![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
What four tissues comprise the skeletal system? |
Bones, ligaments, tendons, and cartilage |
|
|
Define ligaments |
bands of tough, fibrous collagen and elastin that connect bones to bones |
|
|
Define tendons |
rigid cords of tissue containing mostly collagen that secure muscle to bone |
|
|
Define cartilage |
connective tissue found in many parts of the body produced by chondrocytes; acts as a cushion between the bones of joints |
|
|
What is the difference between Axial and Appendicular Skeleton? |
Axial: skull and supporting bones, vertebra and ribs, 80 bones Appendicular: limbs: 126 bones |
|
|
What is the approximate percentage of overall weight that is comprised by bones? |
~14% |
|
|
Name 5 functions of the skeletal system: |
1) support: hard framework, anchors organs 2) protection: surrounds organs such as brain, spinal cord, lungs 3) movement: provides framework for muscle attachment 4) storage: minerals (Ca and phosphorus) and some lipids are stored within bone 5) blood cell formation: occurs in the bone marrow |
|
|
What are bones primarily comprised of? What are the general properties of bone? |
Collagen protein and inorganic Hydroxyapatite Also living cells Strong yet light |
|
|
What is the general anatomy of bone? |
Compact bone is outside, whereas inside is spongy bone (lots of space occupied by bone marrow cells) and the medullary cavity (hollow space filled with yellow marrow) |
|
|
What is yellow marrow comprised of? |
Mostly fat cells and hematopoietic cells |
|
|
Bone is comprised of two things, what are they? |
Matrix and cells |
|
|
What is the matrix comprised of? |
Organic (collagen and a couple of other things) and inorganic (calcium and phosphorus) |
|
|
What is the organic matrix primarily comprised of? |
Provides strength and flexibility (~35% of adult bone mass) |
|
|
What is the inorganic portion of the matrix comprised of? |
Hydroxyapatite (an insoluble salt of calcium and phosphorus); provides stability ~65% of adult bone mass |
|
|
What are the remaining matrix components? |
Small amounts of magnesium, sodium, potassium, bicarbonate act as 'mortar' to bond Ca and phosphorus. Also, 25% of adult bone mass is attributed to water. |
|
|
The bone is also an inorganic mineral Reservoir. What minerals and how much? |
> 99% of body's calcium stored within bones and teeth; ~85% of body's phosphorus stored in bone Hydroxyapatite is Ca(10)-(PO4)(6)-(OH)2. Important to maintain calcium in diet. |
|
|
SKIP There are other bone associated proteins like Osteonectin. What role does this play? |
an acidic extracellular matrix glycoprotein that plays a vital role in bone mineralization, cell-matrix interactions, and collagen binding |
|
|
SKIP Another one is Osteocalcin. What does this do? |
Hormone that is pro-osteoblastic (bone-building); also stimulates insulin release. |
|
|
What are some common bone cells? |
Fibroblasts, osteoclasts, osteoblasts, endothelial cells, osteocytes |
|
|
What covers the outside of the bone? |
Periosteum, dividing into inner and outer layers |
|
|
What do osteoblasts and osteoclasts do? |
Osteoblasts - bone forming cells Osteoclasts - bone resorbing cells |
|
|
What are lining cells? |
They line entire surface of bone. |
|
|
What are osteocytes? |
They are mature bone cells. |
|
|
Osteoblasts are responsible for which three things in forming bone matrix cells? |
Synthesis, deposition and mineralization |
|
|
What do osteoblasts also produce? |
Enzymes and osteoid (a mixture of collagen and proteins) to which hydroxyapatite binds |
|
|
Where are osteoblasts primarily found? |
At the surfaces of mature bones. |
|
|
What are osteoblasts regulated by? |
Express hormone receptors (vitamin D, estrogen, and parathyroid hormone) |
|
|
Discuss osteoclasts in detail |
are large, multi nucleated cells that eat bone. function in self-created acidic environment share lineage with blood cells, especially macrophages mature osteoclasts form from fusion of precursors |
|
|
Besides bone eating, what are osteoclasts important for? |
blood calcium regulation |
|
|
Bone lining cells used to be what? |
Osteoblasts that have flattened |
|
|
What are bone lining cells responsible for? |
Immediate release of calcium from the bone if blood calcium is too low |
|
|
What do bone lining cells protect bone from? |
chemicals in the blood that dissolve crystals (such as pyrophosphate) |
|
|
What types of receptors do bone lining cells express? |
Express receptors for hormones and factors that initiate bone remodeling |
|
|
What main function do osteocytes serve? |
Mechanosensor cells that control the activity of osteoblasts and osteoclasts; secrete various growth factors that activate lining cells or osteoblasts |
|
|
Long branches of osteocytes allow for what? |
Intercellular contact |
|
|
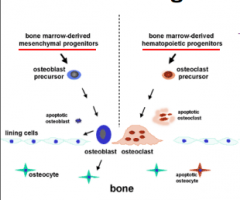
Picture of bone cell lineage |
|
|
|
Bone cells arise from which precursor cells? What are precursor cells? |
Bone marrow stem cells |
|
|
Osteoblasts and osteocytes arise from which stem cell? |
Mesenchymal stem cells |
|
|
Osteoclasts arise from which stem cells? What are these same stem cells used for? |
Hematopoietic stem cells - the same stem cells that blood cells derive from |
|
|
What type of structure does spongy bone have? |
'Spongy' honeycomb-like structure that forms the inner layer of bone tissue |
|
|
What about compact? AKA? |
AKA cortical bone, which is dense and compact, and forms the outer shaft of the bone |
|
|
Compact bone is composed of individual units called _______ which are what? |
Osteons - concentric rings of bone tissue with blood vessels and nerves in the center |
|
|
How do the concentric rings work? |
Within an osteons, collagen fibres and mineral salts align and run in opposite directions from layer to the next. There are many concentric tubes; each tube is a lamella. Having multiple layers prevents cracks from spreading |
|
|
What properties does spongy bone have? |
Lighter and less dense than compact bone. This is also bone material but interspersed with lots of spaces. |
|
|
What is spongy bone found? |
At the core of most flat and irregular bones; also at the ends of longs bones |
|
|
What is the general structure of spongy bone? |
lamellae form 'sheets' |
|
|
Spongy bone cannot handle much _____. |
Strain. |
|
|
Spongy bone contains ________. |
Red marrow. |
|
|
Spongy bone re-aligns with ________. |
Stress. |
|
|
What types of cells comprise the periosteum? |
Dense connective tissue layer cover |
|
|
Periosteum does what in addition to covering bone? |
Contains nociceptors (nerve endings) and serves as site of attachment for muscle and tendon |
|
|
What is the neonate/infant skeleton comprised of? |
Cartilage, not bone. Cartilage is produced by specialized cells called chondrocytes that make extracellular matrix composed of collagen fibers, elastin and proteoglycans. |
|
|
What happens during growth? |
Bone replaces cartilage, and bone formation outpaces bone resorption. |
|
|
How do osteoclasts eat bone? |
Secrete onto bone surface a lot of enzymes and acid which breaks down the region where they are, to be reabsorbed by the blood similar to phagocytes in a way |
|
|
Why does resorption occur at all during growth? |
Need some resorption to mobilize calcium |
|
|
Where does ossification first begin? |
In the spongy bone |
|
|
What are some growth hormone effects? |
Indirectly promotes growth by stimulating liver production of insulin-like growth factors (IGFs) - act directly on bone and soft tissues to bring about most growth-promoting actions - stimulate protein synthesis, cell division, and lengthening and thickening of bones |
|
|
Which part of long bones express receptors and for what? |
The epiphyseal growth plate of long bones express receptors for many peptide growth hormones (IGFs, FGFs, TGF-beta). the whole process is highly regulated. |
|
|
What happens during dwarfism? |
most common cause of dwarfismautosomal dominant - not sex-linked; you only need one mutation (one from both parents) - if you get just one bad copy, you're in trouble. Gly380Arg always on, what you get is premature conversion of growth plate into bone; essentially bone is created way too fast .....not given enough time to grow (premature conversion of the growth plate into bone) |
|
|
What are some ways to increase bone resorption? Decrease? |
PTH, thyroid hormone, vitamin D metabolites, cortisol calcitonin, gonadal steroids |
|
|
What are some ways to increase bone formation? Decrease? |
Growth hormone, gonadal steroids cortisol |
|
|
Where is 99% of the body's calcium located? |
In the extracellular matrix; the calcified matrix of bone |
|
|
Where is 0.1% of calcium located? |
In the ECF Acts as cement for tight junctions, role in myocardial and smooth muscle contractions, neurotransmitter release at synapses, role in excitability of neurons, cofactor in coagulation cascade |
|
|
Where is 0.9% stored? |
Intracellular, either ER or SR Acts as signal in second messenger pathways; plays a role in muscle contract |
|
|
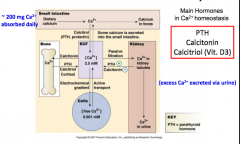
Calcium homeostasis in the blood picture |

|
|
|
Important slide on calcium balance in the body |
|
|
|
Roughly how much calcium is needed to be absorbed daily? |
200 mg |
|
|
Describe very general pathway |
Calcium > small intestine > blood or feces > blood to bone, to cells, or to kidneys > excess calcium secreted in urine |
|
|
How is calcium uptake/secretion controlled with respect to blood-bone? |
Bone calcium uptake: calcitonin bone calcium secretion to blood: PTH (parathyroid hormone), Calcitriol, Cortisol |
|
|
How is calcium uptake/secretion controlled with respect to blood-cells? |
Into cells: electrochemical gradient Into blood: active transport |
|
|
How is calcium uptake/secretion controlled with respect to blood-kidney? |
Into kidney: passive filtration Out of kidney: Increase PTH or decrease calcitonin |
|
|
What's the deal with PTH? |
Essential primary regulator of Ca. Raises free plasma Ca levels by: 1) mobilizing calcium from bone 2) enhancing renal reabsorption of Ca 3) indirectly increases intestinal absorption of calcium (facilitates activation of VitD to stimulate Ca and PO4 absorption from intestine |
|
|
What is the general calcium/PTH feedback mechanism? |
Plasma Ca decreases > signals parathyroid glands > PTH increases > Plasma Ca increases (negative feedback to parathyroid glands) |
|
|
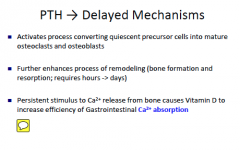
How fast acting is PTH? |
Rapid mechanism; occurs within minutes; stimulates bone resorption by pre-existing osteoclasts (which are sitting on bone waiting); inhibits collagen synthesis by osteoblasts; at kidneys, Ca reabsorption is stimulated |
|
|
Not a super important slide |
|
|
|
What is Calcitriol? |
Vitamin D3 |
|
|
How is calcitriol obtained? |
Synthesized from Vitamin D that has been obtained: a) through diet, or made in skin by the action of sunlight on precursors made from acetyl CoA |
|
|
What does calcitriol do? |
Reinforces the plasma Ca increasing effect of PTH by enhancing Ca uptake from the small intestine; also mobilizes Ca from bone and facilitates renal reabsorption of calcium |
|
|
A picture of the whole process |

|
|
|
What are the four general steps in bone healing? |
Initial inflammatory response spongy bone forms in first few days blood vessels re-grow and spongy bone hardens full healing takes 1-2 months |
|
|
Describe arthritis |
loss of cartilage; 90% of population have some osteoarthritis by age 40; over 100 forms including joint pain; chronic inflammation of joints; can be a normal age-dependent change; may also be pathological; age-related changes; decreased blood supply; trauma; loss of cartilage |
|
|
Age related atrophy - what is this? |
A decrease in bone mass, strength and bone resistance due to calcium loss |
|
|
What is the difference between osteoporosis and osteopenia? |
Osteoporosis - low bone mass and deterioration of bone tissue; Osteopenia is reduced bone mineral density |
|
|
More details on osteoporosis |
metabolic bone disorder resulting in a decline in bone density - bone resorption > bone deposition Increased risk for fracture - vertebrae, hip, wrists |
|
|
What is osteoporosis attributed to? |
genetic and environmental factors: smoking, lack of exercise; loss of muscle mass; hormonal variations. associated after menopause; reduced bone mass begins by age 30 associated with a fall in estrogen level |
|
|
What is required for healthy bones? |
large amount of calcium, phosphorus, some fluoride, magnesium, iron, manganese; vitamin A helps osteoblasts function properly; vitamin C supports manufacture of collagen and differentiation of osteoblasts into mature osteocytes; vitamins K and B12 are needed for protein synthesis |
|
|
What about vitamin D? |
Important - promotes absorption of Ca and phosphorus from intestines; essential for bone mineralization, growth and repair |
|
|
Bone therapies |
Free vascular bone graft = bone + vessels Bone auto and allografts (from self or cadavers) Bone substitutes – rather than from cadaver origin Stem cell therapies (enhance bone formation) |

