![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
|
Describe Periosteum
|
Dense irregular connective tissue full of type I collagen,
Anchored to the bone with Sharpey's fibers A medium for MM attachment to B Break your bone and it's gonna hurt b/c periosteum is highly innervated |
|
|
Bone and cartilage sometimes look alike in a stained section, what is a good way to tell them apart?
What does this mean as far as growth? |
Bone has cells in lacunae, but just ONE, no isogenous groups.
Bone only undergoes appositional growth, (no interstitial) |
|
|
What is endosteum?
|
a simple layer of bone-lining stem cells
|
|
|
Describe how endosteum controls bone resporption and repair.
|
No need for sharpey's fibers, Bone liniing cells cover every surface of all the trabecular bone. If they retract it exposes
bone mineral and osteoclasts are formed. This directs the resorption of bone. Has Stem cells for bone repair. |
|
|
Two classifications of bones
|
1: Woven then lamellar
2: cortical and trabecular |
|
|
What is the difference in woven or llamellar bone (what is the basis of the first classification?
|
The basis is how the collagen is laid down.
Woven: first to form in fetal development and bone repair Irregular bundles of collagen, less calcified, replaced Lamellar: Replaces woven, Orderly arrnagement of collage into lamellae, More calcified= stronger |
|
|
What is the difference in the Trabecular or Compact bone (what is the basis of the second classification?)
|
2nd is a macroscopic classification of bone
Trabecular: cancellous, spongy bone Compact: Dense/cortical bone |
|
|
What is the distribution of compact and lamellar bone?
|
Trabecular is prominent at epipyses at ends of bone. Trabeculae directed down into the cortical bone in directions to distribute the force uniformly
|
|
|
What is the basic structural unit and organization of compact bone?
|
Osteon
Central canal (haversion) lined by endosteum Lamellae Lacunae (w/cells) Canaliculi that connect central canal to lacunae The whole thing is wrapped up by a nice cement line |
|
|
What canals run parallel with the bone shaft? Perpendicular?
|
Parallel: central canals
Perp: Volkman's (travel from the inside out |
|
|
How can you tell the difference between Osteoblasts, osteocytes, and Osteoclasts in a slide?
|
Osteocytes are IN the bone, easy
Osteoblasts are lining the bone and have ONE nucleus Osteoclasts are lining the bone and have MULTIPLE Nuclei |
|
|
Where are osteoprogenitor stem cells located?
|
Found in periosteum and endosteum
|
|
|
What is measured in blood to evaluate bone formation?
|
Osteocalcin and Alkaline Phosphatase
|
|
|
Osteoblasts talk to eachother via__? Addition of calcium phosphate around the Osteoblasts they will become?
|
Talk with gap junctions
Adding CaPO4 + surround themselves with bone ECM to become osteocytes |
|
|
What is the nature of osteocytes?
|
They are amitotic b/c can't go anywhere/ Communicate via canaliculi, they maintain the ECM and can mobilize Ca
|
|
|
What is the purpose of the canaliculi?
|
Source of gap junction and diffusion. In lecture she added that blood vessel in central canal out through this system of canaliculi. NEVER contain BVs
|
|
|
What is a disorder of Type I collagen?
|
Osteogenesis imperfecta, Affects all bones in the body.
Demineralized bones because type I collagen and its arrangement contributes to the minearlization of bone. |
|
|
What do Matrix vessicles contain, from where do they come, what do they do?
|
Matrix vessicles contain Alkaline phosphatase, Ca++ and PO4. THey are in the osteoblast, Vessicles act as seeding areas that promotes a nice set-down of mineral that will thoroughly mineralize collagen.
|
|
|
Osteoblasts lay down _____ which in time will become ____.
|
Osteoid,
Mineralized bone after mineralization guided by Matrix vessicles. |
|
|
Child vs adult Vitamin D Deficiency
|
CHild: larger osteoid seam, rickets, greater lag time, not enough Ca++ to mineralize the osteoid
Adult: Osteomalacia |
|
|
Osteoclasts are derived from?
|
bone marrow precursor cells Granulocyte/Monocyte progenitors (not osteoprogenitor cellsd) of myeloid lineage, they fuze into a big blob.
|
|
|
As osteoclasts eat through bone it forms what is called """ or """
|
Ruffled border,
Howship's lacuna |
|
|
How does Osteoclast resorb bone?
|
Golgi pumps out tons of immiture lysosomes, which bind to membrane and cause it to rufffle, it also causes subosteoclast compartment to be acidic.
There is an actin plaque filament donut that seals off the ruffled border. Bone resorbs and sends ot nearby capillary . Note: no capillary, no resorption, defective actin= defective osteoclast |
|
|
What are the three things Osteoblasts secrete to affect Osteoclasts.?
Whats another effector not from Osteoblasts (2)? |
M-CSF
RANKL OPG (PTH from parathyroid) RANKL from T lymphocytes |
|
|
What does M-CSF do, where is its source?
|
from Osteoblasts
1-stimulates precursor osteoclast formation and 2-induces them to make RANK and then express at their surface. |
|
|
What does RANKL do, where is its source?
|
from Osteoblasts
1- binds to RANK receptor on Osteoclasts inducing further differentiation into Osteoclasts such as fusing with other precursors, etc. |
|
|
Essentially what's the difference in M-CSF and RankL?
|
MCSF- increase in cell numbers with receptors
Rank L- increase activated cells/cell activation |
|
|
What is PTH's effect on Osteoclast cells? How?
|
PTH from chief cells of the parathyroid. Acts on osteoBLasts to increase MCSF and RANKL
secretion to lead to osteoclast differentiation. it "activates the cascade" |
|
|
Explain how inflammation can increase bone resorption
|
Activated t lymphocytes during inflammation secrete RANKL and increased osteoclast activity to increase bone resorption (increased Ca++ demand on the body)
|
|
|
What is OPGs effect on Osteoclast activity? How?
|
from osteoblast
Osteoprotegerin acts as a decoy receptor for RANKL ; so less RANKL available to bind to real RANK on osteoclast precursor cells, OPG inhibits cascade Both RANKL and OPG from osteoblasts |
|
|
WHat does Calcitonin do to Osteoclast activity?
From where does it come? |
Shuts down by binding to calcitonin receptors.
from C Cells. THis is the FASTER response to shut down osteoclasts |
|
|
What happens when normal bone remodeling pattern becomes uncoupled?
|
Bone remodeling: osteoclast and osteoblast reformation of bone.
Decreased bone density |
|
|
What is the primary form of osteoporosis?
|
Osteoclasts work perfectly normal but osteoblasts don't make enough bone.
|
|
|
What are secondary forms of osteoporosis?
|
Hyperparathyroidism and
Steroids |
|
|
What are the three elements needed for fracture healing?
|
Approximation of fractured segments
Limited movement of bone fragments through stabilization and immobilization and Most importantly Intact periosteum and endosteum |
|
|
What is a risk in fragment stabilization and immobilization?
|
Too much stabilization vs weakening of supporting tissues
|
|
|
Why is Intact periosteum/endosteum the most important requirement for fracture repair?
|
it is the source of stem cells and blood supply.
IF no periosteum available due to nature of fracture may cause healing problems. Endosteal side will heal quicker b/c of availability of regeneration factors |
|
|
Stem cells in the periosteum/endosteum can become three different "blasts" depending on oxygen levels. What are they?
|
Low O2= fibroblast
Mid O2= Chondroblast High O2= Osteoblast Blood= O2 nutrtition, hormones, GFs, etc= better stem cell attraction and differentiation. |
|
|
Explain what happens at initial fracture of the bone
|
Bleeding=clot
BVs shut down on either side of fracture = more death "Tissue dies in either side of the fracture as a result of the fracture itself. Area of damaged tissue is greater than just the actual site of damage. Endosteum is usually less affected. |
|
|
After break what is the order of tissue as vasculature improves?
|
Fibroblasts- granulation tissue in really low O2 environ
Chondroblasts as Medium O2 levels. Cartilage replaced with bone as vascularity continues to improve. |
|
|
What are the four major parts of the long bone?
|
Epiphyses- ends
Diaphysis- includes everything other than the epiphysis Epiphyseal plates- located between the epiphysis and the metaphyses Metaphyses- where it flares out. |
|
|
Where is the bone marrow cavity?
|
in the diaphysis between the trabecular bone ends, surrounded by cortical bone.
|
|
|
Explain blood supply to Epiphysis and metaphysis in child vs adult.
|
As long as there is cartilage between epi and metaphysis there is very little anastamoses
that occur. Yound individuals will NOT have anastamoses. Adults may, depends. |
|
|
What is intramembranous ossification?
|
Bone formed directly by stem cells, no cartilage structure first.
Plates of skull formed this way. Directly from mesenchyme in a highly vascular environment NOTE: Fracture repair can have a component of intramembranous ossification |
|
|
In limb bud formation all of the vasculaature originates in the periphery of the limb, this promotes what growth in the center? Then what?
|
This promotes chondroblast formation- a cartilage bone model.
Then, as vasculature becomes increasingly dense a Perichondrium forms around the cartilage model Around the same time central chondroblasts calcify the matrix (not bone, just calcified chondroblasts CaCO3 crystals) and die. |
|
|
After the CaCO3 skeleton of part of a bone's cartilage model what happens?
|
Perichondrium now changes name to periosteum (8th week) and primary ossification centers have begun to grow.
|
|
|
What are required to say that a bone has "growth plates"?
|
you must have a primary and secondary center of ossification
|
|
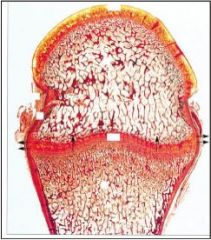
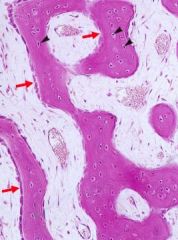
identify the arrows
|
Secondary centers of ossification
|
|
Identify the bony structure
|
Bony collar
|
|
Identify the center of the structure
|
CaCO3 chondrocyte skeleton ready for primary growth to occur
|
|
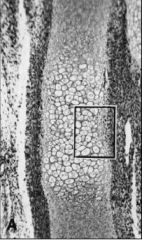
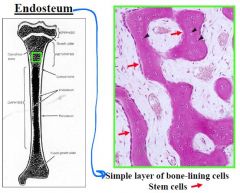
Arrows are pointing to what type of tissue?
|
Endosteum
|
|
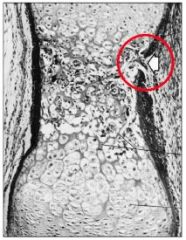
What are the arrows pointing to?
|
|
|

What is identified here?
|
Fractures at the epiphyseal plates cause bony bridges Ostosis and uneven growth of long bones
|
|

What is shown in this image?
|
Osteoclasts and Howship's lacunae
|
|

type of bone formation?
|
Intramembranous ossification
|
|
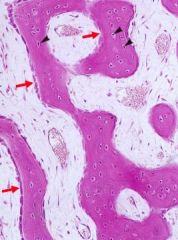
What cells are these?
|
Osteoblasts
|
|

Identify these cells
|
Osteoblasts
Osteocytes Osteoclasts (multinucleated |
|
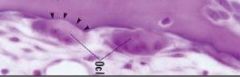
Identify these cells
|
Osteoclasts with ruffle border
|
|
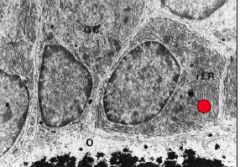
What is this?
|
Osteocyte with cannaliculi
|
|

What is this diagnosis?
|
Osteogenesis imperfecta
|
|
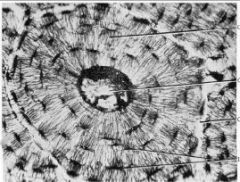
Label these
|
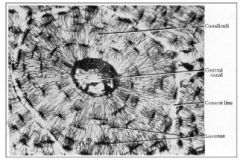
|
|

Diagnosis
|
Osteoporosis
|
|

Identify
|
Primary center of ossification
|
|
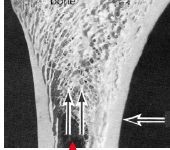
These arrows are pointing at what?
|
Inside= trabecular
outside= compact or cortical |
|
identify types of bone
|
Cortical or compact
trabecular |
|
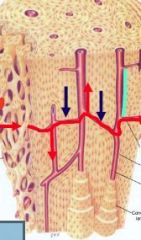
Identify red and blue
|
Red= volkmans in and out
Blue= central canal up and down |

