![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
13 Cards in this Set
- Front
- Back
|
Describe the structure of the ANS
|
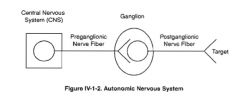
-the automatic nervous system (ANS) is responsible for the motor innervation of smooth muscle, cardiac muscle, and glands of the body
-the ANS is composed of 2 division: sympathetic and parasympathetic -in both division there are 2 neurons in the peripheral distribution of the motor innervation 1. preganglionic neuron with cell body in the CNS 2. postganglionic neurons with cell body in a ganglion in the PNS -it also consists of higher centers within the thalamus, midbrain, pons and medulla -the hypothalamus is the primary integrating center of the ANS but the beginning of many of the pathways originate in the tectum of the midbrain |
|
|
Describe the features of the sympathetic system
|
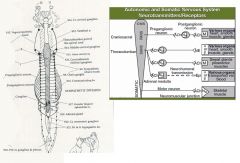
-all preganglionic neurons use acetylecholine regardless if they are parasympathetic or parasympathetic
-most postganglion nerves release norepinephrine (except sweat glands & piloerector muscles which are acted upon by acetylecholine) -the adrenal medulla releases epinephrine Preganglionic neuron: cell body in the CNS Postganglionic neuron: cell body in ganglia in peripheral nervous system sympathetic: short preganglionic, long post ganglionic (except adrenal medulla) -referred to as the thoracolumbar system, since it is this region of the spinal cord where most of the preganglionic neurons start -it is designed to aid fight or flight response in animals in situations of percieved threat or danger |
|
|
Describe the features of the parasympathetic system
|
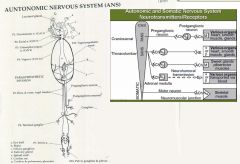
-all preganglionic neurons use acetylecholine regardless if they are parasympathetic or parasympathetic
Preganglionic neuron: cell body in the CNS Postganglionic neuron: cell body in ganglia in peripheral nervous system parasympathetic: long preganglionic, short postganglionic -it is known as the craniosacral system, since the parasympathetic preganglionic neuron cell bodies live either in the brain or sacral spinal cord gray matter -has acetylcholine (ACh) as the neurotranmitter of both the pre & postganglionic neurons -four cranial nerves: 3, 7, 9, 10 Occulomotor nerve (CN3) - ciliary & sphincter pupillae muscles to CONSTRICT the PUPIL and accommodate the lens Facial nerve (CN 7) - lacrimal, nasal, & palatine glands; madiular and salivary glands Glossopharyngeal (CN 9) - parotid & buccal salivary glands Vagus (CN 10) supplies parasympathetic innervation to the thorax and most of the abdomen (pharynx, larynx, trachea, esophagus, thoracic & abdominal organs) ●Dorsal & ventral vagal trunks - travel on the "top" and "bottom" of the esophagus ●Terminal ganglia - groups of postganglionic vagal cell bodies located in the walls of the organs innervated ●Pelvic nerves - arise from the sacral spinal cord and pass through the pelvic plexus to innervate the smooth muscle and glands of the pelvic area |
|
|
Describe the parasympathtic system control of vision
|

-the pathway for parasympathetic control of pupil size starts with the pathway for vision (CN II optic)
-approximately 20% of these fibers bypass the lateral geniculate nucleus (LGN) and synapse in the pretectal nucleus or tectum -from here the neurons then project axons back across the midline (decussation) to terminate in the parasympathetic nucleus of CNIII (aka Edinger Westphal nucleus in humans) in the midbrain -most fibers decussate twice (first at the optic chiasm and secondly after the pretectal nucleus) but a small number stay ipsilateral at each location - so that a unilateral afferent input produces a bilateral response, but the strongest stimulus for response is the ipsilateral one -from the parasympathetic nucleus of CNIII, neuron 1 (preganglionic) travels to the ciliary ganglion, located just caudal to the eye, where it synapses with the postganglionic neuon -the postganglionic neuron supplies the sphincter pupillae and ciliary muscles in the orbit. -the spincter pupillae constricts the pupil -the ciliary muscles are for accomodation and when contracted by parasympathertics relaxes the suspensory ligaments of the lends, allowing the lens to round up for near vision |
|
|
Describe the sympathtic system control of vision
|
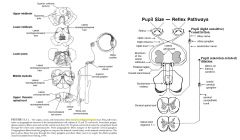
-the pathway for sympathetic control of pupil size originates in the TECTUM of the midbrain
-neurons here synapse on the second neuron in the pathway, whose cell body lives in the TEGMENTUM of the midbrain -the combination of these two neurons then forms the lateral TECTOTEGMENTOSPINAL tract which runs down the cervical spinal cord to the T1, T2, and T3 spinal cord segments, where it synapses on neuron 1 in the sympathetic system -neuron 1 (preganglionic) has its cell body within the spinal cord gray matter and sends axons down through the ventral nerve root, along the ramus communicans (ventral to the thoracic spine) and then up the vagosympathetic trunk in the neck (bypassing the stellate and caudal cervical ganglia) to synapse on neuron 2 whose cell body lives in the cranial cervical ganglion -this is located just near the tympanic bulla -neuron 2 (postganglionic) axons then project to the smooth ciliaris muscle and smooth dilator muscle of the pupil SUMMARY: The dilator pupillae muscle is innervated by preganglionic sympathetic fibers from the T1 segment of the spinal cord and by postganglionic sympathetic axons from the superior cervical ganglion -CAUSES DILATION OF THE PUPIL |
|
|
Describe the function of both the parasympathetic and sympathetic in pupil size
|
-pupil size is a balance between the parasympathetic and sympathetic nervous systems
-also a balance between the amount of light in the environment and the emotional status of the animal -the parasympathetic pathway regulates the response of the eye to environmental light -the sympathetic pathway regulates the response of the pupil to environmental factors that elicit stress (e.g. excitement, fear, anger |
|
|
Describe the lesions affecting the sympathetic supply
|
-more common
-lesions in the cervical spinal cord, thorax, neck or typanic bullae can affect sympathetic supply -the loss of sympathetic supply results in Horner's syndrome: ●Meiosis (small pupil on the affected side) ●Ptosis (drooping upper eyelid on the affected side) ●Enophthalmos (sunken eyeball, with third eyelid protrusion as a result) |
|
|
What are the signs of CNIII lesions?
|
-lesions affecting the parasympathetic branch of CN III and causing a failure of parasympathetic supply to the eye are unusual
-it is more common to see lesions that pick off the whole CN III SIGNS ●Anisocoria (unequal pupil size between the 2 eyes with a dilated pupil in the affected eye) ●Absent direct pupillary light reflex in the affected eye, but normal consensual reflex (ie. if the lesion is in the right CN III, you would see an absent PLR in the right eye when light was shone on it, but a present PLR in the left eye) ●Other signs of CNIII involvement: Strabismus (deviation of the eyeball within the orbit) and abnormal oculocephalic reflex |
|
|
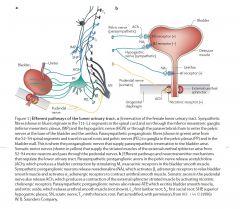
Describe the components of bladder control
|
❤AFFERENT SUPPLY
-mechanoreceptors (A-delta) in the wall of the bladder respond to stretch and distension -their axons travel in through the PELVIC nerve and enter the sacral spinal cord segments (S1-3) -cell bodies of these neurons are located in the dorsal root ganglion and the axons terminate in 1 of 3 places ●on interneurons in the dorsal horn of gray matter S1-S3 segments - these will communicate with the parasympathetic neurons in the S1-S3 segments ●on interneurons in the dorsal horn of gray matter of L1-L5 spinal cord segments - these will communicate with the sympathetic neurons in these segments ●Some collaterals travel into the dorsal column white matter of the spinal cord and ascend within the white matter, synapsing ultimately in the thalamus which then projects axons to the cerebral cortex for conscious perception of bladder filling ❤EFFERENT ●SOMATIC LMNS -provide voluntary control over straited muscle of the external sphincter -cell bodies in the ventral horn of GM S1-S3 spinal cord segments -axons travel through the ventral spinal nerve roots via the sacral plexus into the PUDENDAL NERVE to synapse on the urethral sphincter to provide voluntary contraction ●PARASYMPATHETIC -preganglionics in sacral spinal cord S1-S3 -axons travel out VIA PELVIC NERVE and are JOINED BY POSTGANGLIONIC SYMPATHETIC AXONS within the HYPOGASTRIC NERVE - together the hypogastric and pelvic nerves form the pelvic plexus -the parasympathetic axons synapse on neuronal cell bodies of post-ganglionic neurons in the PELVIC GANGLION which is located in the pelvic plexus itself -the posganglionics innervate the detrusor muscle of the wall of the bladder ●SYMPATHETIC -starts in the lateral horn of L1-L5 spinal cord segments -axons leave via ventral roots, spinal nerve, ramus communicans and terminate on the CAUDAL MESENTERIC GANGLION and synapse of postganglionic neuron cell bodies -the axons of the postganglionic cells travel out in the HYPOGASTRIC NERVE which goes to the pelvic plexus -at the pelvic plexus some nerves synapse with alpha-2 receptors on the cell bodies of postganglionic parasympathetic neurons & INHIBIT their firing, OTHERS travel to the neck of the bladder and split -at the neck some go to the internal sphincter and synapse on alpha 2 adrenoceptors on smooth muscle in this sphincter - this causes the internal sphincter to constrict, others go to the detrusor muscle and synapse on beta receptors and inhibit this muscle ❤CONTROL CENTERS -control centers for micturition live in the PONS and PONTINE RETICULAR FORMATION -they receive afferent information from the sensory neurons that travel cranially through the dorsal columns of the spinal cord -axons from the control centers travel caudally through the spinal cord to L1-5 and S1-3 to control the LMNs and autonomic nervous system -these UMNs facilitate or inhibit LMNs (including the ANS neurons) to allow for micturition when appropriate -they are also under control of the cerebral cortex and cerebellum - this allows voluntary control over the whole system, and coordination of the different parts |
|
|
Describe the control of urination
|

-the wall of the urinary bladder is composed of smooth musculature lined with an epithelial layer
-in the region surrounding the urethral opening, called the neck of the bladder, there is a thickening of the musculature, the internal uretheral sphincter -the closing of the INTERNAL SPHINCTER is due to the activity of SYMPATHETIC fibers from the lumbar region of the spinal cord -in contrast, striated muscle fibers located a little more distally in the urethra form the external urethral sphincter, which is under voluntary control -this sphincter can prevent emptying of the urinary bladder, even when the autonomic control attempts to bring about urinary discharge -in newborn and untrained animals, urination mainly occurs as a result of spinal reflex -the wall of the bladder contains stretch sensitive sensory cells that monitor the degree of filling of the bladder A, Storage reflexes. distention of bladder produces low-level bladder afferent firing which stimulates the sympathetic outflow to bladder outlet (base and urethra) and pudendal outflow to external urethral sphincter. These responses occur by spinal reflex pathways and represent “guarding reflexes,” which promote continence. Sympathetic firing also inhibits detrusor muscle. This is overseen by control centers in the pons - these send impulses through the reticulospinal tracts to facilitate lumbar sympathetic outflow and sacral GSE outflow -the control centers also inhibit the parasympathetic outflow during this phase B, Voiding reflexes. During the elimination of urine, intense bladder-afferent firing in the pelvic nerve activates spinobulbospinal reflex pathways (shown in blue) that pass through the pontine micturition centre. This stimulates the parasympathetic outflow to the bladder and to the urethral smooth muscle (shown in green) and inhibits the sympathetic and pudendal outflow to the urethral outlet (shown in red). Ascending afferent input from the spinal cord might pass through relay neurons in the periaqueductal grey (PAG) before reaching the pontine micturition centre. |
|
|
What is incontinence?
|
-leakage of urine, and the inability to urinate
|
|
|
What are the signs of a lower motor neuron bladder?
|
-a lower motor neuron bladder results from lesions in:
●sacral spinal cord segments ●sacral spinal nerves ●pelvic nerves and sacral plexus ●pudendal nerves CLINICAL SIGNS -a distended bladder with little tone, constant urine overflowing and dribbling -absent parasympathtic tone and absent LMN activity from the S1-S3 segments -prolonged distention can cause permanent atonia of the detrusor muscle due to separation of the tight junctions within the smooth muscle -treat with BETHANECOL to stimulate the parasympathetic muscarinic receptors in the detrusor muscle and PHENOXYBENZAMINE to block the sympathetic alpha receptors in the internal sphincter |
|
|
What are the signs of an upper motor neuron bladder?
|
-occurs more commonly with severe spinal cord compressive lesions
-the site of the lesion can be anywhere in the spinal cord or brainstem cranial to the S1 segment -afferent input to the pontine centers/cerebral cortex from the bladder as well as efferent control are lost -results: lack of voluntary urination, distended turgid bladder, difficult to express because of high tone in the external sphincter -may be small amounts of leakage (overflow) -over time, reflex emptying may appear (reflex between afferent neurons which inhibit sympathetic neurons and facilitate parasympathetic neurons -treatment involves PHENOXYBENZAMINE to block alpha receptors in the internal sphincter, BETHANECOL to stimulate contraction of the detrusor muscle, DIAZEPAM or DANTROLENE to relax the external (striated) sphincter |

