and soft tissue atrophy Fibular instability Extremity inactivity Leads to poor functional capacity w/ a prosthesis. |
|
|
Osteomyoplastic procedure goals: Osseous/soft tissue reconstruction
|
Remove bone scar/spurs
Medullary canal closure Myoplasty of opposing muscle groups Plastic closure |
|
|
Osteomyoplastic goals: stabilize the extremity
|
Create synostosis between tibia and fibula
Prevent lateral deviation of fibula Stabilize femur, preventing lateralization Muscle balancing |
|
|
Osteomyoplastic procedure goals: Provide an end WB extremity
|
Provided by bony bridge in BKA
Closure of medullary canal returns normal venous gradient; distal bone remains vascularized |
|
|
Osteomyoplastic procedure goals: create a cylindrical residual extremity
|
Improves fitting/use of prosthesis
Smooth contour aides in preventing localized skin breakdown Pressure points are reduced. |
|
|
Osteomyoplastic procedure goals: restore normal physiology
|
Venous gradient in bone returned
Vasculature improves in remaining extremity. Muscle length-tension relationship reestablished, thus restoring efficient use of the muscle |
|
|
Pain is...
|
multifactorial
|
|
|
Sources of pain:
|
bone
Muscle nerves Emotional Prosthetic |
|
|
Bone pain
|
Deep seated vs. superficial
Exostosis, fib hitting tib, etc |
|
|
Muscle pain
|
Spasm, atrophy, poor coverage
|
|
|
Nerve pain
|
Neuromas, trigger points (caused by ill fitting prosthesis), phantom vs centralized pain (N is chronically stimulated, reflex arc in CNS)
|
|
|
__% of phantoms aren't painful.
|
80-90%
Bigger trauma to the limb, the greater the likelihood they'll develop chronic pain. |
|
|
Contraindication to amputation is
|
pain, especially phantom
|
|
|
Phantom pain treatment
|
Tell them to massage the part that they feel hurts on the missing side on the opposite side.
Biofeedback- mirror box Neurontin- side effect: out of body experience, depression, taken all the time, cold turkey stop will cause rebound of phantom pain |
|
|
Painful stump
|
fibular head can become very painful due to atrophy
|
|
|
If put hand on limb and have them contract mm and hear a grind=
|
bursal inflammation around the bone
|
|
|
Pediatric patients w/ amputation may have:
|
terminal overgrowth
|
|
|
Heterotopic ossification
|
Often seen in soldiers b/c of blast effect, crush injuries, prolonged ischemia, etc.
May grow out of skin. |
|
|
Sense of instability
|
Inactive residual limb may gain excess adipose tissue and muscle atrophy causing it to be unstable.
|
|
|
Bell clapping-
|
Femur moving around in socket. Often need to restore adduction moment.
|
|
|
What can cause chronic irritation of tibial N?
|
Fibular motion occurring when compression is transmitted from socket to fibula causing scissoring of the two bones.
|
|
|
Transtibial procedure
|
Form a bridge to act as the calcaneous, but higher up.
Raise osteoperiostial flaps, suture to and put bone graft. Stabilize soft tissue, suture flaps to create a bone bridge. Do a myoplasty over the end of bone. Incision is lateral to the tibial crest. |
|
|
Transfemoral procedure
|
Resect dead bone, do the same procedure as tibial.
Restore adduction moment Bring quads over hamstrings and suture. |
|
|
Prosthetic causes of abducted gait
|
Prosthesis may be too long.
Too much abduction may have been built into prosthesis. High medial wall may cause amputee to hold prosthesis away to avoid ramus pressure. Improperly shaped lateral wall can fail to provide adequate support for the femur. Pelvic band may be positioned too far away from patient's body. |
|
|
Amputee causes of abducted gait
|
Patient may have an abduction contracture.
Defect may be due to a habit pattern. Increase in residual limb volume. Patient donned prosthesis incorrectly. |
|
|
Prosthetic causes of circumducted gait
|
Prosthesis too long
Prosthesis may have too much alignment stability or friction in the knee, making it difficult to bend the knee during swing. |
|
|
Amputee causes of circumducted gait
|
Amputee may have abduction contracture
Patient may lack confidence for flexing prosthetic knee b/c m weakness or fear of stubbing toe. Defect may be result of habit pattern. Patient donned prosthesis incorrectly. Increase in residual limb volume. |
|
|
Prosthetic causes of vaulting
|
Prosthesis too long
Inadequate socket suspension Limb discomfort |
|
|
Amputee causes of vaulting
|
Fear of stubbing toe
Limb discomfort Donned prosthesis incorrectly |
|
|
Common deviations in transtibial amputees
|
Abducted gait
Circumducted gait Vaulting Lateral bending |
|
|
Prosthetic causes of lateral bending
|
Prosthesis too short
Improperly shaped lateral wall fail to provide adequate support for femur. High medial wall may cause amputee to lean away to minimize discomfort. Prosthesis aligned in abduction may cause a wide-based gait. |
|
|
Amputee causes of lateral bending
|
Inadequate balance
Abduction contracture or glut med weakness Residual limb over sensitive and painful. Very short limb failing to provide sufficient lever arm for pelvis Habit pattern Donned prosthesis incorrectly |
|
|
Transfemoral gait deviations
|
Rotation on heel strike
Uneven arm swing Uneven step length Uneven heel rise Terminal impact Knee instability Medial or lateral whips Foot slap Drop-off at end of stance Long prosthetic step Excessive lordosis |
|
|
Prosthetic causes of rotation on heel strike
|
Too much resistance to PF
Too much toe-out built into prosthesis Socket fit too loosely |
|
|
Amputee causes of rotation on heel strike
|
Patient extends residual limb too vigorously at heel strike
Amputee has poor muscle control of residual limb |
|
|
Prosthetic causes of uneven arm swing
|
Improperly fitting socket causes limb discomfort.
|
|
|
Amputee causes of uneven arm swing
|
Poor balance
Fear and insecurity accompaied by uneven timing. Habit pattern Patient donned prosthesis incorrectly. |
|
|
Prosthetic causes of uneven step length
|
Improperly fitting socket causing pain and desire to shorten stance phase.
Weak extension aid or insufficient friction in prosthetic knee causing excessive heel rise and uneven timing b/c prolonged swing through. Alignment stability if knee buckles too early |
|
|
Amputee causes of uneven step length
|
Hip muscle weakness
Poor balance Fear and insecurity Donned prosthesis incorrectly |
|
|
Prosthetic causes of uneven heel rise
|
Knee joint has insufficient friction
Inadequate extension aid |
|
|
Amputee causes of uneven heelrise
|
Using more power than necessary to force knee into flexion.
|
|
|
Prosthetic causes of terminal impact
|
Insufficient knee friction
Knee extension aid too strong |
|
|
Amputee causes of terminal impact
|
Deliberately and forcibly extending residual limb
|
|
|
Prosthetic causes of knee instability
|
Knee joint too far ahead of TKA line
Insufficient initial flexion built into socket PF resistance too great causing knee to buckle at heel strike. Failure to limit DF leading to incomplete knee control. |
|
|
Amputee causes of knee instability
|
Hip extensor weakness
Severe hip flexion contracture |
|
|
Prosthetic causes of medial/lateral whips
|
Lateral whips from excessive IR of prosthetic knee.
Medial whip from excessive ER of prosthetic knee. Socket too tight reflecting residual limb rotation. Excessive valgus in prosthetic knee. Badly aligned toe break causing twisting on toe off. |
|
|
Amputee causes of medial/lateral whips
|
Faulty walking habits
Donning prosthesis incorrectly |
|
|
Prosthetic causes of foot slap
|
PF resistance too soft
|
|
|
Amputee causes of foot slap
|
Driving prosthesis into walking surface too forcibly
|
|
|
Prosthetic causes of drop-off at the end of stance
|
Inadequate limitation of DF
Keel of SACH-type foot too short or toe break of conventional foot too far posterior. Socket too far anterior in relation to foot |
|
|
Prosthetic causes of long prosthetic step
|
Insufficient initial flexion in socket when irreducible residual limb flexion contracture is present.
|
|
|
Prosthetic causes of excessive lordosis
|
Improperly shaped posterior wall causing forward rotation of pelvis to avoid WB on ischium
Insufficient initial flexion built into socket |
|
|
Amputee causes of excessive lordosis
|
Tight hip flexors
Weak hip extensors subbing w/ erector spinae Weak abs Habit pattern Moving shoulders backwards to obtain better balance |

