![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
ROME Criteria for IBS |
Recurrent abdominal pain or discomfort at least 3 days per month in the previous 3 months associated with two or more of the following:
|
|
|
Alarms symptoms prompting consideration of alternative Dx than IBS: |
onset of symptoms after age 50 unintentional weight loss anorexia bloody stools nocturnal diarrhea family history of significant colon disease |
|
|
Alternative DX to consider in patients with IBS patterns of symptoms |
Constipation—Predominant
Other Emergency Pancreatitis Hepatitis Biliary Colic Urological Disorders - (e.g. urolithiasis) |
|
|
Diverticulosis |
Presence of diverticuli in the colon |
|
|
Diverticulitis - Simple - Complicated |
Simple/Uncomplicated: Inflammation of diverticular tissue restricted to the pericolonic fat
Complicated: More extensive disease characterized by: - abscess - peritonitis - intestinal obstruction - fistula formation |
|
|
Diverticula |
Herniation of the colonic mucosa through the insteninal wall at the the vasa recta |
|
|
Oral Antibiotic therapy for uncomplicated diverticulitis |
• Trimethoprim-sulfamethoxazole, one double-strength tablet bid, and metronidazole 500 mg q6h or
All oral regimens should be taken for 7 to 10 days |
|
|
IV Antibiotic coverage for complicated/severe diverticulitis |
Mild to Moderate Infection
|
|
|
Indications for hospital admission in uncomplicated diverticulitis |
significant comorbid illness including inability to tolerate oral liquids poor social support inability to comply with follow-up in a reasonable time frame (2 to 3 days) |
|
|
Causes of Large Bowel Obstruction |
Malignancy/Tumor Volvulus Diverticular disease Fecal Impaction Strictures (due to inflammation) Adhesions Hernia |
|
|
Olgive's Syndrome |
massive colonic distension in the absence of mechanical obstruction
Thought to be due to impaired auntonomic nervous system control of gut motility |
|
|
Coffee Bean Sign
|
Sigmoid volvulus
|
|
|
ED Priorities for patients with IBD |
(1) recognize new cases of IBD (2) exclude complications in patients with IBD (3) identify IBD patients who need admission |
|
|
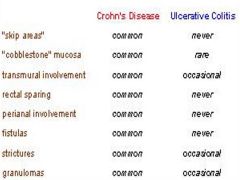
Differentiating Features of Crohn's Disease versus Ulcerative Colitis |
|
|
|
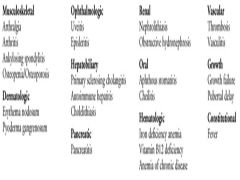
Extraintestinal Manifestations of IBD |
|
|
|
Complications of IBD |
Common -fistulae -strictures -abscesses
Life threatining - fulminant colitis - toxic megacolon - intestinal perforation |
|
|
Toxic megacolon |
pathologic dilation of the colon resulting from inflammation of the smooth muscle layers of the intestine
Leads to paralysis, dilation, and eventually perforation if left untreated
Hallmark: colonic dilation in a patient with a known inflammatory condition of the colon who appears systemically toxic |
|
|
Potential pharmacological triggers for toxic megacolon in patients with underlying IBD/colitis |
anticholinergics antimotility agents narcotics antidepressants |
|
|
Medications used in the treatment of IBD |
5-Aminosalicylic Acid Agents
|
|
|
Disease severity criteria in Ulcerative colitis |
Mild Disease
|
|
|
Disease severity criteria in Crohn's disease |
Mild to Moderate Disease
|
|
|
Pathophysiology of colonic ischemia |
Combination of non-occlusive microvacular disease and low flow states/vasoconstriction |
|
|
Imaging sign suggesting colonic ischemia |
Thumbprinting |
|
|
Management of colonic ischemia |
Primarily supportive
Bowel rest IV hydration Analgesics +/- Antibiotics dependent on severeity
Correct Precipitants Avoid vasopressors and corticosteroids Decompression
Surgical consultation if signs perforation/necrosis |
|
|
Pathophysiology of acute and chronic radiation proctocolitis |
Acute: Ulceration and inlammation or radiation induced damage to colonic mucosa
Chronic: Endarteritis leading to ischemia and ulceration |
|
|
Mainfestations of acute radiation protocolitis |
Abdominal pain Bleeding Tenesmus Incontinence
Arises during acute pelvic radiation |
|
|
Manifestations of chronic radiation proctocolitis |
Insidious onset with protean manifestations:
- ulcerative disease - stricture with or without obstruction - fistulae - bowel perforation |

