![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
73 Cards in this Set
- Front
- Back
|
Incident report AKA: Variance Report for opened medication not given. |
Report to provider and nurse manager, don't document in the medical record, disregard the medication, and file incident report. |
|
|
HIPPA violations |
Speaking about pts to other nurses in the cafeteria, elevators, restaurants, or other public areas |
|
|
False imprisonment |
Restraining a confused client |
|
|
Impetigo Not contagious if safety precautions followed |
Superficial skin infection |
|
|
Communicable diseases Contagious |
Fifths disease, chicken pox, rubella |
|
|
Noninvasive procedures |
MRI, CT scan, carotid ultrasound, |
|
|
Invasive |
Cerebral arteriogram Uses contrast material. Get written consent |
|
|
Safety for older adults |
•Set water heater to 120°F •Grab the plug when unplugging not the cord itself • use microwave or electrical toaster instead of open flame like gas stove. • Install a handrail on at least one side of stairs for decrease fall risk |
|
|
Teaching older adults |
•Allow frequent rest periods • use white or buff-colored paper with matte finish to avoid glare • present at 6th to 8th grade reading level 📚 • use 14-point font size when providing written material |
|
|
Root cause analysis |
Function of quality improvement in client care. |
|
|
Suspicions about other employees |
1. Gather data 2. Validate with another observer. 3. Take the appropriate actions to safeguard pts. Then document the incident |
|
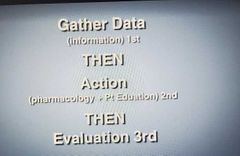
Nursing Process |

|
|
|
Negligence |
Exposed to Unreasonable risk of injury. Example: forgetting to put up side rails on bed |
|
|
Battery |
Touching a client without consent |
|
|
Intentional tort |
Intentionally injures another in some manner. |
|
|
Slander |
Injury to reputation |
|
|
Health care proxy |
Person chosen to make end of life decisions in the event pt can not speak for themselves. |
|
|
Delegation |
LPN: Can do reality orientation for a pt with STABLE but disoriented, check daily weight, check NG input and output. Tube feedings, wound irrigation , irrigate indwelling catheter, tracheostomy care if (stable or not new) no ivs or push can hang antibiotic but not administer the med. AP: Escort clients to other departments, can take blood to the lab. Cpr in cardiac arrest pts, CAN NOT check residual on gastrostomy tube, can add thickening agents to food for pts, ambulating, can do postmortem care |
|
|
Living Will |
It allows the client to express personal wishes regarding health care decisions |
|
|
End of shift report |
Include objective and measurements about the client's condition. No need to report routine care procedures or biographical information |
|
|
Beneficence |
Based on the principle that actions should be taken with the intent to do good. |
|
|
Autonomy |
Right to self determination, independence and freedom of choice |
|
|
Paternalism "Health care provider thinks they know what is best" |
Principal that one person can assume responsibility for making the decisions of another person. |
|
|
Justice |
Everyone should be treated similarly and fairly |
|
|
Nonmaleficence |
Do no harm |
|
|
Accommodation |
One person puts aside her own goals to satisfy the needs of another |
|
|
Compromise |
Both individuals give up something |
|
|
Avoidance |
Uses passive behaviors and withdrawals from a conflict |
|
|
Collaboration |
Both individuals actively try to find a solution |
|
|
Child abuse always report. |
Don't wait |
|
|
Process audit |
Measures interventions used to facilitate expected and desired outcomes in pts. |
|
|
Strategic planning |
Is part of planning process. Examines purpose, mission, philosophy and goals of an organization |
|
|
Structure audit |
Evaluation of the relationship between quality care. Environment where Healthcare is delivered |
|
|
Outcome |
Evaluates how the pt health status changed as a result of the intervention |
|
|
Autocratic Leadership "Think all about me" |
Makes decisions independently and then notifies the staff after. Autocratic manager maintains a high degree of control over the staff and allows little freedom of staff members. |
|
|
Democratic leadership "Think nice and open" encourages communication |
Guides staff toward reaching an objective and shares responsibility with the staff. Example: asks staff for there input |
|
|
Laissez-faire Leadership "Think hand off" Jerk |
Exerts little or no leadership and control. |
|
|
Transactional "Focused on tasks" |
Focuses on getting work done. |
|
|
Capital Budget |
Expenditure of money for equipment and major purchases. Example replacing cardiac monitors |
|
|
Variance analysis |
Difference between the planned budget and results of actual results |
|
|
40 watt is low wattage |
This is a safety hazard |
|
|
Declining delegation |
A float can decline tasks if she does not feel comfortable and it's a safety issue. Example: hanging blood |
|
|
Assault
|
Verbal threatening |
|
|
Case managers are for long term care |
Example: Refer stroke pts that need cared for because of neurological deficits |
|
|
Critical pathway |
A multidisciplinary tool that guides client care and bases outcomes on an externally imposed timeline |
|
|
Preparing a pt for a long term facility |
Provide a written summary of the client's nursing plan of care to the long-term facility |
|
|
Disciplinary process |
Verbal admonishment is the first step. Written is the second step |
|
|
Transformational leadership |
One who motivates employees by creating a work environment in which the goals of the leader are shared by the employees |
|
|
Fire |
Always remove pt first. |
|
|
Delegation |
Directions need to be clear: Frequency (number) what the task is, the duration ( how long), and mechanics of the action |
|
|
Restraining Forces |
Can impede change. Staff resistance can be a restraining force |
|
|
Fidelity |
Be faithful |
|
|
Informed consent Ask pt to explain the procedure that is being performed to verify the pt gave informed consent |
The person performing the procedure is legally responsible for obtaining informed consent. |
|
|
Utility |
Good of many people |
|
|
Hip arthroplasty |
Teach do not cross legs, inspect incision every 4 hrs, do not flex hip past 90° angle. Make sure to let AP know of the weight-bearing if helping to ambulate |
|
|
Authoritarian approach to managing issues |
Gives penalties to promote behavior changes |
|
|
Democratic approach |
Gives constructive feedback |
|
|
Laissez-faire |
"Suggestion box" places emphasis on group decision making |
|
|
Emergency situations think which pts will survive |
Pts with head wounds and respiratory rates of 4 are probably not going to make it. Pick pts that will make it |
|
|
Key words in delegation of tasks "Tell me" |
5 rights of delegation; provide specific information, expectations and time-frame and when to report the information back to the RN |
|
|
State nurse practice act |
Administrative laws that provide guidelines for nursing |
|
|
Patient self determination act |
Helps pts make informed decisions about care. Like end of life |
|
|
Emtala: Emergency medical treatment and active labor act |
Gives treatment regardless of financial status |
|
|
Good Samaritan |
Protects health care professionals |
|
|
Obtaining consent for surgery The nurse has the responsibility to make sure the pt has an understanding of the procedure. Have the pt repeat. If client has questions once consent is signed refer to the dr |
1. Clients can not give consent under narcotics. Get a consent from a relative If client relative is not available and surgery is critical surgery can proceed. Do not delay surgery if pt is critical |
|
|
National notifiable disease |
Varicella |
|
|
Psych Displacement " Move from dis place to dat place" |
Pt has anxiety about test result and says they have received horrible care from nurse |
|
|
Turn, cough and deep breath is priority after surgery |
TCDB |
|
|
Altruism |
Putting others first |
|
|
Mental health Dissociation |
Separates painful events from the conscious mind and describes events as if they happened to another person Example: A client who was abused as a child describes it like it happened to someone else |
|
|
Hospice nurse |
Hospice care includes bereavement services after a family members death. Teaches family how to administer medication, includes respite care also |
|
|
3 hr glucose tolerance test for pregnancy |
Fast the night before, blood samples collected every hr |
|
|
Appendicitis |
Sudden relief in pain indicates a burst appendix |

